Uniportal versus three-port video-assisted thoracoscopic surgery for spontaneous pneumothorax: a meta-analysis
Introduction
Pneumothorax has been described as a situation in which air is inserted into the pleural space. Open thoracotomy and video-assisted thoracoscopic surgery (VATS) are the main surgical treatments for pneumothorax. Open thoracotomy with pleurectomy was once used as the gold standard technique as recent as 2003 (1). The treatment of spontaneous pneumothorax has been developed from open thoracotomy to VATS over recent decades. Because of the lesser invasion, compared with open thoracotomy, conventional VATS has been clearly shown to offer greater advantages in regard to postoperative stay, operative time, length of postoperative drainage and postoperative pain (2-4). However the recurrence and residual neurological symptoms (including paresthesia, postoperative pain) still frequently occurred in this minimally invasive surgery (5-8). The main reason for postoperative pain may be injury to the intercostal nerves, as open thoracotomy usually requires one large incision or costal resection, and conventional VATS usually requires one small incision for the scope and multiple small incisions, to complete the procedure of dissection, resection, and grasping.
Since single-incision thoracoscopic surgery (SITS) for pulmonary wedge resection to treat pneumothorax was first reported by Yamamoto et al. in 1998 (9), sympathectomy, pulmonary resection, bronchial sleeve lobectomy, and bronchial reconstructive surgery have been performed via uniportal VATS (10-14). This offers another treatment option for spontaneous pneumothorax. With the application of uniportal VATS for spontaneous pneumothorax in a retrospective study, Huang et al. reported that the uniportal VATS group had a better outcomes in terms of operative time, intraoperative blood loss, and postoperative pain, but worse outcomes in regard to chest tube drainage time, postoperative length of hospital stay, postoperative leakage and recurrence than three-port VATS group (15). Uniportal VATS appears to have several disadvantages, such as limitation of the visual field, difficulty of use of VATS instruments, and ergonomic discomfort. The safety and feasibility of uniportal VATS seems to be controversial. Jutley et al. reported that uniportal VATS had an advantage in the reduction of postoperative pain and paresthesia compared to three-port VATS (16). However this was not reported by Yang et al. (17). These studies yielded different results. We performed the first meta-analysis to combine these comparative outcomes during the perioperative period, and investigate the safety, feasibility and advantages of uniportal VATS.
Materials and methods
Literature search strategy
A research for relevant publications was conducted in the Cochrane Library, PubMed, EMBASE, Web of Science, China National Knowledge Infrastructure (CNKI), Wanfang Data databases, and CQVIP, from their date of publication to April 2015. The search strategy used “uniportal video-assisted thoracoscopic surgery”, “single-port video-assisted thoracoscopic surgery”, “three-port video-assisted thoracoscopic surgery”, “spontaneous pneumothorax”, and ”pneumothorax” as key words or MeSH terms. We also collected the relevant references of all retrieved articles and conducted further searches.
Criteria for inclusion and exclusion
Eligible studies included the following criteria: (I) the studies evaluated the effect of uniportal VATS versus three-port VATS; (II) human-based studies with spontaneous pneumothorax; (III) studies were published in English and Chinese; (IV) studies were limited to RCT, case-control or cohort studies; (V) date on one of the outcomes [mortality, complications, recurrence, postoperative stay, operative time, length of postoperative drainage, paresthesia, visual analogue pain score (VAS) and patients satisfaction scale (PSS)] was provided. The exclusion criteria were as follows: (I) studies published in a language other than English or Chinese; (II) nonhuman-bases studies, studies without controllable patients, overlapping studies, case reports, letters, reviews or meta-analyses; (III) studies in which the necessary data were not provided.
Data extraction
Two investigators (Shi-Lei Qin, Yan-Long Yang) independently performed the assessment and data extraction using the author, year of publication, number of patients, age, gender, affected side, mortality, complications, recurrence, operative time, postoperative stay, length of postoperative drainage, paresthesia, VAS, PSS, and duration of follow-up. We contacted the authors if these data were missing or incomplete in their publications. Disagreements were resolved by discussion and adjudication by a senior investigator (Lei Xian). The VAS was assessed according to Duncan (18).
Quality assessment
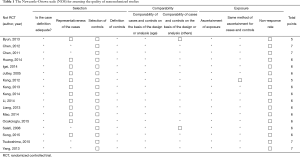
The quality of the included studies was independently assessed using the Newcastle-Ottawa scale (NOS) by two investigators (Shi-Lei Qin, Yan-Long Yang). Studies with five or more stars were defined as high quality studies. Disagreements were resolved by discussion.
Statistical analysis
The effective values of dichotomous variables or continuous variables were estimated by odds ratios (OR) or standardized mean differences (SMD) with their 95% CIs respectively. The Chi-square and I2 tests were used to evaluate statistical heterogeneity. The significance level of heterogeneity was fixed at P<0.10. When P>0.1 and I2<50%, heterogeneity was classified as acceptable (no heterogeneity: I2=0%−25%; low heterogeneity: I2=25%−50%; moderate heterogeneity: I2=50%−75%; high heterogeneity: I2=75%−100%). It was then tested using a fixed effects model. If I2>50%, a random effects model was conducted. For the source of heterogeneity, a sensitivity analysis of each study was used for secondary analysis. Publication bias was assessed by Egger’s and Begg’s test using STATA version 12.0 (Stata Corporation, College Station, TX). All P values were two-sided. A P value <0.05 was considered statistically significant. All statistical analysis was performed by Review Manager V.5.3 (The Cochrane Collaboration, Software Update, Oxford, UK) and STATA version 12.0.
Results
Study characteristics
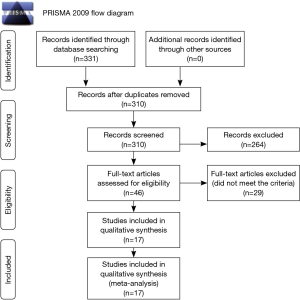
The present work followed the guidelines for systematic reviews and meta-analyses (PRISMA Flow Diagram). In total, 331 studies were identified by searching seven electronic databases. After removing duplicates and screening abstracts, the remaining potentially eligible for inclusion were further assessed by a screen of the full texts. After the exclusion of 29 studies that did not meet our inclusion criteria, 17 studies (15-17,19-32) were included in the final analysis. The process of article selection is summarized in Figure 1. Four studies were published in Chinese (15,22,27,28), and 13 studies were published in English (16,17,20,21,23-26,29-32). Table 1 shows the NOS quality scale and all eligible studies scored highly (with five stars or more). All 17 studies were retrospective case-control studies and included a total of 988 patients, of which 502 (50.8%) patients underwent uniportal VATS and 486 (49.2%) patients underwent three-port VATS. The main characteristics of all of the studies included are shown in Table 2.
Full table

Full table
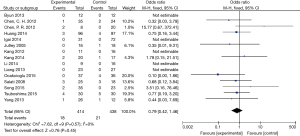
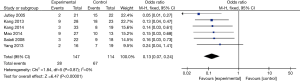
Perioperative mortality and recurrence
Seven studies (15,17,21,26,29,30) with 493 patients reported that no death occurred in either the uniportal or three-port VATS groups. Fifteen studies (15-17,19-25,27,29-32) assessed the postoperative recurrence rate, with a combined total of 852 patients included in this meta-analysis. No significant heterogeneity was detected (P=0.57, I2=0%). A Fixed effects model was selected. There was no significant difference between the uniportal and three-port VATS groups (OR=0.79; 95% CI: 0.42 to 1.46; P=0.45). However the recurrence rates of the uniportal VATS groups seemed to be lower than that of the three-port VATS groups (uniportal vs. three-port: 4.34% vs. 4.79%). The results are summarized in Figure 2.
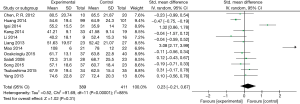
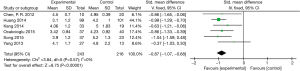
Operative time
Twelve studies (15,17,21-23,26-32) included comparable data on operative time with a combined total of 800 patients included in this meta-analysis. The mean of operative times of the uniportal and three-port VATS groups were 61.29 vs. 59.04 min, respectively. High heterogeneity was detected between the uniportal and three-port VATS groups (P<0.00001; I2=88%). A random effects model was used, and there was no significant difference between the uniportal and three-port VATS groups (SMD =−0.23; 95% CI: −0.21 to 0.67; P=0.31). The results are summarized in Figure 3.
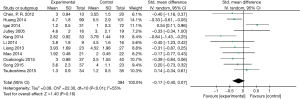
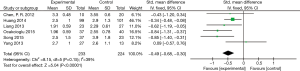
Length of postoperative drainage
A total of 11 studies (15,16,20,22,23,26-29,31,32) included comparable data on length of postoperative drainage, with a combined total of 744 patients included in this meta-analysis. The mean lengths of postoperative drainage for the uniportal and three-port VATS groups were 3.29 and 3.44 days, respectively. Moderate heterogeneity was observed among these studies (P=0.01; I2=55%). A random effects model was used, and no significant difference between the uniportal and three-port VATS groups was found (SMD =−0.17; 95% CI: −0.40 to −0.07; P=0.16). The results are summarized in Figure 4.
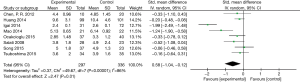
Postoperative hospital stay
Eight studies (15,21,23,28-32) yielded comparable data on postoperative hospital stay with a combined total of 635 patients included in this meta-analysis. The heterogeneity was significant (P<0.00001; I2=86%), and a random effects model was used. This meta-analysis suggested that the uniportal VATS groups were significantly associated with shorter postoperative hospital stay compared to the three-port VATS groups (SMD =−0.58; 95% CI: −1.04 to −0.12; P=0.01). However, the mean of lengths of postoperative hospital stay in the uniportal VATS groups were shorter by no more than one day than in the three-port VATS groups (5.71 vs. 5.84 days). Thus we still concluded that there was not great clinical difference between the two groups in terms of length of postoperative hospital stay. The results are summarized in Figure 5.
Paraesthesia
Six studies (16,17,25,26,28,30) included comparable data on paresthesia with a combined total of 261 patients included in this meta-analysis. The rates of paresthesia in the uniportal and three-port VATS groups were 19.04% and 58.77%, respectively. No significant heterogeneity (P=0.87; I2=0%) was seen in the fixed effects model. This meta-analysis suggested that the uniportal VATS groups were significantly associated with a lower rate of paresthesia compared to the three-port VATS groups (OR=0.13; 95% CI: 0.07 to 0.24; P<0.00001). The results are summarized in Figure 6.
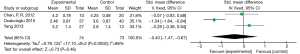
Postoperative pain
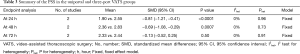
The VAS at 24 h, 48 h and 72 h were assessed for postoperative pain in 6, 3 and 6 studies, respectively. The mean VAS at 24 h, 48 h, 72 h in the uniportal vs. three-port VATS groups were 3.57 vs. 4.49, 2.97 vs. 3.63, 2.41 vs. 2.91, respectively.
Heterogeneity was acceptable in terms of VATS at 24 h and 72 h (VAS at 24 h: P=0.57, I2=0%; VAS at 72 h: P=0.15, I2=39%). A fixed effects model was selected for a meta-analysis, which indicated that the uniportal VATS groups were significantly associated with lower VAS at 24 h and 72 h when compared to the three-port VATS groups (VAS at 24 h: SMD =−0.87; 95% CI: −1.07 to −0.68; P<0.00001; VAS at 72 h: SMD =−0.49; 95% CI: −0.68 to −0.30; P<0.00001). The results are showed in Figures 7,8.
However, the heterogeneity was unacceptable in terms of VATS at 48 h (P=0.0002; I2=88%), and a random effects model was selected. There was no significant difference in the VAS at 48 h between the two VATS groups (SMD =−0.40; 95% CI: −1.47 to 0.67; P=0.46). After performing of sensitivity analysis, one study was excluded (29). Heterogeneity was not found (P=0.49; I2=0%), and a fixed effects model was selected. However, a statistical difference was not-found (SMD =0.13; 95% CI: −0.37 to 0.63; P=0.62). The results were summarized in Figure 9.
Patients satisfaction scale (PSS)
Only two studies (21,29) provided comparable data on PSS with a combined total of 107 patients included in this meta-analysis. Summary statistics found that the mean of PSS at 24 h, 48 h and 72 h in the uniportal vs. three-port VATS groups was 1.90 vs. 2.55, 2.36 vs. 2.83, 2.33 vs. 2.44, respectively. There was no heterogeneity between the uniportal and three-port VATS groups (PSS at 24 h: P=0.96, I2=0%; at 48 h: P=0.73, I2=0%; at 72 h: P=0.91, I2=0%), so a fixed effects model was selected. This meta-analysis suggested that the uniportal VATS groups had a significantly lower PSS at 24 h and 48 h compared to the three-port VATS groups (at 24 h: SMD =−0.81; 95% CI: −1.21 to −0.41; P<0.0001; at 48 h: SMD =−0.69; 95% CI: −1.08 to −0.29; P=0.0007). However, there was no significant differ ence between the uniportal and three-port VATS groups in terms of PSS at 72 h (SMD= −0.13; 95% CI: −0.52 to −0.25; P=0.50). The results were summarized in Table 3.
Full table
Sensitivity analysis
To evaluate the influence of single studies and analyze the effects of heterogeneity on the pooled SMDs of operative time, length of postoperative drainage and hospital stay, we performed a sensitivity analysis by estimating the average OR in the absence of each study.
For the operative time, two studies (23,28) influenced the comparable outcome in the sensitivity analysis of each study. Heterogeneity was acceptable (P=0.21, I2=25%). Thus, a fixed effects model was selected. There was a significant difference between these two groups (SMD= −0.17; 95% CI: −0.32 to −0.01; P=0.04). In both studies excluded after sensitivity analysis, the operative time in the uniportal VATS groups was longer than that in the three-port VAST groups (uniportal vs. three-port: 1.8±0.1 h vs. 1.3±0.2 h, and 55.2±15.5 min vs. 35.9±14.0 min). The most likely reason for the high heterogeneity of operative time in one study was that the suture was used in the uniportal VATS groups, while endoscopic staplers were used in the three-port VATS groups (28). The cause of high heterogeneity in another excluded study may have been a change to multi-DOF forceps by operators and assistants.
Regarding length of postoperative drainage, after excluding two studies (23,28) based on sensitivity analysis, heterogeneity was non-existent among the remaining 6 studies (P=0.76, I2=0%), and a significant difference was found (SMD= −0.23; 95% CI: −0.41 to −0.05; P=0.01).
For postoperative hospital stay, sensitivity analysis of each study showed that, there was no heterogeneity (P=0.32, I2=14%) and a significantly difference was found (SMD= −027; 95% CI: −0.42 to −0.11; P=0.0009) between the uniportal and three-port VATS groups in summarized data from the 10 studies, except for one study (23).
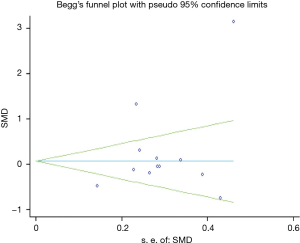
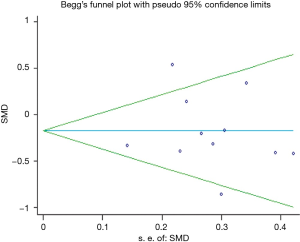
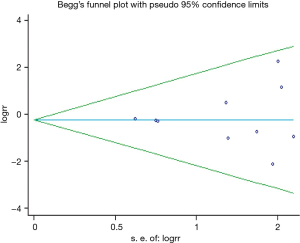
Publication bias
Publication bias was assessed using Egger’s and Begg’s test in STATA version 12.0. No publication bias in the comparison of recurrence (Egger P=0.67; Begg P=0.72), operative time (Egger P=0.24; Begg P=0.84), or length of postoperative drainage (Egger P=0.72; Begg P=1.00) was detected. And Egger’s and Begg’s test for the other endpoints, which were evaluated by fewer than 10 studies, were not performed. The results are summarized in Figures 10-12.
Discussion
Uniportal VATS was described as inserting the video thoracoscope and two forceps through a single incision. Uniportal VATS was performed under general anesthesia using one-lung ventilation with the patient in lateral recumbency. The size of the skin incision should be associated with the size of the forceps, thoracoscope and trocar. Most publications reported that the skin incisions made was 1.5−3.0 cm in length through the 4th−7th intercostal space on the mid-axillary, anterior or posterior axillary line. Most surgeons preferred a wound protector or a trocar to fix on the incision window. We suggested that a rubber wound protector should be a better choice (31), due to the provision of an adequate space for operating, protection of intercostal tissue and prevention of nerve entrapment. Next, a 5- or 10-mm 30° or 0° thoracoscope and straight shaft forceps or multi-DOF forceps were required to perform lobectomy. Multi-DOF forceps, which allowed the surgeon to manipulate bullae or blebs on a different axis, could diminish this interference, which was caused by inadequate space for operating through the same incision. After checking for air leak and bleeding, one drainage tube was inserted through the incision. We concluded form these studies that, uniportal VATS was performed better with a wound protector to fix on the incision window, a multi-DOF forceps to operate, and staplers for lobectomy during the surgical procedure.
We conducted this meta-analysis to evaluate the evidence comparing uniportal to three-port VATS for spontaneous pneumothorax and to assess the advantages of uniportal VATS. This meta-analysis evaluated the mortality, recurrence, complications, postoperative stay, operative time, length of postoperative drainage, paresthesia, VAS, and PSS of in uniportal and three-port VATS in patients with spontaneous pneumothorax using the best evidence available to date. Compared to the three-port VATS groups, there was no significant difference in the uniportal VATS groups in terms of mortality, recurrence, postoperative stay, operative time, and length of postoperative drainage. This meta-analysis indicated that the uniportal VATS groups were significantly associated with lower paresthesia, postoperative pain, and higher patients satisfaction in the short-term.
The mortality rate was 0% as reported in both groups. Complications were reported in only 13/320 (4%) patients (six patients in the uniportal VATS groups and seven patients in the three-port VATS groups) in six studies(17,20,21,29-31), including two patients with wound infection, nine patients with air leak, and two patients with pleural effusion. No serious complications occurred. This meta-analysis indicated that using the uniportal VATS technique did not caused more deaths, complications or recurrences during the perioperative period. This uniportal VATS technique was as clinically safe as the three-port VATS technique and did not lend to a worse outcome.
This meta-analysis showed that uniportal VATS did not increase operative time, or prolong postoperative drainage or postoperative hospital stay comparing with three-port VATS. Theoretically, a smaller incision makes operation more difficulty. Based on the surgeons’ experiences, the operative time may be longer when they first begin using the technique. After adapting the technique and gaining more practice, the speed of the procedure accelerated quickly. For postoperative drainage, most studies reported bleeding and the flux of postoperative drainage could be ignored both in uniportal VATS groups and three-port VATS groups. This meant that uniportal VATS did not increase the risk of injury of to any vessels in the thoracic cavity, which may occur due to the difficulty of the uniportal VATS technique. These results showed that uniportal VATS was a safe and effective surgical approach for spontaneous pneumothorax, and did not pose an additional burden on hospital resources.
Residual neurological complications in the uniportal VATS groups were considered significantly lower than in the three-port VATS groups. Compared to the three-port VATS groups, the uniportal VATS groups showed significantly lower in incidences of paresthesia. Patients in the uniportal VATS groups suffered from less postoperative pain at 24 h and 72 h, but equal pain at 48 h. There was no significant difference between the uniportal and three-port VATS groups in the analysis for VAS at 48 h. One reason may be the limited amount of data which came from only three studies with a total of 147 patients. As three-port incisions caused more injuries to the intercostal nerves than uniportal incisions did, more residual neurological symptoms, such as paresthesia, post-operative pain, even sexual dysfunction (16), can be unrelenting and difficult to treat with analgesics. The included studies reported that the patients in the three-port VATS groups required more postoperative epidural or intravenous patient-controlled analgesia (PCA) treatment than those in the uniportal VATS groups. Short-term outcomes showed that residual paresthesia and pain were lower and patients satisfaction was higher in the uniportal VATS groups. These advantages of uniportal VATS would lead to being the preferred choice of surgeons’ and patients’ choices. With its popularity and application, uniportal VATS may be an alternative technique to three-port VATS. However a scientific, randomize trial with a large sample size is needed to investigate long-term outcomes.
The most common patient complaints were paresthesia and wound pain, which may be caused by injury to the intercostal nerves when the operative approach was chosen—either VATS or open thoracotomy—penetrates the intercostal space. To prevent these problems, we summarized the following strategies based on surgeons’ feedback: (I) single incision laparoscopic surgery (SILS) system combined with single-port technique was used as a novel method in uniportal VATS for treatment of pneumothorax (33). This SILS system, which was made of elastic elastomeric material, can diminish compression of the intercostal space. (II) A wound protector, which was used to fix on the incision window, may have a greater advantage in preventing postoperative pain than multi-incision trocar (31). (III) The 2-mm video-assisted endoscope, which was reported to be used in the two-port VATS procedure (34), is smaller than the 5-mm video-assisted thoracoscope, and could therefore be used with a single smaller incision, reducing injury to the intercostal nerves. (IV) Pre-emptive wound infiltration with a local anesthetic, which was reported to reduce postoperative pain in needlescopic VATS procedures for the treatment of palmar hyperhidrosis in a randomized trial (35), may be applied in uniportal VATS procedure. Blocking of the central sensitization may reduce wound pain. (V) Another uniportal VATS procedure, known as the subxiphoid technique (36), may not cause injury to the intercostal nerves because the incision is made on the subxiphoid area. This subxiphoid uniportal VATS technique may be an innovation in the single-incision approach.
In this meta-analysis, only two studies reported a conversion from uniportal VATS to three-port VATS. Chen et al. (21) reported only that the conversion from uniportal VATS to three-port VATS for hemostasis is difficult, but the number of conversions is not. Igai et al. (23) reported that only one patient required conversion to a three-port approach because of severe adhesion. To overcome these problems for surgeons who are new to uniportal VATS, we suggest that more practice for surgeons may lesd to fewer injuries, and well-selected patients should be considered.
Limitation
Despite having 17 case-control studies that compare uniportal VATS and three-port VATS, randomized controlled trials had not been conducted. Small sample size was another limitation in most studies. A multi-center study with large-sample-size has not yet been reported. For these reasons, heterogeneity existed in recurrence, operative time, length of postoperative drainage and length of postoperative hospital stay.
Conclusions
This paper is the first meta-analysis that compared uniportal with three-port VATS for spontaneous pneumothorax. The uniportal VATS technique neither increased mortality or recurrence rate nor prolonged the operative time, length of postoperative drainage or postoperative hospital stay. However, this new technique could reduce patients’ postoperative pain and paresthesia, and improve patients’ satisfaction. This meta-analysis indicates that the uniportal VATS is a safe, feasible and effective treatment for spontaneous pneumothorax. A reduction in paresthesia and post-operative pain were among the advantages of uniportal VATS.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Henry M, Arnold T, Harvey J, et al. BTS guidelines for the management of spontaneous pneumothorax. Thorax 2003;58 Suppl 2:ii39-52. [PubMed]
- Sawada S, Watanabe Y, Moriyama S. Video-assisted thoracoscopic surgery for primary spontaneous pneumothorax: evaluation of indications and long-term outcome compared with conservative treatment and open thoracotomy. Chest 2005;127:2226-30. [PubMed]
- Naunheim KS, Mack MJ, Hazelrigg SR, et al. Safety and efficacy of video-assisted thoracic surgical techniques for the treatment of spontaneous pneumothorax. J Thorac Cardiovasc Surg 1995;109:1198-203; discussion 1203-4. [PubMed]
- Goto T, Kadota Y, Mori T, et al. Video-assisted thoracic surgery for pneumothorax: republication of a systematic review and a proposal by the guideline committee of the Japanese association for chest surgery 2014. Gen Thorac Cardiovasc Surg 2015;63:8-13. [PubMed]
- Noh D, Lee S, Haam SJ, et al. Recurrence of primary spontaneous pneumothorax in young adults and children. Interact Cardiovasc Thorac Surg 2015;21:195-9. [PubMed]
- Passlick B, Born C, Sienel W, et al. Incidence of chronic pain after minimal-invasive surgery for spontaneous pneumothorax. Eur J Cardiothorac Surg 2001;19:355-8; discussion 358-9. [PubMed]
- Sihoe AD, Au SS, Cheung ML, et al. Incidence of chest wall paresthesia after video-assisted thoracic surgery for primary spontaneous pneumothorax. Eur J Cardiothorac Surg 2004;25:1054-8. [PubMed]
- Pagès PB, Delpy JP, Falcoz PE, et al. Videothoracoscopy versus thoracotomy for the treatment of spontaneous pneumothorax: a propensity score analysis. Ann Thorac Surg 2015;99:258-63. [PubMed]
- Yamamoto H, Okada M, Takada M, et al. Video-assisted thoracic surgery through a single skin incision. Arch Surg 1998;133:145-7. [PubMed]
- Rocco G, Khalil M, Jutley R. Uniportal video-assisted thoracoscopic surgery wedge lung biopsy in the diagnosis of interstitial lung diseases. J Thorac Cardiovasc Surg 2005;129:947-8. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [PubMed]
- Gonzalez-Rivas D, Fieira E, de la Torre M, et al. Bronchovascular right upper lobe reconstruction by uniportal video-assisted thoracoscopic surgery. J Thorac Dis 2014;6:861-3. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [PubMed]
- Huang LZ, Cao QD. Contrast research between single-port Video-assisted thoracoscopic surgery and traditional thoracoscope surgery for the treatment of spontaneous pneumothorax. Journal of Ningxia Medical University 2014;36:650-2.
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [PubMed]
- Duncan JA, Bond JS, Mason T, et al. Visual analogue scale scoring and ranking: a suitable and sensitive method for assessing scar quality? Plast Reconstr Surg 2006;118:909-18. [PubMed]
- Byun CS, Hwang JJ, Choi JH. Single-incision vats bullectomy with suture-lift method in primary spontaneous pneumothorax. Innovations Technology and Techniques in Cardiothoracic and Vascular Surgery 2013;8:145-6.
- Chen CH, Lee SY, Chang H, et al. The adequacy of single-incisional thoracoscopic surgery as a first-line endoscopic approach for the management of recurrent primary spontaneous pneumothorax: a retrospective study. J Cardiothorac Surg 2012;7:99. [PubMed]
- Chen PR, Chen CK, Lin YS, et al. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax. J Cardiothorac Surg 2011;6:58. [PubMed]
- Li CJ, Zhang M, Liu D, et al. Comparative analysis of standard three-port, one single utility port and uniportal VATS for spontaneous pneumothorax in young patients. Modern Instruments & Medical Treatment 2014;20:27-9.
- Igai H, Kamiyoshihara M, Ibe T, et al. Single-incision thoracoscopic surgery for spontaneous pneumothorax using multi-degrees of freedom forceps. Ann Thorac Cardiovasc Surg 2014;20:974-9. [PubMed]
- Kang DK, Min H, Hwang YH, et al. Clinical feasibility of single-port video-assisted thoracoscopic surgery using alexis(registered trademark) wound retractor for primary spontaneous pneumothorax. Interactive Cardiovascular and Thoracic Surgery 2012;15:S143.
- Kang DK, Min HK, Hwang YH, et al. The results of single-port video-assisted thoracic surgery for primary spontaneous pneumothorax. Innovations Technology and Techniques in Cardiothoracic and Vascular Surgery 2013;8:145.
- Kang do K, Min HK, Jun HJ, et al. Early outcomes of single-port video-assisted thoracic surgery for primary spontaneous pneumothorax. Korean J Thorac Cardiovasc Surg 2014;47:384-8. [PubMed]
- Liang Z, Chen J, Lin LR, et al. The effect comparison of the treatment for primary pneumothorax: uniport vs three-port VATS. Journay of GuangDong Medical College 2013;31:379-80.
- Mao Y, Lin Q, Cen HF, et al. Suture hole thoracoscopicin treatment of spontaneous pneumothorax. China Modern Doctor 2014;52:34-6.
- Ocakcioglu I, Alpay L, Demir M, et al. Is single port enough in minimally surgery for pneumothorax? Surg Endosc 2015. [Epub ahead of print]. [PubMed]
- Salati M, Brunelli A, Xiumè F, et al. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg 2008;7:63-6. [PubMed]
- Song IH, Lee SY, Lee SJ. Can single-incision thoracoscopic surgery using a wound protector be used as a first-line approach for the surgical treatment of primary spontaneous pneumothorax? A comparison with three-port video-assisted thoracoscopic surgery. Gen Thorac Cardiovasc Surg 2015;63:284-9. [PubMed]
- Tsuboshima K, Wakahara T, Matoba Y, et al. Single-incision thoracoscopic surgery using a chest wall pulley for lung excision in patients with primary spontaneous pneumothorax. Surg Today 2015;45:595-9. [PubMed]
- Gigirey Castro O, Berlanga González L, Sánchez Gómez E. Single port thorascopic surgery using the SILS tool as a novel method in the surgical treatment of pneumothorax. Arch Bronconeumol 2010;46:439-41. [PubMed]
- Kim BY, Oh BS, Park YK, et al. Microinvasive video-assisted thoracoscopic sympathicotomy for primary palmar hyperhidrosis. Am J Surg 2001;181:540-2. [PubMed]
- Sihoe AD, Manlulu AV, Lee TW, et al. Pre-emptive local anesthesia for needlescopic video-assisted thoracic surgery: a randomized controlled trial. Eur J Cardiothorac Surg 2007;31:103-8. [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. [PubMed]