Air pollution and chronic airway diseases: what should people know and do?
Air pollution continues to be a significant concern to public health worldwide and a tough problem confronted by both developed and developing countries. In developed countries like United States and Europe countries, air pollution had been rather severe and remained a considerable environmental problem. Compared with most developed countries that had accomplished industrialization for years, developing countries are confronting more severe air pollution duo to intense energy consumption, large scale demolishment and reconstructions, and increased emissions from transportation in the process of industrialization and urbanization.
Burden of air pollution
According to the World Health Organization (WHO) report in 2008, 1.3 million deaths were estimated to be related to ambient air pollution globally. The figure became 3.7 million in 2012, which was nearly tripled. Two million deaths were attributable to the effects of household air pollution in 2008. This number also increased as nearly doubled (4.3 million) according to the latest report based on 2012 data by WHO recently. More than two million premature deaths each year were related to air pollution. Globally, seven million deaths were attributable to the joint effects of household and ambient air pollution in 2012 (1).
Air pollution has impact on most of the organs and systems of human body. Air pollutants can induce and aggravate diseases like cardiocerebral vascular disease, ischemia heart disease (2-6). Air pollution even has adverse effects on nervous system (7), digestive system (8), and urinary system (9). Long-term ambient air pollution exposure was reported to increase all-cause mortality (10). Air pollution is the cause and aggravating factor of many respiratory diseases like chronic obstructive pulmonary disease (COPD) (11,12), asthma (12,13), and lung cancer (14,15).
Struggle against air pollution seems to be a longtime task for both developed countries and developing countries (16-18), especially China (17,19-21). Apparently, as the air pollution remains a severe problem worldwide, to understand what constitute the air pollutants and what benefit measures could be taken is of help for people especially those with chronic respiratory diseases.
Components and sources of air pollutants
The pollutants vary with places, seasons and times. For instance, pollutants in ambient outdoor air and indoor air are not completely the same. The components are not the same at different place even in the same city.
Outdoor pollutants
The major pollutants in outdoor air are particulate matter (PM), ozone (O3), sulfur dioxide (SO2), nitrogen dioxide (NO2), carbon monoxide (CO), and Lead (Pb) (22). The pollutants in the ambient air can be divided into primary and secondary types (23). To offer guidance in reducing the impacts of air pollution on human health, WHO air quality groups (AQGs) released the air quality guidelines in which four pollutants namely PM, O3, NO2, and SO2 were listed as the indices of air pollution (23). Actually, air pollutants consist of various components including micro-organisms. Usually, lead and benzene homologues (20) are also considered the noteworthy pollutants in the air.
The pollutants in the ambient door air were mainly from industrial production, forest and brush fire, garbage burning, and emission of transport (23). The fine particles are those 2.5 micrometers or less in diameter. Motor vehicles, power plants, residential wood burning, forest fires, agricultural burning, some industrial processes, and other combustion processes are believed the major sources of them (24). In China, large scale straw burning is the source of severe air pollution at a specific time which brings in a haze climate directly. It is believed that the largest single source of airborne PM from motor vehicles is derived from diesel exhaust. The diesel exhaust particles account for up to 90% of airborne PM in the world’s largest cities (25). Other sources of PM include wild forest fire, burning of garbage, large scale demolishing and reconstructions. PMs are usually carbon particles, with other chemical components, microbes, and heavy metals deposit on their surface (12). PM10 and PM2.5 are two frequently-used indices for PM monitoring. PM2.5 is now used as a main indicator of risk to health from particulate pollution in the air quality indices (AQIs) in many countries.
Indoor pollutants
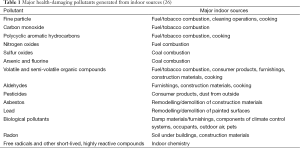
The indoor pollutants are different from that in the ambient air although most of them are the same. Nevertheless, indoor air contains all the same pollutants as in the outdoor air, but the concentrations are different, usually lower. Besides the same pollutants in outdoor air, there are some other components in indoor air which come from inside the building. The major sources include combustion of solid fuels indoors, tobacco smoking, emissions from construction materials and furnishings, and poor ventilation (Table 1) (26).
The indoor pollutants and sources are quite different between developed and developing countries. For example, combustion of solid fuels indoor is one of the main sources of indoor air pollution in developing countries while things are complete different in developed countries. In many developing countries, solid fuels such as biomass or coal are the major fuel source for cooking and heating. Combustion can produce CO, NO2, PM and other organic matter such as polycyclic aromatic hydrocarbons (PAHs). Some volatile organic compounds such as benzene and formaldehyde can also been produced by combustion (27). Combustion of coal can produce oxides of sulfur and toxic elements including arsenic, fluorine, selenium, and possibly mercury (28). The PAHs, which originate from combustion due to food cooking, can be in both gas and PM phases. The fractions of gaseous PAHs (97%) were consistently higher than the fractions of particulate PAHs (29). Poor ventilation, stove indoor without chimney, can result in a high concentration of air pollutants inside the building in the process of combustion. Tobacco smoking, which is also more common in developing countries duo to poor education, inefficient administration and poor policy of the government, can remarkably increase the concentration of pollutants indoor. Other indoor pollutants include the emissions such as radon gas from contractual material (30) and chemicals such as benzene and formaldehyde from furniture (20,31,32). The formaldehyde and benzene indoor are worthy of more attention duo to their concentration levels and hazardous properties (33). Improper maintenance of ventilation and air conditioning systems can further aggravate the indoor air pollution.
Impact of air pollution on human health
The health effects of air pollution remain a public health concern worldwide. Detrimental effects of air pollution were confirmed to be associated with growing morbidity and mortality. The adverse effects vary with the kinds of pollutants and locale. For instance, outdoor air pollutants like PM, NO2, and SO2 can increase mortality (10). Long-term exposure to fine PM can increase mortality (34), particularly from cardiovascular disease. It is reported that air pollutant such as O3 can increase the risk of appendicitis. Higher levels of ambient O3 exposure may even increase the risk of perforated appendicitis (8). Inspiration of PM containing PAHs and diesel was correlated with an increased risk of bladder cancer (9). Populations in cities, where the air pollution is usually severe duo to local high concentrations of pollutants from industry and vehicle emission, are at higher health risks. SO2 in the urban centers could increase children’s hospital admissions (35). High concentrations of ambient particles can trigger the onset of acute myocardial infarction and increase hospitalization for cardiovascular disease (36,37). Particulate particles, such as nanosized ones can easily pass through the blood-brain barrier and translocate to the central nervous system, where they can induce inflammation and changes of the blood-brain barrier (7), increase the risk for stroke, Parkinson’s disease, and neurodevelopmental disorders. Indoor air pollutants like formaldehyde and benzene can induce leukemia (32). Cooking emissions has particularly impact on housewife and the kitchen.
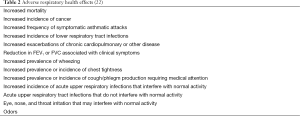
High levels of ambient air pollution are harmful to peoples, especially for those with chronic pulmonary disease. The impact of air pollutants on the respiratory system has been consistently reported in recent years (11,38-41). As indicated by the American Thoracic Society (ATS) provided guidance on definitions of what constitutes and adverse effect of air pollution (Table 2) (22), air pollution was associated with many respiratory diseases. The detrimental effects include decrease in pulmonary function (42), increase of infections (43), increase in respiratory symptoms (44), acute exacerbations of COPD (45), onset of asthma, more hospitalizations, increased respiratory mortality (11), and higher prevalence of childhood asthma (40).
COPD is characterized by an enhanced chronic inflammatory response in the airways and the lung to noxious particles or gases (41). Research demonstrated that women in developing countries had a high risk for chronic obstructive lung disease duo to exposure to household wood smoke from cooking (46). Air pollutants such as particular materials from fossil fuel combustion can cause inflammation in the lung and further impaired the reduced pulmonary function in COPD patients (47). When exposed to particle pollution, patients with COPD usually have more emergency room visit, hospital admission, or even death in some cases (24). Infection is one of the inducing factors of exacerbations of COPD. As PM can bring many micro-organisms on the surface, inhalation of PM may contribute to more frequent exacerbation of COPD. Other mechanisms including the detriment of mucociliary clearance, increase of the adherence of virus to respiratory mucus cells, and impairment of the resistance ability of immune system are all involved in the adverse effects of pollutants.
Air pollution can affect asthma prevalence, onset, symptoms, and the reaction to treatment. Air quality plays an important role in the inception of asthma early in life and as trigger of asthma exacerbations in later time (48). Exposure during infancy to NO2 increases the risk for childhood asthma. Research indicated that traffic-related air pollution exposure during infancy was associated with decreased lung function, and long-term respiratory consequences in susceptible children (49). Exposure to environmental agents indoors can also increase asthma symptoms or lead to asthma exacerbations. Long-term exposure to ambient air pollution can damage lung function in children. Air pollution levels are related to asthma control (50). Increased outdoor air pollution levels were associated with more frequent use of rescue inhalers in patients with asthma. Recent exposure to NO2 and possibly O3 may reduce the response to short-acting beta-agonists in children with asthma (50).
Air pollution has impact on lung cancer. Lung cancer is one of the most common cancers in city population. Research showed that an increase in road traffic was associated with lung cancer. Ambient air pollution, specifically PM and NO2 were associated with a higher risk for lung cancer (14,51). PM was significantly associated with lung cancer especially adenocarcinomas lung cancer.
Measures for reducing adverse effects of air pollution in general
The detrimental effects to health from air pollution are largely determined by the concentration of air pollutants and the amount of exposure time. People can take many measures to reduce the amount of pollutant inhalation. Some measures are appropriate for all people. Some others are of particular importance for those with chronic respiratory diseases. People should keep a good living habit and regulate their daily activity according to the local air quality report. For people with chronic respiratory disease like COPD, reduction of exposure to indoor and outdoor air pollution can reduce the risk for acute exacerbation of COPD. For asthma patients, less exposure can reduce the onset of asthma. Regular treatments under the guidance of physicians are recommended. Patients should not change daily remedies without permission from their doctors. Because air pollution usually maintain at different level for days or months, taking extra measures is of help for people especially those with chronic respiratory diseases.
Measures against ambient air pollution
Regulate daily activity according to the air quality index (AQI)
People can reduce the detrimental effects of ambient air pollution by shorting the time spent on activity outdoor and the level of activity when AQI is beyond a specified level. The AQI is a index for reporting daily air quality, which has been used by the U.S. Environmental Protection Agency to provider simple information about local air quality since 2009 (24). It is calculated from four major air pollutants: ground level O3, particle pollution, CO, and SO2 (24). In March, 2012, The Ministry of Environmental Protection of China began to implement National Standard for Air Quality. In which, AQI was also adopted and PM2.5 was added as a major index. The AQI tells people how clean or unhealthy the air is, and what associated health effects might be a concern. The AQI can be reached from website of the government, the local media such as newspapers and television, and client end software on mobile phone today. When the AQI reaches a certain high level, people should reduce the time outdoor and exerted activity in the polluted air (Table 3) (24). AQI values can vary from one season to another, in different place even in the same city, and on different time. In urban area, CO may be high in the central area during the rush hours because large amount of vehicles and usually poor air flow. O3 level is often higher in warmer months and peak in the afternoon to early evening. Particle pollution is often elevated near busy roadways, especially during morning or evening rush hours (24).
Subjects with chronic respiratory disease, such as COPD and asthma, should regulate their daily activity according to the local AQI report. For example, people in United States should reduce prolonged or heavy outdoor exertion when AQI is over 50. In addition, more attention should be paid to what pollutants are elevated beyond normal level in the AQI report. For instance, the level of O3, to which, patients with COPD and asthma are particularly sensitive. Exposure to O3, even at a lower level, can lead to aggravation of the diseases, increased medication, more doctor and emergency room visits and hospital admissions. People with asthma are more sensitive to SO2. Even a very brief exposure, as short as minutes, can trigger bronchospasm, leading to wheezing, chest tightness, and shortness of breath. The level of NO2 and possibly O3 may reduce the response to short-acting bronchial-agonists in children with asthma, subjects with asthma should take adequate measures besides using inhaled bronchodilators regularly, when the levels of NO2 continually higher than normal.
Use of masks
Wearing personal protective equipment (N95 mask or equivalent) might be a useful for avoiding detrimental effect of ambient air pollutants (29). Masks have been proved useful in reducing respiratory virus transmission during a pandemic (52). Using of nose mask during haze environment can help people to prevent adverse effects from vehicular pollution (53).
Masks can be divided into at least two categories. One type works by mechanical filtration that reduces the PM and the other absorbing gaseous chemicals by the activated carbon inside. Surgical face mask and plain face mask are designed for preventing and avoiding spillage droplets spread and large particulate materials usually hundred micrometer large. But they are not of any use in preventing inhalation of fine articles like PM2.5. N95 and R95 face mask is a kind of efficient filter masks which can absorb as high as 95% of airborne particles in the inhaled air (54). The later type is more efficient and should be recommended as efficient protective measure in minimizing exposure to gas emissions (29). But the disadvantage of these kinds of masks are obvious, they are not comfortable duo to their high respiratory resistance and can not be worn for long time. The efficiency of air filtration and chemical absorption will be lowered when used for a certain time, and frequent replacement would result in a high financial burden. To date, there is no recommended guidance for masks in preventing effects of air pollution.
Measures for indoor air pollution
As many people spend most of their time indoors, to reduce the production of indoor pollutants and avoid inhalation are more important. To choose furniture with less chemical emission, check the ventilation system of the house regularly, ventilate the room as opening the door and windows regularly to fresh the air so as to reduce harmful gaseous pollutants from the furniture and construction material, use clean fuels instead of biomass fuels if possible, improve cooking stoves to burn fuel more efficiently and use a chimney woodstove to vent emissions to outside, and similar interventions are feasible and recommended (55,56). These measures can significantly reduced indoor air pollution and relieve symptoms consistent with chronic respiratory tract irritation (46).
Besides these measures, air filtration is frequently recommended as an environmental control measure for patients with chronic respiratory disease. Particle filtration can be effective in reducing PM quantity particularly in homes. Particle filtration systems can supply filtered air into the room or whole-house, reducing indoor exposures to particles from outdoor air and reduce the morbidity and mortality associated with air particles (57). People with chronic respiratory disease may benefit from use of particle filtration systems in their home. Researches demonstrated that using indoor air cleaning devices can significantly reduce indoor PM concentrations, improve air quality, increase symptom-free days (58), reduce asthma trigger and improve health outcomes (59). improve bronchial hyperresponsiveness in asthma children (60), and reduce asthma morbidity (61) by filtrating particle and adsorbing gaseous pollutants. Forced air systems with high efficiency filtration can reduce many asthma triggers and provide effective means of controlling allergen levels (62).
There are many types of in-room air cleaners divided mainly by the type of air cleaning technology used. They can also be divided into portable or fixed devices as wall attached or ceiling mounted. The basic mechanism of air cleaner is air filtration by which airborne pathogens were reduced and spread of airborne infectious diseases was prevented. Most air cleaners have HEPA filter, which is highly efficient in PM filtration. Air cleaners with electrostatic generator can also considerably reduce particle concentration in indoor air (63). Other units include UVGI lights, ions generator, and activated carbon. Those units work in different way to reduce micro-organism or absorbing aero-chemicals. For improving indoor air quality of houses and buildings more efficiently, combined systems employing types of air filter units were recommended. For example, one study reported a complex air cleaner which consisted of four types air filter units: an activated charcoal filter (ACF), an unit for trapping agent for acidic gases, a MnO2 filter for oxidative decomposition of formaldehyde, and a photocatalyst filter coupled with a parallel beam ultraviolet irradiation device (33). Recently, new type of air cleaner with nova technology might be more efficient. For example, plasma cluster ion air purifier uses a multilayer filter system composed of a prefilter, a carbon filter, an antibacterial filter, and a HEPA filter, combined with an ion generator to purify the air efficiently (64). The plasma cluster ion air purifier can disable airborne microorganisms through the generation of ions in addition to PM filtration and other gaseous chemical pollutant absorption. This advance is especially important for people with chronic respiratory diseases.
During smoke episodes like forest fires, community members should remain indoors and use air cleaners. The air cleaner can effectively reduce PM2.5 exposure during forest fires and residential wood burning (65). Electrostatic air cleaners can reduce all size particles. The irritation and general symptom indices decreased (66). In peoples exposed to smoke from wildfire, using of high-efficiency particulate air cleaners could reduce odds of reporting adverse health effects of the lower respiratory tract (67).
Other measures
Smoking cessation
Smoking cessation is an important and relatively easy measure to take for all cigarette smokers particularly patients with chronic respiratory diseases (68,69). Smoking itself is one of the sources of air pollution in a closed space such as a room, besides its pathogenic role in the pathogenesis of COPD. Smoking cessation is important for patients with asthma too. In smokers with asthma, lung function can be improved and sputum neutrophil percentage reduced by smoking cessation (70). It is no doubt that smoking cessation is the one of the main interventions for COPD and asthma patients especially when facing the air pollution,
Sufficient nutrients
Although seemingly having no direct relationship with the diverse effects of air pollution, dietary nutrients remain important protective factors for respiratory health (71). High intake of fresh fruit and some vegetables has beneficial effects on lung health. Fruits and vegetables contain various nutrients like antioxidant vitamins such as vitamin C, vitamin E and so on. The antioxidant vitamins have a protective effect in the oxidative process and inflammatory response implicated in lung diseases. This protective effect might become more important in defending the adverse effects of air pollutants. Study showed that children with high consumption of leafy vegetables had a better lung function and less respiratory symptoms (71), fruit and vegetable intake had strong associations with symptoms. Low consumption of fish and fruit affected symptoms like persistent cough and wheeze (72). Since nutrients like vitamins and other mineral substances are involved in cell metabolism and the maintain of immuno-defence system, nutrients are of great importance in defending detriments from environment including air pollution, Therefore sufficient consumption of fruit and vegetables should be recommended in subjects with additional oxidative stress challenge, such as exposure to high levels of air pollution (73).
Herbal medicines
Herbal medicine among COPD patients was popular in East Asia. In China, traditional Chinese medicine has been used for hundred years in treating chronic bronchitis and asthma. Some aromatic herbal medicines were used to prevent respiratory infections. Herbal medicines were also tried to improve the air quality. For example, compound Xiangai aerosol is reported to be able to reduce the number of particles and bacteria in a certain space, and hence improve the air quality (74). Recently, a study, which demonstrated the effectiveness of a Chinese medicine on influenza, shed light to its future use in respiratory disease (75). Several herbal medicines including Panax ginseng and Salvia miltiorrhiza might be useful, but the effectiveness can not be established beyond reasonable doubt (76). On the whole, effectiveness of herbal medicines in treating COPD exacerbated by air pollutants has not been established on evidence-based medicine. Obviously, research of herbal medicines in preventing and treating pulmonary detriment duo to air pollution is currently scarce and well-designed studies seem warranted.
In summary, exposure to air pollution has many substantial adverse effects on human health. The health effects of air pollution depend on the components and sources of pollutants, which vary with countries, seasons, and times. Subjects with chronic respiratory diseases such as COPD and asthma are especially vulnerable to the detrimental effects of air pollutants. To reduce the harmful effects of ambient air pollution, people should be aware of the local air quality and take extra measures such as reducing the time outdoor and wearing masks when necessary. For reducing the air pollutants indoor, use of clean fuels, improved stoves, and air cleaners are recommended. Smoking cessation and adequate diet are suitable for all people.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- World Health Organization. Burden of disease from joint effects of household and ambient air pollution for 2012. Cited 2015 Oct 31. Available online: http://apps.who.int/gho/data/node.home
- Watson KE. Air pollution and heart disease. Rev Cardiovasc Med 2006;7:44. [PubMed]
- Scarborough P, Allender S, Rayner M, et al. Contribution of climate and air pollution to variation in coronary heart disease mortality rates in England. PLoS One 2012;7:e32787. [PubMed]
- Rückerl R, Ibald-Mulli A, Koenig W, et al. Air pollution and markers of inflammation and coagulation in patients with coronary heart disease. Am J Respir Crit Care Med 2006;173:432-41. [PubMed]
- Hassing C, Twickler M, Brunekreef B, et al. Particulate air pollution, coronary heart disease and individual risk assessment: a general overview. Eur J Cardiovasc Prev Rehabil 2009;16:10-5. [PubMed]
- Gold DR, Samet JM. Air pollution, climate, and heart disease. Circulation 2013;128:e411-4. [PubMed]
- Genc S, Zadeoglulari Z, Fuss SH, et al. The adverse effects of air pollution on the nervous system. J Toxicol 2012;2012:782462.
- Kaplan GG, Tanyingoh D, Dixon E, et al. Ambient ozone concentrations and the risk of perforated and nonperforated appendicitis: a multicity case-crossover study. Environ Health Perspect 2013;121:939-43. [PubMed]
- Castaño-Vinyals G, Cantor KP, Malats N, et al. Air pollution and risk of urinary bladder cancer in a case-control study in Spain. Occup Environ Med 2008;65:56-60. [PubMed]
- Carey IM, Atkinson RW, Kent AJ, et al. Mortality associations with long-term exposure to outdoor air pollution in a national English cohort. Am J Respir Crit Care Med 2013;187:1226-33. [PubMed]
- Faustini A, Stafoggia M, Colais P, et al. Air pollution and multiple acute respiratory outcomes. Eur Respir J 2013;42:304-13. [PubMed]
- Kelly FJ, Fussell JC. Air pollution and airway disease. Clin Exp Allergy 2011;41:1059-71. [PubMed]
- Karakatsani A, Analitis A, Perifanou D, et al. Particulate matter air pollution and respiratory symptoms in individuals having either asthma or chronic obstructive pulmonary disease: a European multicentre panel study. Environ Health 2012;11:75. [PubMed]
- Vineis P, Hoek G, Krzyzanowski M, et al. Air pollution and risk of lung cancer in a prospective study in Europe. Int J Cancer 2006;119:169-74. [PubMed]
- Sax SN, Zu K, Goodman JE. Air pollution and lung cancer in Europe. Lancet Oncol 2013;14:e439-40. [PubMed]
- Morawska L, Thomas S, Bofinger N, et al. Comprehensive characterization of aerosols in a subtropical urban atmosphere: particle size distribution and correlation with gaseous pollutants. Atmospheric Environment 1998;32:2467-78.
- Zheng M, Salmon LG, Schauer JJ, et al. Seasonal trends in PM2.5 source contributions in Beijing, China. Atmospheric Environment 2005;39:3967-76.
- Zhu Y, Hinds WC, Kim S, et al. Study of ultrafine particles near a major highway with heavy-duty diesel traffic. Atmospheric Environment 2002;36:4323-35.
- The state environmental protection bureau. 2002 Report on the State of Environment in China. Environment Protection 2003:3-13.
- Li L, Li H, Zhang X, et al. Pollution characteristics and health risk assessment of benzene homologues in ambient air in the northeastern urban area of Beijing, China. J Environ Sci (China) 2014;26:214-23. [PubMed]
- Millman A, Tang D, Perera FP. Air pollution threatens the health of children in China. Pediatrics 2008;122:620-8. [PubMed]
- American Thoracic Society. What constitutes an adverse health effect of air pollution? Official statement of the American Thoracic Society. Am J Respir Crit Care Med 2000;161:665-73. [PubMed]
- Sivertsen B. Air Quality Guidelines Global Update 2005. 2006. Available online: http://www.euro.who.int/pubrequest
- U.S. Environmental Protection Agency. Air quality index. Research Triangle Park. NC: 2009. Available online: http://www.airnow.gov
- Shah SD, Cocker DR, Miller JW, et al. Emission rates of particulate matter and elemental and organic carbon from in-use diesel engines. Environmental Science & Technology 2004;38:2544-50. [PubMed]
- Zhang J, Smith KR. Indoor air pollution: a global health concern. Br Med Bull 2003;68:209-25. [PubMed]
- de Koning HW, Smith KR, Last JM. Biomass fuel combustion and health. Bull World Health Organ 1985;63:11-26. [PubMed]
- Finkelman RB, Belkin HE, Zheng B. Health impacts of domestic coal use in China. Proc Natl Acad Sci U S A 1999;96:3427-31. [PubMed]
- Zhao P, Yu KP, Lin CC. Risk assessment of inhalation exposure to polycyclic aromatic hydrocarbons in Taiwanese workers at night markets. Int Arch Occup Environ Health 2011;84:231-7. [PubMed]
- Wang J, Meisenberg O, Chen Y, et al. Mitigation of radon and thoron decay products by filtration. Sci Total Environ 2011;409:3613-9. [PubMed]
- Bentayeb M, Billionnet C, Baiz N, et al. Higher prevalence of breathlessness in elderly exposed to indoor aldehydes and VOCs in a representative sample of French dwellings. Respir Med 2013;107:1598-607. [PubMed]
- Costantini AS, Benvenuti A, Vineis P, et al. Risk of leukemia and multiple myeloma associated with exposure to benzene and other organic solvents: evidence from the Italian Multicenter Case-control study. Am J Ind Med 2008;51:803-11. [PubMed]
- Sekine Y, Fukuda M, Takao Y, et al. Simultaneous removal of formaldehyde and benzene in indoor air with a combination of sorption- and decomposition-type air filters. Environ Technol 2011;33:1983-9. [PubMed]
- Dockery DW, Pope CA 3rd, Xu X, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med 1993;329:1753-9. [PubMed]
- Barnett AG, Williams GM, Schwartz J, et al. Air pollution and child respiratory health: a case-crossover study in Australia and New Zealand. Am J Respir Crit Care Med 2005;171:1272-8. [PubMed]
- Gill EA, Curl CL, Adar SD, et al. Air pollution and cardiovascular disease in the Multi-Ethnic Study of Atherosclerosis. Prog Cardiovasc Dis 2011;53:353-60. [PubMed]
- Peters A, Dockery DW, Muller JE, et al. Increased Particulate Air Pollution and the Triggering of Myocardial Infarction. Circulation 2001;103:2810-5. [PubMed]
- Raaschou-Nielsen O, Andersen ZJ, Beelen R, et al. Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). Lancet Oncol 2013;14:813-22. [PubMed]
- Pope CA 3rd, Burnett RT, Thun MJ, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 2002;287:1132-41. [PubMed]
- Nishimura KK, Galanter JM, Roth LA, et al. Early-life air pollution and asthma risk in minority children. The GALA II and SAGE II studies. Am J Respir Crit Care Med 2013;188:309-18. [PubMed]
- Global l Initiative for Chronic Obstructive Lung Disease. 2014. Available online: http://www.goldcopd.org
- Lagorio S, Forastiere F, Pistelli R, et al. Air pollution and lung function among susceptible adult subjects: a panel study. Environ Health 2006;5:11. [PubMed]
- Dominici F, Peng RD, Bell ML, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA 2006;295:1127-34. [PubMed]
- Delfino RJ, Gong H, Linn WS, et al. Asthma Symptoms in Hispanic Children and Daily Ambient Exposures to Toxic and Criteria Air Pollutants. Environmental Health Perspectives 2003;111:647-56. [PubMed]
- Medina-Ramón M, Zanobetti A, Schwartz J. The effect of ozone and PM10 on hospital admissions for pneumonia and chronic obstructive pulmonary disease: A national multicity study. Am J Epidemiol 2006;163:579-88. [PubMed]
- Smith-Sivertsen T, Diaz E, Pope D, et al. Effect of reducing indoor air pollution on women’s respiratory symptoms and lung function: the RESPIRE Randomized Trial, Guatemala. Am J Epidemiol 2009;170:211-20. [PubMed]
- Abbey DE, Burchette RJ, Knutsen SF, et al. Long-term particulate and other air pollutants and lung function in nonsmokers. Am J Respir Crit Care Med 1998;158:289-98. [PubMed]
- Teague WG, Bayer CW. Outdoor air pollution. Asthma and other concerns. Pediatr Clin North Am 2001;48:1167-83. ix. [PubMed]
- Schultz ES, Gruzieva O, Bellander T, et al. Traffic-related air pollution and lung function in children at 8 years of age: a birth cohort study. Am J Respir Crit Care Med 2012;186:1286-91. [PubMed]
- Hernández-Cadena L, Holguin F, Barraza-Villarreal A, et al. Increased levels of outdoor air pollutants are associated with reduced bronchodilation in children with asthma. Chest 2009;136:1529-36. [PubMed]
- Nawrot TS, Nackaerts K, Hoet PH, et al. Lung cancer mortality and fine particulate air pollution in Europe. Int J Cancer 2007;120:1825-6; author reply 7.
- MacIntyre CR, Cauchemez S, Dwyer DE, et al. Face Mask Use and Control of Respiratory Virus Transmission in Households. Emerg Infect Dis 2009;15:233-41. [PubMed]
- Ingle ST, Pachpande BG, Wagh ND, et al. Exposure to vehicular pollution and respiratory impairment of traffic policemen in Jalgaon City, India. Ind Health 2005;43:656-62. [PubMed]
- Wertheim HF, Ngoc DM, Wolbers M, et al. Studying the effectiveness of activated carbon R95 respirators in reducing the inhalation of combustion by-products in Hanoi, Vietnam: a demonstration study. Environ Health 2012;11:72. [PubMed]
- Liu S, Zhou Y, Wang X, et al. Biomass fuels are the probable risk factor for chronic obstructive pulmonary disease in rural South China. Thorax 2007;62:889-97. [PubMed]
- Romieu I, Riojas-Rodriguez H, Marron-Mares AT, et al. Improved biomass stove intervention in rural Mexico: impact on the respiratory health of women. Am J Respir Crit Care Med 2009;180:649-56. [PubMed]
- Fisk WJ. Health benefits of particle filtration. Indoor Air 2013;23:357-68. [PubMed]
- Butz AM, Matsui EC, Breysse P, et al. A Randomized Trial of Air Cleaners and a Health Coach to Improve Indoor Air Quality for Inner-City Children With Asthma and Secondhand Smoke Exposure. Arch Pediatr Adolesc Med 2011;165:741-8. [PubMed]
- Wu F, Takaro TK. Childhood asthma and environmental interventions. Environ Health Perspect 2007;115:971-5. [PubMed]
- Sulser C, Schulz G, Wagner P, et al. Can the Use of HEPA Cleaners in Homes of Asthmatic Children and Adolescents Sensitized to Cat and Dog Allergens Decrease Bronchial Hyperresponsiveness and Allergen Contents in Solid Dust? Int Arch Allergy Immunol 2009;148:23-30. [PubMed]
- Lanphear BP, Hornung RW, Khoury J, et al. Effects of HEPA Air Cleaners on Unscheduled Asthma Visits and Asthma Symptoms for Children Exposed to Secondhand Tobacco Smoke. Pediatrics 2011;127:93-101. [PubMed]
- Myatt TA, Minegishi T, Allen JG, et al. Control of asthma triggers in indoor air with air cleaners: a modeling analysis. Environ Health 2008;7:43. [PubMed]
- Wargocki P, Wyon DP, Lynge-Jensen K, et al. The effects of electrostatic particle filtration and supply-air filter condition in classrooms on the performance of schoolwork by children (RP-1257). HVAC&R Researchv 2008;14:327-44.
- Health Quality Organization. Air cleaning technologies: an evidence-based analysis. Ont Health Technol Assess Ser 2005;5:1-52. [PubMed]
- Barn P, Larson T, Noullett M, et al. Infiltration of forest fire and residential wood smoke: an evaluation of air cleaner effectiveness. J Expo Sci Environ Epidemiol 2008;18:503-11. [PubMed]
- Skulberg KR, Skyberg K, Kruse K, et al. The effects of intervention with local electrostatic air cleaners on airborne dust and the health of office employees. Indoor Air 2005;15:152-9. [PubMed]
- Mott JA, Meyer P, Mannino D, et al. Wildland forest fire smoke: health effects and intervention evaluation, Hoopa, California, 1999. West J Med 2002;176:157-62. [PubMed]
- Rigotti NA. Smoking cessation in patients with respiratory disease: existing treatments and future directions. Lancet Respir Med 2013;1:241-50. [PubMed]
- Tønnesen P, Carrozzi L, Fagerstrom KO, et al. Smoking cessation in patients with respiratory diseases: a high priority, integral component of therapy. Eur Respir J 2007;29:390-417. [PubMed]
- Chaudhuri R, Livingston E, McMahon AD, et al. Effects of smoking cessation on lung function and airway inflammation in smokers with asthma. Am J Respir Crit Care Med 2006;174:127-33. [PubMed]
- He QQ, Wong TW, Du L, et al. Nutrition and children’s respiratory health in Guangzhou, China. Public Health 2008;122:1425-32. [PubMed]
- Antova T, Pattenden S, Nikiforov B, et al. Nutrition and respiratory health in children in six Central and Eastern European countries. Thorax 2003;58:231-6. [PubMed]
- Romieu I. Nutrition and lung health. Int J Tuberc Lung Dis 2005;9:362-74. [PubMed]
- Hu J, Jiang X, Mao C, et al. The effect of air disinfection of the compound xiangai aerosol on particle space. J Hunan Normal Univ 2012;9:88-90. (Med Sci).
- Wang C, Cao B, Liu QQ, et al. Oseltamivir compared with the Chinese traditional therapy maxingshigan-yinqiaosan in the treatment of H1N1 influenza: a randomized trial. Ann Intern Med 2011;155:217-25. [PubMed]
- Guo R, Pittler MH, Ernst E. Herbal medicines for the treatment of COPD: a systematic review. Eur Respir J 2006;28:330-8. [PubMed]