Medium long-term follow-up outcomes of BalMedic® bovine pericardial bioprosthetic valve in the mitral position
Introduction
Conventionally, mechanical valves are more durable than bioprostheses; however, patients with mechanical valves require lifelong anticoagulants, and may experience related complications. Research has shown that life expectancy after valve replacement procedures is almost identical regardless of whether mechanical valves or bioprostheses have been used (1-3). However, younger patients prefer mechanical valves to avoid having to undergo a second operation, and accept that they will need to take anticoagulant drugs, which is a treatment that can be difficult to control, well after their operations, and will require constant hospital care.
With its extended valve-in-valve application, the transcatheter heart valve (THV) has fundamentally changed the habitual thought. With the THV, a new valve can be implanted and anchored on a previous dysfunctional valve via an interventional route. Patients with THVs do not need to undergo a second surgery, which is an obvious weakness that arises when tissue valves are used. More importantly, patients do not require lifelong anticoagulants after the surgery, which substantially improves their quality of life.
Large amounts of clinical data from the United States and Europe have shown that tissue valves perform well (4-6). With the development of tissue treatment techniques and accumulated clinical data, tissue valves are now being used in younger patients. Under the 2017 American College of Cardiology and the American Heart Association (ACC-AHA) guidelines and the 2015 European Society of Cardiology (ESC) uidelines for cardiac surgery (7), the age for tissue valve replacement for patients has been lowered to 50 years for the first time.
The incidence of rheumatic heart disease is high in China, especially in rural areas (8). This disease mainly leads to the dysfunction of the mitral valve, which needs to be replaced due to stenosis or/and regurgitation. Most patients with rheumatic heart disease who require valve replacements are middle aged (commonly in their 50s), and are younger than patients with degenerative heart disease. It leads to bigger challenge for the anti-calcification and durability features of implanted valves.
The application of tissue valves is irreversibly globally; however, mechanical valves still represent a large share of the market in China. The lack of long-term clinical follow-up data, especially data post the 10-year follow-up period, which are rarely officially reported, is a serious concern for many surgeons who would like to use tissue valves. This article examines the 10-year follow-up results of Chinese patients with domestic artificial heart valves in the mitral position.
The implanted bioprostheses were from Beijing Balance Medical Tech Co., Ltd., the first tissue valve manufacturer in China. With their unique, patented anti-calcification technology, balance bovine pericardial materials have also been used in congenital heart disease treatments and other surgical implantation operations. These tissue valve products, which were approved by the China Food and Drug Administration (CFDA) in 2003, have been used over 400 hospitals in China. The 2 hospitals involved in this study are both earlier users, who first started using these bioprostheses in 2005.
Compared with other published data on overall valves replacement performance, this paper focuses on mitral valve from the two hospitals. Mitral valve diseases are more prevalent and serious in China, so multi-center statistics results from different parts of the country are more meaningful.
Follow-up clinical data were collected from the 2 cardiac centres, and the performance of the valves in the mitral position were evaluated. This has been the largest group follow-up study thus far for a domestic Chinese product. The results provide a foundation for the clinical validation of the valve product.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-21-734).
Methods
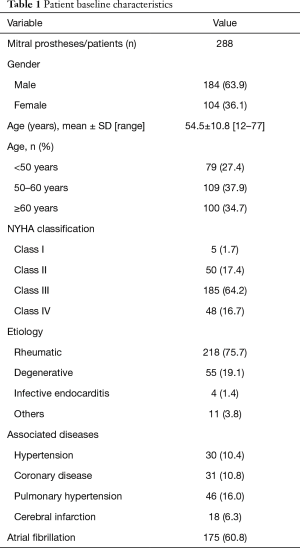
The implanted products had been granted premarket approval from the CFDA. This study was reviewed and approved by the Ethics Committees of The First People’s Hospital of Yulin, and The Affiliated Hospital of Qingdao University. All data collection was supported and approved by the ethics committees of these two hospitals and informed consent was taken from all the patients. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). From 2005 to 2015, 288 patients were provided with replacement BalMedic bovine pericardial bioprosthetic valves in the mitral position. Table 1 sets out the background characteristics of the patients, including their sex, age, complications, etiology, and preoperative cardiac New York Heart Association (NYHA) classification. Patients’ overall survival (OS), reoperation-free, and structural valve deterioration (SVD)-free rates were analyzed statistically. The results reflected the dysfunction ratio of the implanted valves at different post-implantation periods. Most patients made an appointment on the telephone to attend the same hospital at which they underwent surgery for their follow-up visits; however, some patients attended local hospitals that provided reports. All of the surviving patients underwent electrocardiogram (ECG) and echocardiography. The mean age of the patients was 54.5±10.8 years, and the average follow-up period was 7.2±2.6 years. To reflect the diversity of patients’ ages, the patients were divided into the following 3 age groups: the <50 age group, the 50-60 age group, and the ≥60 age group. The results for each group were analyzed and compared.
Full table
Statistical analysis
Mortality and the reoperation rate were used to determine the comprehensive treatment effect. In addition, the SVD rate provided information about valve durability based on whether the valves continued to work in patients’ bodies. Less serious than reoperation, SVD was defined as a valve open/closure disturbance due to a dysfunction, such as calcification, tearing, or degenerative changes. Function failure from infection or thrombosis was not included. Following the echocardiography inspection, all SVD cases were diagnosed during the follow-up period. The results for other valve-related complications, such as hemorrhage, embolism, infective endocarditis, and nonstructural valve dysfunction (e.g., paravalvular leakage), will be presented in later publications.
The Kaplan-Meier (K-M) method and a log-rank test analysis were used to calculate the estimated rates of freedom from any event. The overall results are expressed as pooled untransformed proportions (i.e., hazard ratios) with 95% confidence intervals. Continuous variables were expressed as mean ± standard deviation (SD). Categorical variables were analyzed using a chi-squared or Fisher’s exact test. A P value <0.05 was considered statistically significant. R software (version 4.0.2) was used for the computations and statistical analysis.
Results
Over 300 patients underwent BalMedic bovine pericardial bioprosthetic valve replacements in the mitral position (not including patients who underwent double valve replacements) at the 2 hospitals during the period set for this study. Table 1 sets out general information about the 288 discharged patients who were included in this study. In relation to the age groups, most patients were in the younger age group (54.5±10.8). Specifically, there were 79 (27.4%) patients in the <50 age group, 109 (37.9%) in the 50–60 age group, and 100 (34.7%) in the ≥60 age group. Of the patients, 75.7% suffered from rheumatic heart disease, which is the local high incidence heart disease. Degenerative valve sufferers only accounted for 19.1% of the patients. Before surgery, 80.91% of the patients were classified as NYHA functional class III or IV. Patients presented with a number of associated diseases, including hypertension (10.4%), coronary disease (10.8%), pulmonary hypertension (16.0%), cerebral infarction (6.3%). Of the patients, 175 (60.8%) were diagnosed with atrial fibrillation before the valve replacement.
Postoperative mortality
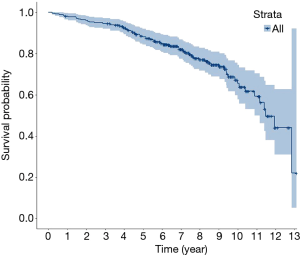
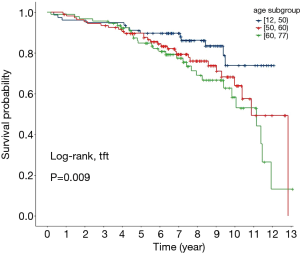
The early (in-hospital) mortality rate was not considered in the statistical analysis due to incomplete data. A total of 288 patients survived to discharge. During the follow-up period, 72 patients died. Thus, the overall 10-year survival rate was 65.6%. Figure 1 shows the OS K-M curves. Figure 2 shows the OS rate for each age group. Patients aged <50 had the highest OS rate of 74%, patients in the 50–60 age group had an OS of 64.1%, and patients in the ≥60 age group had the lowest OS rate of 58.4%. The bioprosthetic valve calcified more easily in younger patients than older patients. The results showed that NYHA calcification did not lead to a higher mortality rate. Due to the average life expectancy, the 10-year survival rate was low in elderly patients, especially if their cardiac functions were poor before the valve replacement.
Second surgery
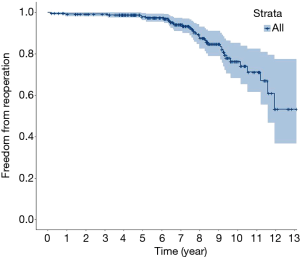
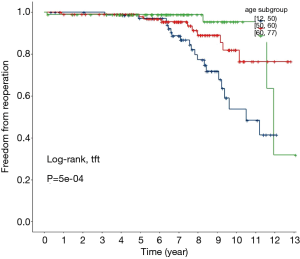
The phrase “second surgery” refers to any valve replacement reoperation for which a dysfunction of a valve in an alive patient led to a second replacement surgery. The 10-year reoperation-free rate was 76.3%. Figure 3 shows the overall variation K-M curve. Figure 4 shows the reoperation-free rate for each age group. The ≥60 age group achieved better reoperation-free rates than the other two groups. Specifically, 95.5%, 82%, and 53.7% of patients did not require a second surgery during the follow-up period in the ≥60 age group, the 50–60 age group, and the <50 age groups, respectively. The results showed that valve dysfunction occurred more frequent in younger patients, but the progression was slow, and most patients had a chance to undergo a second surgery, or would undergo valve-in-valve percutaneous surgery in the near future.
SVD
As stated above, SVD reflects the overall effect of postoperative events that may cause valve failure. In such cases, valves do not always need to be replaced instantly; however, generally, valve failure leads to a second surgery. The diagnostic criteria for SVD of the mitral valve in this study were as follows: moderate to severe regurgitation, a mean transvalvular pressure of >8 mmHg or a maximum transvalvular pressure >25 mmHg, or a peak flow of >2.5 m/s. These criteria have been adopted in many follow-up studies and are well accepted (9-11).
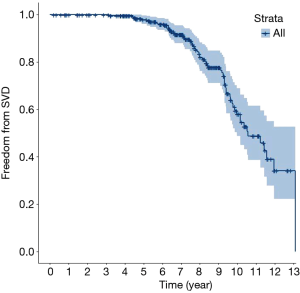
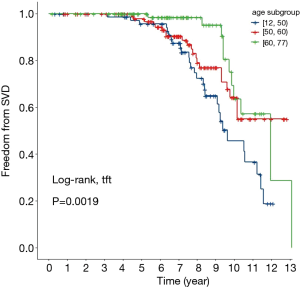
Figure 5 shows the overall SVD-free rates. The 10-year SVD-free rate was 58.0%. The trend for the SVD rate was similar to that of the reoperation-free rate; that is, the SVD-free rate in elderly patients was higher than in the other groups. Specifically, the SVD-free rate was 63.6% in the ≥60 age group, and 64.2% in the 50–60 age group. Less than half (45.7%) of patients in the younger age group (i.e., the <50 age group) were free of SVD. The higher incidence of SVD is consistent with the higher metabolism level of younger patients. Further, as stated, SVD led to a high incidence of reoperation among younger patients. Figure 6 shows the SVD-free rate in different age groups.
Discussion
There have been rapid developments in transcatheter valves in recent years. Like surgical tissue valves, the leaflets of transcatheter valves are also made of animal tissue, such as bovine/porcine pericardium or porcine aortic valves, which are treated with chemical techniques. Generally, there are two type of biological valves based on the leaflet materials, Bovine Pericardium and Porcine Aortic Valve respectively. Although some other animal tissues were also used to be applied, no others get into widely marketing use as the above two. Globally, there are over 700,000 biological valves implanted into human patients, who are suffered from irreversible native heart valve diseases. The replacement can restore the heart valve function and effectively extend the patients’ life. Clinically, the prognostic factors of heart valve disease include two aspects, stenosis and regurgitation. If the level of stenosis or regurgitation was diagnosed above medium, which has clinical standard, valve replacement surgery may need to be considered.
The continuation treatment of a dysfunctional surgical valve through transcatheter implantation is called a valve-in-valve. However, as this procedure can only be realized for tissue valves, the use of mechanical valves ceased. This trend settled the concern that bioprostheses are less durable than mechanical valves. The other obvious advantage of bioprothese is avoiding post-surgery anti-coagulant, which is very annoying for the patients. Patients accepted replacement mechanical valve, whose leaflets are made of rigid materials, have to inevitably take anti-coagulant medicine for whole life long time. The valve selection is becoming more and more tendentious. Through Clinical follow-up data comparison, bovine pericardium valve has gradually become golden standard of artificial heart valve leaflet material, although porcine valve still has a certain market share. In relation to tissue valves, regardless of whether they are implanted through surgery or transcatheter, the key issue remains the durability of the leaflets. Leaflet anti-calcification has always been the main problem of tissue valve durability. Each manufacturer has its own technique for tissue treatment, which are mainly directed at anti-calcification.
The metabolism level of the human body is one of the most important factors that leads to different levels of calcification (12). It has been found that tissue valves calcify more quickly in younger patients, who suffered more from rteumatic heart disease (13). Presently, the minimum age for tissue valve implantation is 50 years old. Before bioprostheses can be used more widely among younger patients in China, more clinical evidence needs to be gathered. The other feature of rheumatic heart disease is mitral valve dysfunction.
Glutaraldehyde treatment on bovine pericardium is common in the field. This treatment strengthens the animal tissue using a crosslinking process at the fibre level. However, it also has a negative effect, which enables the material to calcify more easily. The application of a coordination compound solves both issues. This innovative process is used in the BalMedic bovine pericardial valves (Beijing Balance Medical Tech Co., Ltd.). Thus, the leaflet is more durable in terms of mechanical deformations, and there is also a lower risk of calcification. The typical and most urgent operation requirement is for the treatment of congenital heart disease patients (14,15). Other patch productions for different surgical operations are being considered.
This study focused on a special patient group. Specifically, all replacements were in the mitral position, patients with rheumatic heart disease comprised three-quarters of all patients, and patients were younger in age compared to degenerative sufferers. Thus, the results largely reflect anti-calcification effects in young patients.
The two hospitals in the study are located thousands of kilometers apart from each other in the south and north of China. The selection of tissue valves was not related to the background (or etiology) of each patient. The overall enrollment period for this study was over 10 years. Similar to the results of other studies (16), the results showed the main reason for valve replacement in this group was rheumatic heart disease. In the present study, the typical and special characteristic of patients before the surgery was that their cardiac function was much worse than that of most patients in the Western follow-up group in which over 80% of patients were classified as NYHA class III/IV (17,18). The mean age of patients was 54.5±10.8 years, which was younger than that of Western patients by 5–10 years (9-11). The 10-year OS rate was 65.6%. This figure is not inferior to any typical mitral valve follow-up figure (10,19)). Considering the background of the younger patients, the patented anti-calcification treatment played its due role. In the <50 age group, the 10-year OS rate was up to 74%. The reoperation-free and SVD-free rates of the younger patient group were lower than those of the older patient groups. However, as mentioned above, valve dysfunction could be fixed through a valve-in-valve procedure. The first surgical valve can also serve as an anchor, which is the most difficult issue in transcatheter mitral valve surgery.
For young Chinese valve disease patients, especially mitral sufferers, a more durable surgical valve represents the best choice for their first treatment. Mechanical valves can cause anticoagulant complications and do not allow a valve-in-valve to be used in any follow-up treatment. In the mitral position, the anchor represents a significant challenge for the transcatheter valve and perivalvular leakage. The overall results of this study showed that this is a promising valve for such patients; however, longer-term clinical follow-up statistics should be considered.
Due to the complexity of mitral valve replacement, other complications, such as hemorrhage, embolism, infective endocarditis, and nonstructural valve dysfunction (such as paravalvular leakage), should also be considered. Some other centres have gathered similar clinical data. We will collect these data and examine a larger patient group and longer-term follow-up results in the future. All follow-up reports will provide a clinical foundation for valve implantations in Chinese patients.
Limitations
To avoid single-centre deviation, data from two hospitals in the north and the south of China were collected for this study. However, the data were still too limited to reflect the whole picture of such a big country as well as the performance of the bioprotheses. Additionally, as this was a retrospective study, potential data and recall biases must be considered. The maximum follow-up time was 14 years (7.23±2.60 years); however, this period is not sufficiently long to reflect the tissue prosthesis performance of younger patients. The 20–25-year follow-up results are necessary if foreign counterparts are to be compared. In the age group analysis, we did not propose any hypothesis or predefined measures, and the patient numbers in the different age groups were too low to examine differences in valve performance.
The patient groups are still being followed. We will publish more data and draw comparisons with other products. We are also interested in comparisons between tissue and mechanical valves, especially in the same implantation period. The results will be more persuasive for younger patients who are hesitant about valve type selection.
Conclusions
BalMedic valves have been widely used in clinical practice for over 18 years. In total, over 15,000 bioprosthetic valves have been implanted, about two thirds of which were implanted in the mitral position. In this first medium long-term follow-up study of a large patient group, the product was shown to have durable performance in Chinese patients with poor cardiac preconditions. In this study, younger patients had higher survival rates, while older patients had higher reoperation-free and SVD-free rates.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-21-734
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-21-734
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-21-734). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work, including ensuring that questions related to the accuracy or integrity of any part of the work have been appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and the Harmonized Tripartite Guideline for Good Clinical Practice from the International Conference on Harmonization. This study was reviewed and approved by the Ethics Committees of The First People’s Hospital of Yulin, and The Affiliated Hospital of Qingdao University. The tissue valves implanted had been granted premarket approval from the CFDA. Informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sidhu P, Okane H, Ali N, et al. Mechanical or bioprosthetic valves in the elderly: a 20-year comparison. Ann Thorac Surg 2001;71:S257-60. [Crossref] [PubMed]
- Holper K, Wottke M, Lewe T, et al. Bioprosthetic and mechanical valves in the elderly: benefits and risks. Ann Thorac Surg 1995;60:S443-6. [Crossref] [PubMed]
- Chikwe J, Chiang YP, Egorova NN, et al. Survival and Outcomes Following Bioprosthetic vs Mechanical Mitral Valve Replacement in Patients Aged 50 to 69 Years. JAMA 2015;313:1435-42. [Crossref] [PubMed]
- Bourguignon T, Bouquiaux-Stablo AL, Loardi C, et al. Very late outcomes for mitral valve replacement with the Carpentier-Edwards pericardial bioprosthesis: 25-year follow-up of 450 implantations. J Thorac Cardiovasc Surg 2014;148:2004-2011.e1. [Crossref] [PubMed]
- Bourguignon T, Espitalier F, Pantaleon C, et al. Bioprosthetic mitral valve replacement in patient aged 65 years or younger: long-term outcomes with the Carpentier-Edwards PERIMOUNT pericardial valve. Eur J Cardiothorac Surg 2018;54:302-9. [Crossref] [PubMed]
- Poirer NC, Pelletier LC, Pellerin M, et al. 15-Year Experience With the Carpentier-Edwards Pericardial Bioprosthesis. Ann Thorac Surg 1998;66:S57-61. [Crossref] [PubMed]
- Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2017;38:2739-91. [Crossref] [PubMed]
- Han QQ, Xu ZY, Zhang BR, et al. Primary triple valve surgery for advanced rheumatic heart disease in Mainland China: a single-center experience with 871 clinical cases. Eur J Cardiothorac Surg 2007;31:845-50. [Crossref] [PubMed]
- Mykén PS, Bech-Hansen O. A 20-year experience of 1712 patients with the Biocor porcine bioprosthesis. J Thorac Cardiovasc Surg 2009;137:76-81. [Crossref] [PubMed]
- Bourguignon T, Bouquiaux-Stablo AL, Loardi C, et al. Very late outcomes for mitral valve replacement with the Carpentier-Edwards pericardial bioprosthesis: 25-year follow-up of 450 implantations. J Thorac Cardiovasc Surg 2014;148:2004-2011.e1. [Crossref] [PubMed]
- Bourguignon T, Espitalier F, Pantaleon C, et al. Bioprosthetic mitral valve replacement in patient aged 65years or younger: long-term outcomes with the Carpentier-Edwards PERIMOUNT pericardial valve. Eur J Cardiothorac Surg 2018;54:302-9. [Crossref] [PubMed]
- Vyavahare N, Ogle M, Schoen FJ, et al. Mechanisms of bioprosthetic heart valve failure: Fatigue causes collagen denaturation and glycosaminoglycan loss. J Biomed Mater Res 1999;46:44-50. [Crossref] [PubMed]
- Barnett SD, Ad N. Surgery for aortic and mitral valve disease in the United States: a trend of change in surgical practice between 1998 and 2005. J Thorac Cardiovasc Surg 2009;137:1422-9. [Crossref] [PubMed]
- Sharma A, Cote AT, Hosking MCK, et al. A Systematic Review of Infective Endocarditis in Patients With Bovine Jugular Vein Valves Compared With Other Valve Types. JACC Cardiovasc Interv 2017;10:1449-58. [Crossref] [PubMed]
- Chen H, Shi G, Qiu L, et al. Outcomes of Prosthetic Valved Conduits for Right Ventricular Outflow Tract Reconstruction. Pediatr Cardiol 2019;40:848-56. [Crossref] [PubMed]
- Guo H, Lu C, Huang H, et al. Long-Term Clinical Outcomes of the Carpentier-Edwards Perimount Pericardial Bioprosthesis in Chinese Patients with Single or Multiple Valve Replacement in Aortic, Mitral, or Tricuspid Positions. Cardiology 2017;138:97-106. [Crossref] [PubMed]
- Thierry L T, Andre V, Georges F, et al. Ten-Year Echocardiographic and Chinical Follow-Up of Aortic Carpentier-Edwards Pericardial and Supraannular Prosthesis: A Case-Match Study. Ann Thorac Surg 2002;74:2010-5. [Crossref] [PubMed]
- Wang M, Furnary AP, Grunkemeier GL, et al. Bioprosthetic Aortic valve Durability: A Meta-Regression of Published Studies. Ann Thorac Surg 2017;104:1080-7. [Crossref] [PubMed]
- Ayegnon KG, Aupart M, Bourguignon T, et al. A 25-year experience with Carpentier-Edwards Perimount in the mitral position. Asian Cardiovasc Thorac Ann 2011;19:14-9. Retraction in: Asian Cardiovasc Thorac Ann 2011;19:292. [Crossref] [PubMed]