Physiotherapy for enhanced recovery in thoracic surgery
Introduction
Physiotherapy is a fundamental component of Enhanced Recovery Programmes (ERP) (1,2). The importance of maximising the patient’s condition prior to surgery, minimising post-operative complications and returning the patient to a functional level of quality of life are all core aspects of what physiotherapy is aiming to achieve in an ERP (1,2).
Physiotherapy prior to ERP
The physiotherapy management of patients undergoing thoracic surgery prior to the introduction of the ERP was an historical based service that had many variations in practice within it, as the service was based on what the practitioner assessed as needed. All patients undergoing Thoracic surgery were assessed day one after surgery regardless of their risk for developing post-operative pulmonary complications (PPC). The patients were given thoracic expansion exercises, taught a supported cough, taught shoulder exercises and marched on the spot for varying amounts of time normally once a day and only Monday–Friday. However barriers to early mobilisation existed (3) which prevented ERP principles of early mobilisation being used. There was a strong reliance by patients for the staff to do things for them rather than being encouraged to be independent. Only once a patient had developed a PPC were they then seen more frequently within the week and over the weekend. Techniques such as Intermittent Positive Pressure Ventilation (IPPV) were then used alongside the other treatments. Prior to discharge from hospital patients were provided with a simple discharge booklet that advised on the amount of exercise they should aim to do to aid their recovery, alongside advice on wound support and precautions for arm use for 6–8 weeks to protect from wound dehiscence.
Physiotherapy post implementation of the ERP
To design the physiotherapy service for the ERP the evidence was reviewed and then evolved to best suit the Thoracic surgery patient population at our institution (1,2). In conjunction with the other disciplines of the multi-disciplinary team (MDT) the specific core components of an ERP were designed with the physiotherapy team focusing on an early post-operative mobilisation plan and self-directed pre-operative exercise programme (4).
Screening tool for physiotherapy treatment
To release resources to support the change of practice to an ERP a physiotherapy screening tool was developed to assess which patients would be the highest risk for developing PPC’s and which patients were low risk. The criteria patients are assessed against are:
- Has the patient had a thoracotomy?
- Has the patient had lung resection/chest wall/pectus correction or decortication surgery?
- Has the patient got a diagnosed lung disease? e.g., COPD.
- Is the patient a current smoker or stopped in the last 2 months?
- Does the patient have a pre-existing mobility problem?
If any of the questions are answered ‘yes’ then the patient would be screened in for post-operative physiotherapy treatment. Otherwise the patient would be classed as a low risk patient and then provided with pre- and post-operative information only. An example of a low risk patient would be a non-smoking patient with no history of lung disease undergoing a talc pleurodesis for a pneumothorax. This tool released time for physiotherapy staff from low risk patients so that an increased service could be introduced for the high risk patients. Any patient that was screened out could be referred for physiotherapy if the medical or rapid response team deemed it necessary.
Pre-operative physiotherapy
To optimise patients for surgery a detailed information booklet was designed along with a DVD for all patients to receive at the pre-operative assessment clinic, this in line with ERP principles that patients who are educated prior to elective surgery have less anxiety (5), improved pain (6) and patient satisfaction (7). As part of this booklet a detailed pre-operative home based pulmonary rehabilitation programme was included to optimise patient’s physical function prior to surgery so as to minimise the physiological effect of the surgery and improve outcomes. Pre-operative rehabilitation for Thoracic surgery patients has been shown to be beneficial and safe (4,8). A diary function was also included for patients to track their progress prior to admission (9).
Post-operative physiotherapy
The structure of the physiotherapy service for Thoracic surgery patients changed from a 5-day service once a day predominantly prior to ERP, to a 7-day service with two treatments sessions a day as required with the ERP for high risk PPC patients and low risk patients being screened out for needing therapy.
Patients that screen in for therapy are assessed either day 0 or day 1 post-operatively by a physiotherapist and can be mobilised within hours of their surgery (10). Patients are seen twice a day until they are able to independently exercise and perform chest clearance. The fundamental cornerstone of the post-operative physiotherapy management is early mobilisation as documented in the ERP principles (1,2). Post-operatively each patient has a standardised mobilisation plan that requires a minimum of 60 m be walked four times on day 1, 80 m on day 2, 100 m on day 3 and then continuing or increasing this as able throughout the rest of their admission. The patients are encouraged to mobilise at a pace were they achieve a breathlessness of 3-4 on the Borg ten point scale (11). The patient is encouraged to record their activity in the diary section of the information booklet which sets out what they should be achieving each day of their admission. An important aspect to patients being mobile was the introduction of portable suction drains (12) which are used as standard within the ERP rather than drains attached to wall suction which mean the patient is limited to their bed space only, which reduces the patient’s level of activity. If a patient is unable to leave the bed space then portable exercise bikes or step ups are used to ensure the patient is benefiting from post-operative exercise.
Posture and arm exercises are also used each day as they have been shown to reduce shoulder dysfunction post-operatively and regain functional activities of daily living (13). These are also recorded in the patient diary and need to be performed 4 times daily.
Another important aspect of the physiotherapy post-operative care is working closely with the MDT to ensure adequate pain relief for the patient. A now standard component of each physiotherapy session is a pain assessment so that early proactive steps can be taken to optimise the patient’s analgesia requirements. As part of this assessment each patient is taught a supported cough to mechanically support the wound to reduce pain and improve confidence in coughing post-operatively.
The use of airway clearance techniques and lung recruitment techniques such as active cycle of breathing (ACBT), IPPV, cough assist, manual techniques and Forced Expiratory Technique (FET) are used as clinically indicated.
The use of incentive spirometry (IS) remains widespread in the post-operative physiotherapy management of major surgical patients, however, several studies and meta analyses have shown no additional benefit to the use of IS compared with standard physiotherapy of mobilisation, breathing exercises and coughing at reducing the incidence of PPC’s or reducing hospital length of stay (14-17). The additional cost of IS devices based on no clinical evidence is unnecessary when the same results can be achieved without their use. IS is not used by the physiotherapy team at Papworth in line with the best available evidence.
A fundamental principle of the Papworth Physiotherapy ERP for thoracic surgery patients is empowering the patient to take ownership and be involved in their care and recovery. A core aspect of this is the patient using their patient diary to guide themselves in what they should be doing and monitoring their own progress.
In preparing for discharge from hospital patients are checked that they are independently mobile back to at least their baseline functional level and are independent with chest clearance techniques, shoulder and postural exercises. A detailed post-operative exercise programme based on the principles of pulmonary rehabilitation is detailed in the patient’s diary for them to follow after discharge from hospital to progress the patient back to a fully functional quality of life.
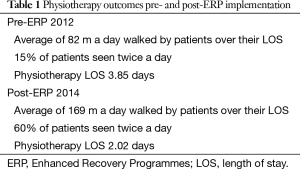
As part of the implementation of the ERP the physiotherapy team audited the activity levels of patients and physiotherapy length of treatment pre- and post-ERP starting, the Table 1 highlights the main audit findings.
Full table
The physiotherapy team continue to review this service and are currently working on publishing the screening tool for Thoracic surgery patients.
Acknowledgements
Mr. Marco Scarci for his ambition and determination to make the Enhanced Recovery Programme such a success. Papworth Hospital NHS Foundation Trust for providing the resources required to set up the Enhanced Recovery Programme and the Physiotherapy Department for their support and guidance whilst the Enhanced Recovery Programme was being developed.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- The Royal College of Anaesthetists. Guidelines for patients undergoing surgery as part of an Enhanced Recovery Programme (ERP). June 2012. Available online: https://www.rcoa.ac.uk/system/files/CSQ-ERP-Guide2012.pdf
- NHS. Enhanced Recovery Partnership Programme. Delivering enhanced recovery—Helping patients to get better sooner after surgery. 31 March 2010. Available online: http://www.westhertshospitals.nhs.uk/enhanced_recovery/documents/pdf/ERPP%20Implementation%20Guidance.pdf
- Irish Thoracic Society Annual Scientific Meeting 2014. Irish Journal of Medicine Science 2014;183:Suppl 11. Available online: http://link.springer.com/journal/11845/183/11/suppl/page/1
- Nagarajan K, Bennett A, Agostini P, et al. Is preoperative physiotherapy/pulmonary rehabilitation beneficial in lung resection patients? Interact Cardiovasc Thorac Surg 2011;13:300-2. [PubMed]
- Kiyohara LY, Kayano LK, Oliveira LM, et al. Surgery information reduces anxiety in the pre-operative period. Rev Hosp Clin Fac Med Sao Paulo 2004;59:51-6. [PubMed]
- Egbert LD, Battit GE, Welch CE, et al. Reduction of postoperative pain by encouragement and instruction of patients. A study of doctor-patient rapport. N Engl J Med 1964;270:825-7. [PubMed]
- Lee A, Gin T. Educating patients about anaesthesia: effect of various modes on patients' knowledge, anxiety and satisfaction. Curr Opin Anaesthesiol 2005;18:205-8. [PubMed]
- Levett DZ, Grocott MP. Cardiopulmonary exercise testing, prehabilitation, and Enhanced Recovery After Surgery (ERAS). Can J Anaesth 2015;62:131-42. [PubMed]
- Mitchell J. Guideline for patient information on enhanced recovery in thoracic surgery. Lung Cancer 2015;87:S39.
- Kaneda H, Saito Y, Okamoto M, et al. Early postoperative mobilization with walking at 4 hours after lobectomy in lung cancer patients. Gen Thorac Cardiovasc Surg 2007;55:493-8. [PubMed]
- Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982;14:377-81. [PubMed]
- Szántó Z, Kovács O. Digital drainage system in the postoperative treatment of thoracic surgical patients. Magy Seb 2012;65:19-23. [PubMed]
- Li WW, Lee TW, Yim AP. Shoulder function after thoracic surgery. Thorac Surg Clin 2004;14:331-43. [PubMed]
- Agostini P, Naidu B, Cieslik H, et al. Effectiveness of incentive spirometry in patients following thoracotomy and lung resection including those at high risk for developing pulmonary complications. Thorax 2013;68:580-5. [PubMed]
- Gosselink R, Schrever K, Cops P, et al. Incentive spirometry does not enhance recovery after thoracic surgery. Crit Care Med 2000;28:679-83. [PubMed]
- Carvalho CR, Paisani DM, Lunardi AC. Incentive spirometry in major surgeries: a systematic review. Rev Bras Fisioter 2011;15:343-50. [PubMed]
- Overend TJ, Anderson CM, Lucy SD, et al. The effect of incentive spirometry on postoperative pulmonary complications: a systematic review. Chest 2001;120:971-8. [PubMed]


