Safety of thoracoscopic surgery for lung cancer without interruption of anti-platelet agents
Primary lung cancer is the second most commonly occurring cancer and the most common cause of cancer deaths worldwide (1). Non-small cell lung cancer comprises approximately 80% of all lung cancers. Surgery is the mainstay of treatment for non-small cell lung cancer, especially in the early stages, with lobectomy as the accepted standard (2). Increasing adoption of thoracoscopic surgery for this purpose has been observed over the previous two decades (3); the reported advantages of thoracoscopic lobectomy compared with open lobectomy include shorter chest tube durations, shorter hospital stays, decreased postoperative pain, and lower morbidity (3-5).
Antiplatelet agents (APAs) are the most frequently prescribed medications for a variety of conditions including coronary artery occlusive disease, cerebrovascular disease, atrial fibrillation, peripheral artery occlusive disease (PAOD), prevention of venous thromboembolism, and primary prevention in high-risk patients (6). The Antithrombotic Trialists’ Collaboration reported that APAs reduced the combined outcomes of any serious vascular event by approximately one quarter (non-fatal myocardial infarction by one third, non-fatal stroke by one quarter, and vascular mortality by one sixth) (7). As a result, surgeons frequently encounter patients who have been administered antiplatelet therapy preoperatively.
Concern regarding excessive perioperative bleeding has led to the general recommendation that APAs be discontinued 7-10 days preoperatively. However, withdrawal of APAs could increase the risk of perioperative cardiovascular events (8-10). The 2012 update to the Society of Thoracic Surgeons guidelines on the use of antiplatelet drugs in patients having cardiac and noncardiac operations recommends that continuing antiplatelet monotherapy is feasible and continuing dual antiplatelet therapy can be feasible in patients undergoing noncardiac surgery unless the risk of bleeding is prohibitive (11). However, studies regarding the safety of continuing APA treatment in general thoracic surgery, especially minimally invasive surgery, are rare.
This retrospective study was conducted to evaluate the safety, with regard to bleeding risk, and operative characteristics, with regard to extent of resection and dissection, of thoracoscopic surgery without interruption of APA.
Patients and methods
Patients
This retrospective study was approved by the institutional review board of the hospital (4-2014-0999) and the need for consent from individual patients was waived. Between January 2009 and February 2015, 1,384 patients underwent thoracoscopic surgery for curative resection of lung cancer, not including those who underwent wedge resection. Of the 164 patients that were taking APAs when the need for surgery was determined, the decision about interruption of APA for each patient was made by the surgeon, in consultation with the anesthesiologist, cardiologist, and neurologist, based on the risk of perioperative thrombotic events and bleeding. The medical records of these 164 patients were reviewed retrospectively.
Operative technique and postoperative care
In our institution, thoracoscopic lobectomy has been performed since 2005, and more than half of the resections for lung cancer are now performed by thoracoscopy. Thoracoscopic lobectomy or segmentectomy was performed with a 3-5 cm utility incision at the anterior axillary line of the fourth or fifth intercostal space using endoscopic instruments, without spreading the ribs, and 2-3 ports for the camera, stapler, and assistant. The operation was performed entirely with thoracoscopic visualization (12). Ultrasonic dissectors were used in most of the patients for tissue dissection and division.
One or two chest tubes were placed after the operation. Postoperative pain control was achieved using patient-controlled intravenous analgesia and supplemental intravenous opioids. An epidural was not used. APAs were readministered from postoperative day 1, if there was no postoperative bleeding complication. The last chest tube was removed when the amount of drainage was <250 mL/day and in the absence of air leaks and chyle leakage.
Perioperative cardiac risk
The perioperative cardiac risk was calculated by the authors using Lee’s revised cardiac risk index (rCRI) (13), which includes six clinical variables: high-risk surgery type (because intrathoracic procedures are classified as high-risk surgeries in the rCRI, all surgeries in this study were classified as high risk), history of ischemic heart disease, history of congestive heart failure, history of cerebrovascular disease, preoperative treatment with insulin, and preoperative serum creatinine >2.0 mg/dL.
Outcome measures
Intra/postoperative outcomes for safety comparisons included operating time, estimated blood loss, need for transfusion, amount and duration of chest tube drainage, length of hospital stay, change in hemoglobin, postoperative morbidity, and postoperative mortality. The change in hemoglobin excluded patients who received a transfusion with red blood cells during the operation or within 24 hours after the operation and was calculated as: hemoglobin on postoperative day 1—preoperative hemoglobin. To compare the oncological quality of the surgery, the extent of lung resection and lymph node dissection, number of dissected lymph nodes, and rate of complete resection were recorded.
Statistical analysis
Continuous data are expressed as median (range) and categorical data as n (percentage). The patients were placed into two groups for comparisons: preoperatively interrupted APA administration (group I) and continued APA administration (group N). Within group N, comparisons were also conducted between those administered aspirin + clopidogrel and those administered other APAs (aspirin only, clopidogrel only, other single APA, and aspirin + other APA). Continuous variables were compared between the groups using the Mann-Whitney U test, and categorical variables were compared using the Chi-squared tests or Fisher’s exact tests. All tests were two-sided, and a P value <0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 20.0 (IBM Corp., Armonk, NY, USA).
Results
Baseline characteristics
Group I consisted of 106 patients (64.6%), with a median duration of APA interruption of 9 [2-50] days. Group N consisted of 58 (35.3%) patients. The baseline characteristics of the patients are summarized in Table 1. Group N had significantly higher rCRI scores (P=0.001). Significantly more patients in group N were administered clopidogrel (P=0.025) or aspirin + clopidogrel (P=0.008). Significantly more patients in group I were administered APAs for primary intervention (P<0.001). Significantly more patients in group N had ischemic heart disease (P=0.007) and underwent percutaneous coronary intervention (PCI) (P=0.006).
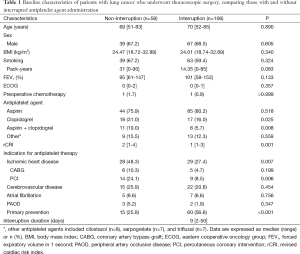
Full table
Characteristics of lung cancer and operation parameters
Characteristics of lung cancer and operative data are summarized in Tables 2,3. The groups were not significantly different in terms of lung cancer characteristics or extent of lung resection and lymph node dissection, number of dissected lymph nodes, rate of complete resection, rate of thoracotomy conversion, rate of transfusion, amount of blood loss during the operation, or operating time. Thoracotomy conversion was performed because of bleeding from the pulmonary artery in 4 patients (2 in each group), descending thoracic aorta rupture by linear stapler tip in 1 patient (group N), invasion to mediastinal pleura by tumor in 1 patient (group I) and severe pleural adhesion in 1 patient (group I).
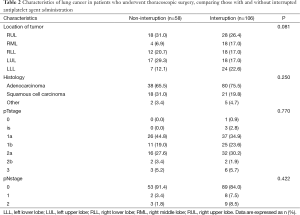
Full table

Full table
Postoperative outcomes
Postoperative outcomes are described in Table 4. The groups were not significantly different in the number of patients requiring transfusion within 30 days postoperatively, change in hemoglobin, amount of chest tube drainage over a period of 3 days, the length of hospital stay, postoperative bleeding and thrombotic complications, or operative mortality. Duration of chest tube drainage was little longer in patient group N (4 days in group N vs. 3.5 day in group I, P=0.036).
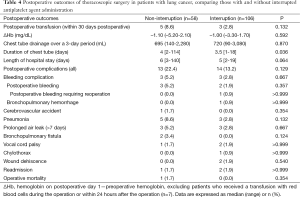
Full table
Postoperative bleeding occurred in 5 patients (3 in group N, 2 in group I; 1 reoperation was performed in the group I patient. The other patients were managed conservatively). One patient in group I experienced hemoptysis, with pulmonary infiltration on chest radiography (bronchopulmonary hemorrhage). He recovered without intervention and was discharged on postoperative day 11. There was one cerebrovascular accident in a group N patient who was administered aspirin + clopidogrel preoperatively for a cerebral infarction. Neurologic deficit was apparent immediately after the operation and acute cerebral infarction was confirmed using brain magnetic resonance imaging. There were no other cardiac or thrombotic complications.
Operative mortality occurred in one patient in group N. After the right lower lobe lobectomy, he was discharged on postoperative day 7 without any complications. He was readmitted with pneumonia, empyema, and a bronchopulmonary fistula on postoperative day 14 and died on postoperative day 89.
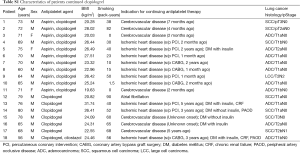
Table 5 provides the results of the comparisons between aspirin + clopidogrel and other APAs within group N. Patients administered aspirin + clopidogrel had significantly more postoperative bleeding (P=0.005), more chest tube drainage over a 3-day period (P=0.028), longer duration of chest tube drainage (P=0.028), and longer hospital stays (P=0.030). In addition, more patients required postoperative transfusion (P=0.001). Reoperation for bleeding was not required in any of the patients.
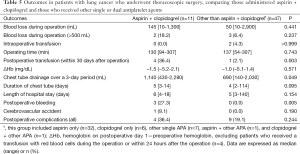
Full table
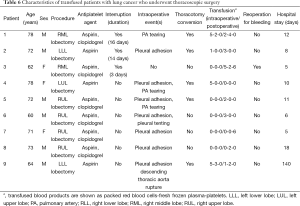
Transfusion was required for eight patients during and/or within 30 days after the operation (group I, n=3; group N, n=5) (Table 6). Most of these patients had pleural adhesion.
Full table
Discussion
The present results indicate that thoracoscopic surgery for lung cancer without interruption of APAs can be performed without an increase in the thoracotomy conversion rate, operating time, estimated blood loss during the operation, transfusion requirement, or postoperative bleeding complications.
APAs are administered for a variety of conditions, including coronary artery occlusive disease, cerebrovascular disease, atrial fibrillation, PAOD, prevention of venous thromboembolism, and primary prevention in high-risk patients (6). In the present study, approximately 10% of the patients who underwent thoracoscopic surgery for lung cancer were taking APAs, while in a population-based cohort study, approximately 26% of patients diagnosed with lung cancer were aspirin users (14). Concerns regarding the discontinuation of APAs include the resulting rebound effect and potentially increased coagulability from a systemic inflammatory reaction to surgery. The average postoperative myocardial infarction rate and mortality due to stent thrombosis during the re-endothelialization phase of a coronary stent are reportedly 35% and 20-40%, respectively. In addition, the treatment for postoperative myocardial infarction, including emergency PCI and thrombolysis, is more difficult and is associated with greater risk (15).
Aspirin does not appear to significantly increase bleeding complications (16,17), based on the results of two randomized clinical trials. The first, a multicenter, blinded study regarding the impact of preoperative maintenance or interruption of aspirin on thrombotic and bleeding events after non-cardiac surgery reported no differences in bleeding events between the aspirin (n=145) and placebo (n=146) groups at postoperative day 7 (n=9, 6.2% and n=8, 5.5%, respectively, P=0.81) or day 30 (n=10, 6.9% and n=10, 6.8%, respectively, P=0.99) (16). In the second, a double-blind study involving 220 patients, a 7.2% absolute risk reduction (95% confidence interval, 1.3-13%) in postoperative major adverse cardiac events was observed, without an increase in bleeding complications. Interestingly, a subjective assessment of intraoperative bleeding by the attending surgeon indicated no difference between the aspirin and placebo groups (17).
The effects of clopidogrel have typically been investigated for cardiac surgeries, resulting in increased blood loss, reoperations for bleeding, transfusion rate, and length of stay in the intensive care unit (15,18,19). However, in the study regarding the safety of general thoracic surgery in patients taking clopidogrel by Cerfolio et al., the risk of bleeding after primary thoracotomy or minimally invasive thoracic surgery was not increased (20). Although 12 lobectomies (11 open, 1 robot-assisted) and 6 thoracoscopic procedures were included, none of the patients underwent thoracoscopic lobectomy.
In addition to the reported advantages of shorter chest tube durations, shorter hospital stays, decreased postoperative pain, and lower morbidity with thoracoscopic lobectomies (3-5), decreased blood loss during the operation has also been reported (12). A few studies have recently reported that minimally invasive surgery in other surgical areas could be safely performed in patients taking APAs without an increase in bleeding complications (21,22). To the best of our knowledge, the present study is the first to suggest that a complex thoracoscopic procedure such as lobectomy can be performed safely, without increasing bleeding complications, blood loss, transfusion requirements, perioperative morbidity, or mortality.
In the present study, continuation of aspirin + clopidogrel was associated with increased postoperative bleeding, transfusion requirements, amount of chest tube drainage over a period of 3 days, duration of chest tube drainage, and length of hospital stay. Of the 11 patients taking aspirin + clopidogrel, 4 (36.4%) patients received transfusions postoperatively, and all had severe pleural adhesions (Table 6). This is consistent with the results of the study by Cerfolio et al., in which patients administered both aspirin and clopidogrel who underwent a redo thoracotomy for subsequent lung cancer needed reoperation because of postoperative bleeding. It appears to be more difficult to control bleeding from the chest wall secondary to the takedown of adhesions in patients taking aspirin + clopidogrel (20).
This study has several limitations. It was a retrospective study performed in a single institution with a small sample of patients. Patents of group N seem to have more cardiac or thrombotic risk and they could be performed simpler procedure for lung cancer. In fact, patients continuing clopidogrel tend to have recent cerebrovascular diasease, recent PCI or CABG, or multiple risk factor (Table S1). Because of the small sample of patients and few thromboembolic events, the effect of continued use APAs on perioperative thromboembolic events cannot be evaluated. In addition, we only compared postoperative outcomes but not the long-term oncologic outcomes of the perioperative use of APAs. However, there were no differences in the extent of resection and lymph node dissection, rate of complete resection, or number of dissected lymph nodes between the groups.
Full table
In conclusion, continued use of APAs during thoracoscopic surgery for lung cancer could be safely done in patients at high risk of cardiac or thrombotic events. However, in patients administered aspirin + clopidogrel, it may be the best to continue aspirin only because of an increased risk of postoperative bleeding and transfusion requirements.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflict of interest to declare.
References
- Parkin DM, Bray FI, Devesa SS. Cancer burden in the year 2000. The global picture. Eur J Cancer 2001;37 Suppl 8:S4-66. [PubMed]
- Spira A, Ettinger DS. Multidisciplinary management of lung cancer. N Engl J Med 2004;350:379-92. [PubMed]
- Stephens N, Rice D, Correa A, et al. Thoracoscopic lobectomy is associated with improved short-term and equivalent oncological outcomes compared with open lobectomy for clinical Stage I non-small-cell lung cancer: a propensity-matched analysis of 963 cases. Eur J Cardiothorac Surg 2014;46:607-13. [PubMed]
- Nicastri DG, Wisnivesky JP, Litle VR, et al. Thoracoscopic lobectomy: report on safety, discharge independence, pain, and chemotherapy tolerance. J Thorac Cardiovasc Surg 2008;135:642-7. [PubMed]
- Whitson BA, Groth SS, Duval SJ, et al. Surgery for early-stage non-small cell lung cancer: a systematic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg 2008;86:2008-16; discussion 2016-8.
- Eikelboom JW, Hirsh J, Spencer FA, et al. Antiplatelet drugs: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e89S-119S.
- Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002;324:71-86. [PubMed]
- Biondi-Zoccai GG, Lotrionte M, Agostoni P, et al. A systematic review and meta-analysis on the hazards of discontinuing or not adhering to aspirin among 50,279 patients at risk for coronary artery disease. Eur Heart J 2006;27:2667-74. [PubMed]
- Brichon PY, Boitet P, Dujon A, et al. Perioperative in-stent thrombosis after lung resection performed within 3 months of coronary stenting. Eur J Cardiothorac Surg 2006;30:793-6. [PubMed]
- Gerstein NS, Schulman PM, Gerstein WH, et al. Should more patients continue aspirin therapy perioperatively?: clinical impact of aspirin withdrawal syndrome. Ann Surg 2012;255:811-9. [PubMed]
- Ferraris VA, Saha SP, Oestreich JH, et al. 2012 update to the Society of Thoracic Surgeons guideline on use of antiplatelet drugs in patients having cardiac and noncardiac operations. Ann Thorac Surg 2012;94:1761-81. [PubMed]
- Lee JG, Cho BC, Bae MK, et al. Thoracoscopic lobectomy is associated with superior compliance with adjuvant chemotherapy in lung cancer. Ann Thorac Surg 2011;91:344-8. [PubMed]
- Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999;100:1043-9. [PubMed]
- Jonsson F, Yin L, Lundholm C, et al. Low-dose aspirin use and cancer characteristics: a population-based cohort study. Br J Cancer 2013;109:1921-5. [PubMed]
- Chassot PG, Delabays A, Spahn DR. Perioperative antiplatelet therapy: the case for continuing therapy in patients at risk of myocardial infarction. Br J Anaesth 2007;99:316-28. [PubMed]
- Mantz J, Samama CM, Tubach F, et al. Impact of preoperative maintenance or interruption of aspirin on thrombotic and bleeding events after elective non-cardiac surgery: the multicentre, randomized, blinded, placebo-controlled, STRATAGEM trial. Br J Anaesth 2011;107:899-910. [PubMed]
- Oscarsson A, Gupta A, Fredrikson M, et al. To continue or discontinue aspirin in the perioperative period: a randomized, controlled clinical trial. Br J Anaesth 2010;104:305-12. [PubMed]
- Chu MW, Wilson SR, Novick RJ, et al. Does clopidogrel increase blood loss following coronary artery bypass surgery? Ann Thorac Surg 2004;78:1536-41. [PubMed]
- Kapetanakis EI, Medlam DA, Boyce SW, et al. Clopidogrel administration prior to coronary artery bypass grafting surgery: the cardiologist’s panacea or the surgeon’s headache? Eur Heart J 2005;26:576-83. [PubMed]
- Cerfolio RJ, Minnich DJ, Bryant AS. General thoracic surgery is safe in patients taking clopidogrel (Plavix). J Thorac Cardiovasc Surg 2010;140:970-6. [PubMed]
- Binhas M, Salomon L, Roudot-Thoraval F, et al. Radical prostatectomy with robot-assisted radical prostatectomy and laparoscopic radical prostatectomy under low-dose aspirin does not significantly increase blood loss. Urology 2012;79:591-5. [PubMed]
- Bogani G, Cromi A, Uccella S, et al. Safety of perioperative aspirin therapy in minimally invasive endometrial cancer staging. J Minim Invasive Gynecol 2014;21:636-41. [PubMed]


