Physiologic and immunologic effects of subxiphoid pulmonary lobectomy compared with transthoracic pulmonary lobectomy in a canine survival model
Introduction
Video-assisted thoracoscopic surgery (VATS) performed through a small-chest incision has been accepted as a minimal invasive surgical platform for thoracic disease. Several studies have determined that the VATS approach to major lung resection for lung cancer is associated with less pronounced immunosuppression effects than its equivalent thoracotomy procedure. Currently, VATS has replaced traditional thoracotomy as the standard operation for most thoracic surgical disease (1,2).
The subxiphoid approach to thoracic cavity is a well-accepted procedure in the treatment of thoracic disease. More recently, many surgeons have reported the clinical experiences of using a single subxiphoid incision to perform the thoracoscopic procedure (3,4). Despite the promising clinical results, there was no available information regarding the perioperative physiologic and immunological impact of the subxiphoid approach when compared to the transthoracic approach.
Proinflammatory cytokines, interleukin 6 (IL-6), C-reactive protein (CRP) levels, lymphocyte subpopulations, granulocyte counts, and monocyte counts are frequently used in the evaluation of systemic immune response activation (5-8).
In this study, these parameters were measured, before and after surgery, to clarify the surgical stress between standard transthoracic and subxiphoid pulmonary lobectomy.
To clarify the physiologic and immunologic effects of the subxiphoid thoracic procedure, we compared the perioperative physiological changes and immunological responses between standard transthoracic thoracoscopic and subxiphoid lobectomy in a canine model.
Methods
The studies were performed in 19 beagle dogs [8.083 kg, 95% confidence interval (CI): 7.648-8.517]. This study was approved by Institutional Animal Care and Use Committee (IACUC) of Chang Gung Memorial Hospital. The animals were fasted for 6 hours before operation. All procedures were performed under general anesthesia with endotracheal intubation with isoflurane (3%) inhalation. Separation of the lungs for one-lung ventilation was achieved by placing the endotracheal cuff into the main bronchus opposite to the surgical lung. After the surgery, 0.6 mL of 2% xylocaine was administered and 3 days of oral acetaminophen (30 mg/kg/day) were used to reduce post-operative pain in all animals. All animals were given intramuscular antibiotics (cefamezine, 20 mg/kg, Standard Chem & Pharm, Tainan, Taiwan) for 3 days and were euthanized at 2 weeks after surgery.
In the subxiphoid group (n=10), a 3-cm incision was made over the xiphoid process as an entrance to the pleural cavity via the subcostal tunnel. A wound protector system (Alexis Wound Retractor, Applied Medical, USA) was inserted from xiphoid incision into the chest cavity and aids in the retraction of wound edges for thoracic exploration. For the transthoracic approach, a 3-cm incision over the six or seventh intercostal space near the midclavicular line is used as the working port. After thoracic exploration, the predetermined lobectomies [right upper lobe (two animals in the subxiphoid group and two animals in the transthoracic group); right middle lobe (two animals, subxiphoid group; two animals, transthoracic group); right lower lobe (two animals, subxiphoid group; two animals, transthoracic group); left upper lobe (two animals, subxiphoid group; two animals, transthoracic group); and left lower lobe (two animals, subxiphoid group; one animal; transthoracic group)] were performed using the single-port VATS technique.
- An endoscope (a 4.5 mm flexible bronchoscope; Olympus, Tokyo, Japan) and two instruments, which were the endoscopic grasper (Scanlan International, Inc., USA) and curved Adson baby forceps, were used via the working port for anatomic lobectomy;
- The endoscopic grasper (Scanlan International, Inc.) was used to manipulate the pulmonary hilum, lung, and mediastinum structures;
- Hilar dissection and pulmonary vein isolation were achieved using an 18-cm curved Adson baby forceps;
- Ligation of pulmonary vein was achieved using a conventional suture ligatures (Ethicon PROLENE Suture) and 5-mm Hemoclips (Tyco Healthcare, USA);
- The LigaSure vessel sealing system (Valleylab, Tyco International Healthcare, Boulder, CO) was used to divide pulmonary vein 3 mm beyond the proximal ligature;
- After complete division of the pulmonary vein, the pulmonary artery is ligated and divided using suture ligatures, hemoclips, and the LigaSure vessel sealing system;
- A 45-mm vascular Endo-GIA (Echelon 45 Endopath stapler; Ethicon Endosurgery, USA) was passed through the port and used to transect the lobar bronchus;
- The resected lung specimen was retrieved via the port;
- The xiphoid wound was closed layer by layer using absorbable sutures.
During operation, the following parameters were recorded: heart rate (HR), mean arterial pressure (MAP), operative time, procedural success, and complications. Postoperatively, animals were given regular diets immediately after recovery from anesthesia. All animals were closely monitored by the veterinary staff for general status and sign of postoperative complication. Blood was taken before surgery, immediate after operation, and at postoperative days 1, 3, 7, and 14 for immunologic and inflammatory analysis. Necropsies were performed on postoperative day 14. At necropsy, the animals were examined for the presence of bleeding complication, postoperative infection, and evidence of vital organ injury.
Immunologic and inflammatory analysis
Leukocyte subset analysis and isolation of neutrophils and mononuclear cells. To determine leukocyte populations (CD4+ and CD8+ lymphocytes, monocytes and neutrophils), fresh heparinized blood was incubated with mouse anti-canine CD3, CD4, CD8, CD14, or CD45 monoclonal antibodies (BD PharMingenTM, BD Biosciences, Franklin Lakes, NJ, USA). The samples were analyzed using flow cytometry (Becton Dickinson, Mountain View, CA, USA) after lysis of red blood cells according to BD Biosciences manufacturer’s instructions.
Intracellular oxidative activity of neutrophils
Neutrophils were incubated with fluorogenic 2’,7’-dichlorodihydrofluorescein -diacetate (DCFH-DA, 5 M; Sigma, St. Louis, MO, USA) at 37 °C for 30 min. Following intracellular hydrolysis and subsequent oxidization, fluorescent intracellular neutrophil 20,70-dichlorodihydrofluorescein (DCFH) was assayed by flow cytometry.
Inducible nitric oxide synthase (iNOS) expression of monocytes
After cytospin preparation of peripheral blood mononuclear cells and fixation in methanol for 3 min, a rabbit anti-canine iNOS antibody (Abcam Biochemicals, Cambridge, UK) was applied for staining. Visualization of the labeled antibody was achieved by the use of an avidin-biotin complex method (LSAB 2 kit, Dako, Carpenteria and Vector Laboratories, Burlingame, CA, USA). iNOS expression in activated monocytes was determine using an image analyzer.
Enzyme-linked immunosorbent assay for IL-6 and CRP
Serum for IL-6 and CRP analysis was stored at −80 °C, and the concentrations of IL-6 and CRP were determined by enzyme-linked immunosorbent assay with a commercially available kit [IL-6 (Quantikine, R & D Systems Inc., Minneapolis, Minnesota, USA) and CRP (PharMingen, BD Biosciences, San Diego, California, USA)].
Statistical analysis
Except when otherwise mentioned, data are presented as mean and 95% CI. All data were analyzed with GraphPad Prism (version 5.0, GraphPad Software, San Diego, CA, USA). Differences between two groups were analyzed for statistical significance by nonparametric tests or the Mann-Whitney U test. The frequency distributions between two groups were tested by using a Fisher exact probability test. Statistical significance was defined as P<0.05.
Results
Physiological study
There was a significant decline in HR and MAP from baseline levels during surgery. However, the change in the HR and MAP between the groups was not statistically significant except at a time point of approximately 45 min after surgery (Figure 1).

Neutrophils and oxidative activity
The number of neutrophils increased significantly following surgery, and returned to the baseline levels at 7 days post-surgery. Significantly increased in DCFH activity was observed on postoperative days 1, 3, and 7. However, there were no statistically significant differences between the groups with regards to neutrophils cell counts and DCFH expression (Figure 2A,B).
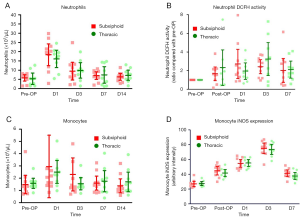
Monocytes and the intensity of iNOS expression
The monocyte count increased on postoperative day 1. The levels of iNOS expression increased in postoperative day 1 until postoperative day 7 in both groups. However, there were no statistically significant differences between the two groups in monocyte cell counts and iNOS expression at any of the study time points (Figure 2C,D).
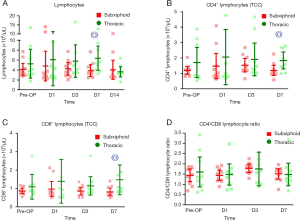
Lymphocytes and CD4/CD8 T lymphocyte subset analysis
Both surgical approaches resulted in significantly increase in the CD4+ T-cell count and CD4:CD8 ratio at 3 days after surgery. Seven days after surgery, the transthoracic groups had significantly higher total lymphocyte count, CD4+ T-cell count, and CD8+ T-cell count than the subxiphoid groups. However, there was no statistical significant difference in the CD4/CD8 ratio between the two groups at any time during the study (Figure 3).
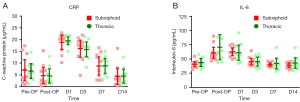
IL-6 and CRP levels
The CRP values increased from baseline on postoperative day 1 and 3. However, Levels of CRP were not different between the groups. The levels of IL-6 increased on postoperative day 1 and returned to preoperative levels on day 3. However, there were no significant differences between the groups (Figure 4).
Necropsy
The necropsy results demonstrated eight pleural adhesions in the subxiphoid group and seven pleural adhesions in the transthoracic group. All anatomic pulmonary lobectomies were performed correctly and completed as designated by the study. No evidence of pleural infection or postoperative complications was noted in either group. The airway and pulmonary vessels resection margin of all animals revealed complete healing.
Discussion
Currently, standard transthoracic thoracoscopic surgery offers smaller incisions, less post-operative pain, and quicker recovery in comparison to open thoracotomy (1,2,9). Several studies have investigated alternate surgical approaches to improve the treatment outcomes of patient with thoracic disease during the last decades. The results of this study further demonstrated the feasibility of the subxiphoid approach for performing pulmonary lobectomy with similar outcome compare to the standard transthoracic thoracoscopic surgery in canine models.
Advances in technology and endoscopic surgical instruments have allowed surgeons to be able to complete VATS through a single small incision (single port VATS) (10,11). However, the investigation of ideal platform of thoracic surgery is a continuous work for improving surgical outcome and reducing postoperative discomfort. Subxiphoid thoracic surgery is a well-established platform for thoracic procedures that include: coronary bypass, correction of pectus excavatum, anterior mediastinal tumor resection, and pericardial window creation for pericardial effusion (12-14). In terms of lung resection, Taniguchi et al. reported the feasibility of the partial resection of the bilateral lungs metastases from colorectal cancer with a 2.5-cm subxiphoid access port in a 72-year-old patient (15). Suda et al. reported the safety of the subxiphoid approach for bilateral partial lung resection in a 60-year-old man with bilateral metastatic pulmonary tumor from colorectal cancer (3). More recently, Liu et al. reported their successful experience with the subxiphoid approach in performing left upper lobectomy in a patient with primary lung cancer (16). However, the safety and effectiveness of subxiphoid major lung resection has not been confirmed with large clinical studies. In this study, we were able to complete anatomic pulmonary resection in all 10 animals with the subxiphoid technique. These results provide strong evidence for the investigation of alternative approach in thoracic surgery.
One of the major concerns of introducing alternative technique of surgical treatment for thoracic disease is the post-operative risk and complications. The potential complications of lung resection can include prolonged air leak, bleeding, and pleural infection. In the present study, there were no observable minor or major post-operative complications. This can be attributed to extensive experience of our research group in the investigation of minimally invasive platform (include divide and repair of pulmonary vessel and airway) for thoracic surgery in the current canine model. Furthermore, the current results may indicate that the subxiphoid approach is a practical and effective alternative to standard transthoracic approach for the anatomic lobectomy.
Another major concern of using the alternative technique in thoracic surgery is the immunologic and physiologic impacts of the procedure. Our research groups have previously investigated the inflammatory and hemodynamic responses of the natural orifice transluminal endoscopic surgery (NOTES) approach for lung resection.
In 2013, we reported a similar hemodynamic impact and inflammatory changes between transoral approach and standard transthoracic approach for surgical lung biopsy in a canine model (17). In 2015, we further demonstrated that the hemodynamic and inflammatory changes during transumbilical lung wedge resection are comparable to standard transthoracic VATS (18). In the present study, we observed a similar physiologic response between the subxiphoid approach and the standard transthoracic approach. Regarding to immunologic impact, many researchers have reported that the VATS approach to major lung resection is associated with less postoperative cell-mediated immunosuppression and better recovery, when compare to the thoracotomy approach. In this previous study, a significant decrease of total number of T lymphocytes and CD4+ T lymphocytes during the postoperative period in lung cancer patients who underwent lung cancer resection was observed in the thoracotomy group but not in the VATS approach group (19). In the present study, the total lymphocyte count, CD4, and CD8 lymphocyte counts in the subxiphoid group were lower on postoperative day 7 compared to the VATS results, suggesting that the subxiphoid method is associated with slower lymphocyte recovery than the standard transthoracic approach.
There are three potential advantages of subxiphoid thoracoscopic pulmonary lobectomy. First, this approach enables exposure to both lungs through a single incision.
Second, this technique does not require a transthoracic or intercostal incision, thereby reduces the risk of pulmonary complications and prevents injuries to the intercostal neurovascular bundles. Finally, pleural drain placed in the subxiphoid incision may cause less acute postoperative pain than the tube placed in the intercostal space by the conventional transthoracic technique, due a reduction of irritation of the intercostal nerves by chest tube in the patient with subxiphoid approach.
The present study has some limitations. First, the number of canines in each study group is limited. Second, the canine lungs have complete interlobar fissures, which seemed to be easier to perform anatomic lobectomy on when compared to incomplete interlobar fissures in human subjects. Third, a long distance between the xiphoid incision and the pulmonary hilum in human can lead to difficulties in completing the lobectomy. Finally, mediastinal lymph node dissections were not performed. Therefore, we cannot determine if mediastinal lymph node biopsy, a critical step in lung cancer management, is appropriate via the subxiphoid incision.
In conclusion, this study demonstrated that utilizing a subxiphoid approach for anatomic pulmonary lobectomy is feasible and effective in a canine survival study. This approach has similar physiologic responses but potentially has more pronounced immunosuppression when compare to standard transthoracic thoracoscopic surgery after anatomic pulmonary lobectomy. Clinical trials would further clarify the role of a subxiphoid approach in thoracoscopic surgery for thoracic disease.
Acknowledgements
This work was supported by the Chang-Gung Memorial Hospital, Taiwan (Contract No. CMRPG3E0751).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Flores RM, Park BJ, Dycoco J, et al. Lobectomy by video-assisted thoracic surgery (VATS) versus thoracotomy for lung cancer. J Thorac Cardiovasc Surg 2009;138:11-8. [PubMed]
- Onaitis MW, Petersen RP, Balderson SS, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg 2006;244:420-5. [PubMed]
- Suda T, Ashikari S, Tochii S, et al. Single-incision subxiphoid approach for bilateral metastasectomy. Ann Thorac Surg 2014;97:718-9. [PubMed]
- Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [PubMed]
- Ni Choileain N, Redmond HP. Cell response to surgery. Arch Surg 2006;141:1132-40. [PubMed]
- Ordemann J, Jacobi CA, Schwenk W, et al. Cellular and humoral inflammatory response after laparoscopic and conventional colorectal resections. Surg Endosc 2001;15:600-8. [PubMed]
- Craig SR, Leaver HA, Yap PL, et al. Acute phase responses following minimal access and conventional thoracic surgery. Eur J Cardiothorac Surg 2001;20:455-63. [PubMed]
- Wichmann MW, Hüttl TP, Winter H, et al. Immunological effects of laparoscopic vs open colorectal surgery: a prospective clinical study. Arch Surg 2005;140:692-7. [PubMed]
- Nagahiro I, Andou A, Aoe M, et al. Pulmonary function, postoperative pain, and serum cytokine level after lobectomy: a comparison of VATS and conventional procedure. Ann Thorac Surg 2001;72:362-5. [PubMed]
- Ocakcioglu I, Alpay L, Demir M, et al. Is single port enough in minimally surgery for pneumothorax? Surg Endosc 2015. [Epub ahead of print]. [PubMed]
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [PubMed]
- Takata M, Watanabe G, Ushijima T, et al. A novel internal thoracic artery harvesting technique via subxiphoid approach--for the least invasive coronary artery bypass grafting. Interact Cardiovasc Thorac Surg 2009;9:891-2. [PubMed]
- St Peter SD, Sharp SW, Ostlie DJ, et al. Use of a subxiphoid incision for pectus bar placement in the repair of pectus excavatum. J Pediatr Surg 2010;45:1361-4. [PubMed]
- Hsu CP, Chuang CY, Hsu NY, et al. Comparison between the right side and subxiphoid bilateral approaches in performing video-assisted thoracoscopic extended thymectomy for myasthenia gravis. Surg Endosc 2004;18:821-4. [PubMed]
- Taniguchi Y, Suzuki Y, Suda T, et al. Video-assisted thoracoscopic bilateral lung metastasectomy with a subxiphoid access port. J Thorac Cardiovasc Surg 2005;130:916-7. [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. [PubMed]
- Chu Y, Liu CY, Wu YC, et al. Comparison of hemodynamic and inflammatory changes between transoral and transthoracic thoracoscopic surgery. PLoS One 2013;8:e50338. [PubMed]
- Lu HY, Chu Y, Wu YC, et al. Hemodynamic and inflammatory responses following transumbilical and transthoracic lung wedge resection in a live canine model. Int J Surg 2015;16:116-22. [PubMed]
- Ng CS, Whelan RL, Lacy AM, et al. Is minimal access surgery for cancer associated with immunologic benefits? World J Surg 2005;29:975-81. [PubMed]


