Increasing atmospheric temperature implicates increasing risk for acute type A dissection in hypertensive patients
Introduction
Acute aortic dissection is a life-threatening condition. The annual incidence is estimated around 11.9 per 100,000 (1). However, these numbers may underestimate the real incidence because of undiagnosed cases and out of hospital deaths (2,3). Type A aortic dissection (AAAD) is a surgical emergency (4). A mistaken initial diagnosis like myocardial infarction is very frequent (up to 30%) and can cause a significant time loss with increased risk of mortality (5,6). Mortality increases by 1% to 1.4% per hour when a patient remains untreated, leading to an almost 80% mortality rate without treatment (6,7). With surgical repair, in-hospital mortality remains at around 20–24% (6,7).
In order to optimize and accelerate diagnosis it is important to be aware of potential risk factors such as arterial hypertension, aortic dilatation or connective tissue diseases. However, besides these patient related aspects there might exist external factors which can increase the risk of an AAAD. There are studies discussing the potential impact of particular weather conditions with the occurrence of AAD (2,3,8-10). Most of them show a tendency with a peak of AAAD incidence in winter months and colder temperature but the results are not unambiguous (8,9,11,12).
The aim of the present study was to identify seasonal specific weather conditions (atmospheric temperature, humidity and atmospheric pressure) and patient characteristics predicting the incidence and occurrence of AAD.
We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/jtd-21-824).
Methods
Study design
This is a retrospective study of all consecutive patients who underwent emergency surgical treatment for AAAD at our Department. Data were prospectively collected and entered in our database.
Data collection
Baseline characteristics, operative variables and postoperative outcomes and follow-up information about survival, major adverse cardiac and cerebrovascular event (MACCE)—free survival and freedom from reoperation (late events) were collected. For follow-up, the patients were seen at the outpatient clinic or were contacted by telephone. The closing date for the analysis of this cohort was November 2017.
Weather information
The weather data were provided by the IDAweb data base of the federal office of Meteorology and Climatology MeteoSwiss (13). We obtained data from a weather station situated approximately 500 m east from our hospital, which is a good representative of our catchment area of the north-eastern part of Switzerland [roughly 12,000 km2 (14)]. The required information was the day mean value of atmospheric temperature, humidity and pressure for every day between January 1st 2006 and December 31st 2016. Additionally, we calculated temperature humidity and atmospheric pressure difference from one day to another by subtracting the value of the actual from the value of the previous day. This method was chosen by our professional statistician to be statistically appropriate in order to answer our question. All events of AAAD were then analyzed in correlation with the obtained daily weather data including atmospheric temperature, humidity and air pressure (constant, rising and lowering compared to the day before and after) within the entire cohort and in patients with or without hypertension separately. Furthermore, we analyzed if atmospheric temperature, air pressure, humidity had an impact on preoperative neurological impairment and postoperative mortality.
Definitions
Early death was defined as 30-day or in-hospital mortality. Interhospital transfer was not considered as discharge.
Renal impairment was defined as an increase of creatinine more than 50% (RIFLE-R/AKIN 1) (15).
Permanent central neurological deficit was diagnosed in the presence of a symptomatic patient with correlating central lesions in cerebral computed tomography. Peripheral neurological deficit was diagnosed in the presence of a symptomatic patient without correlating central lesions in cerebral computed tomography.
Ethics
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by local Ethics Committee of Zurich (NO.: 2017-00824) and informed consent was waived for all patients included until December 31st 2015. From January 1st 2016, all patients signed an informed consent according to the new national data privacy protection act.
Statistical analysis
All statistical analyzes were performed using IBM SPSS Statistics Version 23 (IBM Corp; Armonk, New York, USA) and R version 4.0.0 (R Foundation for Statistical Computing, Vienna, Austria). Categorical variables are presented as frequency with percentage, continuous variables as mean with standard deviation (SD). Follow-up survival was analyzed using Kaplan-Meier curves. To analyze the association of the occurrence of AAAD with season and weather, the numbers of events for each day between January 1, 2006 and December 31, 2016 were counted. Because there were only 0.4% (16/4,018) days with two events, we compared days with and without events. The proportion of days with events was compared between months using the chi-square test. The association between days with AAAD and changing weather conditions was analyzed using chi-square test. Logistic regressions were performed as a multivariate analysis to adjust atmospheric temperature, humidity and pressure for month, analyzed as a categorical variable. Goodness of fit was assessed using the Hosmer-Lemeshow test. As a cutoff for the significance level a P value <0.05 was defined.
Results
Clinical and intraoperative characteristics
Between January 1st 2006 and December 31st 2016 536 patients underwent surgery for AAAD at our department. In 19 cases, no consent for this study could be obtained. A total of 517 patients were finally included in the study. Mean age was 63.4±13 and 35.8% were older than 70 years; 69.4% were male and 68.9% had a known arterial hypertension. Twenty-four percent were smokers and 26.3% had known dyslipidemia. Six per cent of the patients (n=31) presented with preoperative hemiparesis. Baseline characteristics are presented in Table 1. In Table 2, intraoperative characteristics are shown: Supracoronary replacement was performed in 66.9% of the patients, hemiarch replacement in 54.9% and total arch replacement in 15.7%. The Bentall-De Bono operation was performed in 36.4% and a coronary artery bypass graft (CABG) in 9.4% of the patients.
Table 1
| Outcome | |
|---|---|
| N | 517 |
| Age | 63.4±13 (19.6–88) |
| >70 | 35.8% |
| Male | 359 (69.4) |
| Hypertension | 356 (68.8) |
| Aneurysm of ascending aorta | 226 (43.7) |
| Dyslipidemia | 136 (26.4) |
| Smoker | 124 (24.0) |
| Hemiparesis | 31 (6.0) |
| Reanimated | 21 (4.1) |
Mean with standard deviation or range and number of patients with percentage.
Table 2
| Outcome | |
|---|---|
| N | 517 |
| Cross clamp time | 109±54 |
| Total circulatory arrest | 37±22 |
| Deepest temperature | 26.2±4 |
| Antegrade cerebral perfusion | 430 (83.2) |
| Supracoronary replacement | 346 (66.9) |
| Hemiarch replacement | 284 (54.9) |
| Bentall-De Bono operation | 205 (39.7) |
| Biological prosthesis | 97 (18.7) |
| Mechanical prosthesis | 91 (17.6) |
| Aortic valve resuspension | 96 (18.6) |
| Total arch replacement | 81 (15.7) |
| Coronary surgery | 49 (9.5) |
| Valve sparing root repair | 18 (3.5) |
Mean with standard deviation or number of patients with percentage.
Early outcomes
Early outcomes are shown in Table 3. In-hospital mortality was 17.7% with the most frequent cause of death of multi organ failure. Postoperatively, 43.5% of the patients showed renal impairment, pneumonia appeared in 26.8%. Permanent central neurological impairment was observed in 86 patients (22.5%) and peripheral in 13.2%.
Table 3
| Outcome | |
|---|---|
| N | 517 |
| In-hospital mortality | 92 (17.7) |
| Unknown | 31 (5.9) |
| Multi organ failure | 23 (4.4) |
| Cardiac | 18 (3.5) |
| Neurological | 16 (3.1) |
| Bowel ischemia | 1 (0.2) |
| Mediastinitis | 3 (0.6) |
| Renal impairment | 167 (42.7) |
| Pneumonia | 131 (26.8) |
| Permanent central neurological event | 86 (22.5) |
| Peripheral neurological event | 46 (13.2) |
| Myocardial infarction | 29 (5.6) |
Number of patients with percentage.
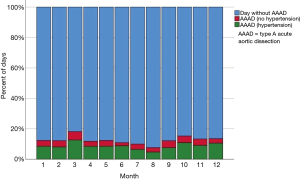
The analysis of a seasonal correlation between the occurrence of AAAD within the entire cohort revealed a significantly increased number of events in certain months of the year (March, October and December, P=0.016, Figure 1). Atmospheric temperature also showed an impact on AAAD (P=0.03) whereas air pressure (P=0.06) and humidity (P=0.87) did not.
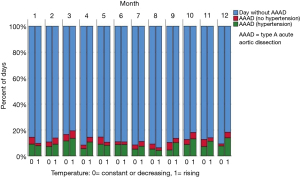
Subgroup analysis (hypertensive vs. non-hypertensive) revealed no impact on AAAD through air pressure (P=0.21) and humidity (P=0.59) but a significant monthly variation of AAAD occurrence in hypertensive (P=0.046, Figure 1). Furthermore, in hypertensive patients, a significantly increased risk of AAAD (34%) was present in conjunction with rising atmospheric temperature (OR 1.34, 95% CI: 1.06–1.69, P=0.015), while this was not seen in non-hypertensive patients (P=0.9). The overall range of temperature difference was 0.1–9.6 °C between the mean values of two consecutive days. The occurrence of AAAD depending on atmospheric temperature is presented in Figure 2. The analysis of atmospheric humidity and air pressure difference did not seem to have an impact on the occurrence of AAAD in the hypertensive group (P=0.25 and P=0.98 respectively).
Similarly, no significant correlation between seasonal changes and AAAD occurrence could be detected for preoperative neurological impairment (P=0.84 for temperature, P=0.36 for air pressure, P=0.45 for humidity) within the entire cohort. Because of the low appearance of neurological deficits, an analysis of the hypertensive group was neglected due to lack of power. In-hospital Mortality within the entire cohort and the hypertensive group showed no significant correlation either (P=0.37 for temperature, P=0.12 in hypertensive; P=0.32 for humidity, P=0.08 in hypertensive; P=0.95 for air pressure, P=0.86 in hypertensive).
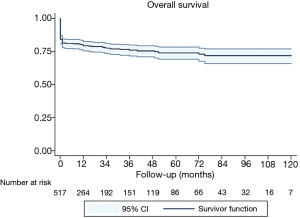
Follow-up
Median follow up was 12 (1–133) months and was completed in 468 (90.5%) with 72%±2.8% survival at 3 years presented in Figure 3.
Discussion
Our data suggest that there is an increased occurrence of AAD in March, October and December in our catchment area. Moreover, in hypertensive patients we detected a 34% increased occurrence of AAAD in weather conditions with rising atmospheric temperatures (independent from the absolute temperature at the time of the event).
In general, there are multiple patient-related factors which have been identified as risk factors for AAAD (16). However, evidence is still lacking, if specific external trigger factors such as change of temperature may also influence the occurrence: Multiple studies have analyzed different weather conditions being the most potent not individual biased criteria potentially influencing human physiology (9,11,12,17). While the results of these studies (i.e., increased incidence during winter months or colder temperature) mainly provided tendencies and only partial clarification, they did not improve the outcome of AAAD (18).
However, the identification of specific environmental and patient conditions could be important to predict or prevent the occurrence of AAD and to accelerate diagnosis and therapy thereby improving outcomes. In fact, our data enables us to make referring physicians more aware about the occurrence and incidence profile of AAD in our catchment area in order to prevent delayed diagnosis in the presence of increasing atmospheric temperatures and certain months of the year.
In the current literature several different correlations between weather conditions and the incidence of AAAD have been described such as increased incidence during winter (especially in January) and lower frequency in summer which corresponds with our findings (17). Mehta et al. studied 957 patients with non-traumatic AAAD enrolled in the International Registry of Acute Aortic Dissection (IRAD) and found a significant seasonal variation with the highest frequency during winter (9). A significant monthly peak was demonstrated in January in the total population studied, whereas this monthly variation was not observed for those patients with hypertension. It can be presumed, that the IRAD represents the data of many different countries with different climate, which might not be the ideal cohort to analyze local weather changes influencing AAD, unlike our study. Our results showed a monthly variation in the occurrence of AAD, with an increased occurrence in March, October and December (P=0.016) in the entire cohort. The reason for the temperature changes might be the unique variable topography in our catchment area with high mountains, lakes and wide planes, which cannot be reproduced by the data of the IRAD study. Different than in other countries, in our region of Switzerland the temperatures in March are similar to those in December, when we also found an increased occurrence of AAD (19). Similar to our study, also located on the northern hemisphere, Sumiyoshi et al. examined 435 patients in Japan and showed seasonal variation of the onset of AAAD with a peak in winter and a trough in summer (20). Takagi et al. did a meta-analysis of 18 studies with 101,264 patients and showed a statistically significant increase in AAAD incidence in winter compared to summer (OR 1.37; P<0.0001; winter 28.2%; summer 20.6%) (17). These findings are comparable to our study and the reason might be a constantly high atmospheric temperature level during the summer months without variations especially no more increase.
On one hand, our findings might be biased due to the summer holiday season in July and August with many residents leaving the country resulting in less AAAD. On the other hand the population count remains persistent, because many tourists visit during these months (up to 4.2 million according to the federal office of statistics) (21). Furthermore, these findings could also be related to the lack of stress with subsequent hypertensive phases: tourists tend to be less stressed and some locals usually enjoy their holidays quietly at home. This more convenient and stress-less lifestyle during the summer months combined with a constant weather might influences the patient population with certain risk factors (hypertension) and even prevents AAAD reflecting our results.
In 2010, Benouaich et al. described in a study with 206 patients in France a higher incidence of AAAD with decreasing temperatures not depending on the time of the year (8). The same results could be shown by Verberkmoes et al. in a retrospective work with 212 patients in the Netherlands (12). Like our study both were unable to show a correlation of other meteorological conditions. In these studies, showing the increased incidence of AAAD during winter months the potential influence of relative temperature elevation during the cold months was not analyzed (12,17). So, we additionally analyzed the correlation with two patient conditions (with and without arterial hypertension). We could demonstrate in the group of patients with high blood pressure a higher occurrence of AAAD during a relative increase of temperature. This might suggest that hypertensive patients react to temperature change differently compared to non-hypertensive ones.
Our data did not show any significant correlation between weather variables or its changes and preoperative neurological deficits or mortality.
The most common explanation for a higher incidence during cold weather is an increase of sympathetic activity resulting in increased vasoconstriction, systolic and diastolic blood pressure and heart rate (18,22). Nonetheless, the precondition for a normal vessel reaction to the sympathetic nervous system requires distensible vessels which are often not present any more in hypertensive patients due to arteriosclerosis (23,24). A stiff aorta is more vulnerable to shear stress, which can lead to the formation of aneurysm and aortic dissection (25).
Interestingly, this observation was independent from the absolute temperature when the event occurred (i.e., overall lower temperatures in winter months) suggesting that it is rather the increase and not the absolute temperature which drives the risk for the occurrence of AAAD. This is also further supported by the fact that we observed the fewest occurrence of AAAD in summer although the temperature is then generally higher than in other times in the year. This number might even be higher due to the fact that only 68.8% of the patients had documented hypertension in their baseline characteristics because they probably did not know about it before AAAD occurred. It has to be assumed that the incidence of AAAD has multifactorial etiology i.e., intrinsic (hypertension, tissue disease, etc.) combined with extrinsic factors (weather conditions with increasing temperature, etc.). The latter ones might only play a minor role with the major being individual micro- and macro-anatomical structural vessel changes over time. If this is the case, new imaging modalities assessing the vessel wall could be developed in the future for screening purposes to prevent AAAD from happening in patients at risk.
Limitations
The limitations of our study are the following: it is retrospective and observational. There might also be a variation in the time of onset of AAAD because we used the date of the referral to our hospital and not the beginning of the symptoms although that might account for a few hours of difference only. While we are fully aware that our results may be potentially influenced by other, unidentified factors, we consider them very useful for our daily routine and, importantly also hypothesis-generating for future studies in the field. Furthermore there might be unregistered und undiagnosed out-of-hospital deaths.
Conclusions
In conclusion, this study describes a significantly increased occurrence of AAD in hypertensive patients in weather conditions with increasing atmospheric temperature and an increased occurrence of AAAD in certain months of the year (March, October and December). However, further studies are needed to analyze the underlying pathophysiology of the occurrence of AAAD depending on changing weather conditions.
Acknowledgments
We would like to thank Prof. Burkhardt Seifert from the Division of Biostatistics of the University of Zürich who provided us with the statistical analysis.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/jtd-21-824
Data Sharing Statement: Available at https://dx.doi.org/10.21037/jtd-21-824
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/jtd-21-824). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by local Ethics Committee of Zurich (NO.: 2017-00824) and informed consent was waived for all patients included until December 31st 2015. From January 1st 2016 all patients signed an informed consent according to the new national data privacy protection act.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Clouse WD, Hallett JW Jr, Schaff HV, et al. Acute aortic dissection: population-based incidence compared with degenerative aortic aneurysm rupture. Mayo Clin Proc 2004;79:176-80. [Crossref] [PubMed]
- Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the diagnosis and management of patients with thoracic aortic disease. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology,American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons,and Society for Vascular Medicine. J Am Coll Cardiol 2010;55:e27-e129. [Crossref] [PubMed]
- Howard DP, Banerjee A, Fairhead JF, et al. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the Oxford Vascular Study. Circulation 2013;127:2031-7. [Crossref] [PubMed]
- Cooper M, Hicks C, Ratchford EV, et al. Diagnosis and treatment of uncomplicated type B aortic dissection. Vasc Med 2016;21:547-52. [Crossref] [PubMed]
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA 2000;283:897-903. [Crossref] [PubMed]
- Nienaber CA, Clough RE. Management of acute aortic dissection. Lancet 2015;385:800-11. [Crossref] [PubMed]
- Pape LA, Awais M, Woznicki EM, et al. Presentation, Diagnosis, and Outcomes of Acute Aortic Dissection: 17-Year Trends From the International Registry of Acute Aortic Dissection. J Am Coll Cardiol 2015;66:350-8. [Crossref] [PubMed]
- Benouaich V, Soler P, Gourraud PA, et al. Impact of meteorological conditions on the occurrence of acute type A aortic dissections. Interact Cardiovasc Thorac Surg 2010;10:403-6. [Crossref] [PubMed]
- Mehta RH, Manfredini R, Hassan F, et al. Chronobiological patterns of acute aortic dissection. Circulation 2002;106:1110-5. [Crossref] [PubMed]
- Pape LA, Tsai TT, Isselbacher EM, et al. Aortic diameter >or = 5.5 cm is not a good predictor of type A aortic dissection: observations from the International Registry of Acute Aortic Dissection (IRAD). Circulation 2007;116:1120-7. [Crossref] [PubMed]
- Kumar N, Pandey A, Venkatraman A, et al. Seasonality in acute aortic dissection related hospitalizations and mortality in the United States: a nationwide analysis from 2004-2011. Int J Cardiol 2015;179:321-2. [Crossref] [PubMed]
- Verberkmoes NJ, Soliman Hamad MA, Ter Woorst JF, et al. Impact of temperature and atmospheric pressure on the incidence of major acute cardiovascular events. Neth Heart J 2012;20:193-6. [Crossref] [PubMed]
- Federal Office for Meteorology and Climatology. Portrait Federal Office for Meteorology and Climatology: Available online: https://www.meteoswiss.admin.ch/home/about-us/portrait.html 2020
- Kennzahlen Regionalporträts 2020: Kantone [press release]. Available online: https://www.bfs.admin.ch/bfs/de/home/statistiken/regionalstatistik/regionale-portraets-kennzahlen/kantone/zuerich.html2020.
- Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 2012;120:c179-84. [PubMed]
- Golledge J, Eagle KA. Acute aortic dissection. Lancet 2008;372:55-66. [Crossref] [PubMed]
- Takagi H, Ando T, Umemoto T, et al. Meta-Analysis of Seasonal Incidence of Aortic Dissection. Am J Cardiol 2017;120:700-7. [Crossref] [PubMed]
- Manfredini R, Boari B, Gallerani M, et al. Chronobiology of rupture and dissection of aortic aneurysms. J Vasc Surg 2004;40:382-8. [Crossref] [PubMed]
- Federal Office for Meteorology and Climatology. Monthly and annual maps: Available online: https://www.meteoswiss.admin.ch/home/climate/swiss-climate-in-detail/monthly-and-annual-maps.html?filters=temp_mean_2016_03_2016; 2021
- Sumiyoshi M, Kojima S, Arima M, et al. Circadian, weekly, and seasonal variation at the onset of acute aortic dissection. Am J Cardiol 2002;89:619-23. [Crossref] [PubMed]
- Statistik Bf. Die Logiernächte sind in der Sommersaison 2017 stark angestiegen. Available online: https://www.bfs.admin.ch/bfs/de/home/statistiken/kataloge-datenbanken/medienmitteilungen.assetdetail.3822643.html. 2017.
- Brennan PJ, Greenberg G, Miall WE, et al. Seasonal variation in arterial blood pressure. Br Med J (Clin Res Ed) 1982;285:919-23. [Crossref] [PubMed]
- Blacher J, Asmar R, Djane S, et al. Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension 1999;33:1111-7. [Crossref] [PubMed]
- Alexander RW. Theodore Cooper Memorial Lecture. Hypertension and the pathogenesis of atherosclerosis. Oxidative stress and the mediation of arterial inflammatory response: a new perspective. Hypertension 1995;25:155-61. [Crossref] [PubMed]
- Erbel R, Alfonso F, Boileau C, et al. Diagnosis and management of aortic dissection. Eur Heart J 2001;22:1642-81. [Crossref] [PubMed]