Unidirectionally progressive resection of lower left lung carcinoma under video-associated thoracoscopy
Introduction
Video-assisted lobectomy has been verified as the standard treating protocol for lung carcinoma by National Comprehensive Cancer Network (NCCN) [2006], and American College of Chest Physicians (ACCP) [2007] separately. Up till now there are mainly two ways of video-assisted lobectomy, one is the traditional minimally invasive surgery procedure that calls for an order of pulmonary fissure, artery, vein, and finally bronchus to remove the lobe. Dr. Jianxing He has prior initiated traditional minimally invasive thoracotomies in china mainland in 1994. As for unidirectional minithoracotomy, which was pioneered in china mainland by Dr. Lunxu Liu (1), would have no need to flip the lobe.
Unidirectionally video-assisted thoracoscopy is made to progress from the anterior to the posterior for the resection of upper or lower lobe, and from inferior to superior for the lower lobe. Being specific, when dealing with hilum structure, an order of pulmonary vein, bronchus, artery, fissure will be taken. Resection of disease lobe combined with mediastinal lymph node dissection is the standard operation for radical cure treatment of non-small cell lung carcinoma. Compared with the traditional open-thoracic surgery, there would be smaller incisions, convenient operation, and less damage. Surgeons do not have to cut off rib(s), and could open up and close the chest rapidly, and patients lose less blood during operation, experiences less post-operational incision pain, and face less risk of postoperative complications, such as pneumonia, atelectasis, arrhythmia etc. This technology is also proofed more beneficial for postoperative recovery than the traditional way by the researches of Villamizar et al. (2). And in multiple studies, the long-term outcomes of video-assisted thoracic surgery (VATS) show no inferior to open-thoracic surgeries (3,4).
When applying the technique, double-lumen intubation is a must.
There is a significant difference between video-assisted lobectomy and small-incision assisted thoracoscopy. That is the former doesn’t call for an open-up in intercostal space, nor manipulations under straight look. Furthermore video-assisted lobectomy reduces postoperative pains greatly than small-incision assisted thoracoscopy. And if the operation depends on straight-looking manipulations excessively, the video-assisted technology would somehow become a kind of “torchlight”. Compared with conventional long thoracotomy or small-incision assisted thoracoscopy, VATS put the patients under the favorable conditions that fit in postoperative treatments like chemotherapy, radiotherapy etc. without reducing curing treatment.
Case presentation
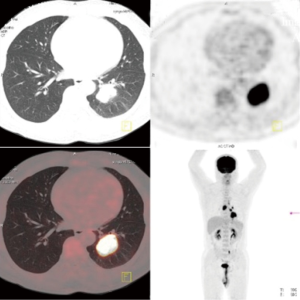
A 50-year-old male was hospitalized due to repeated coughing lasting longer than a year. He had no history of smoking. The positron emission tomography-computed tomography (PET-CT) (Figure 1) shows a hypermetabolic mass with a 5.3 cm × 3.4 cm × 5.7 cm diameters, the SUVmaxshows 18.2, SUVave 7.6; benign nodules were spotted in right upper lobe posterior segment and the left lingual segment, there were some obsolete lesions in left lingual segment. Multiple lymph nodes in left pulmonary hilum and mediastinum are found enlarged and hypermetabolic.
The diagnosis of left lower pulmonary carcinoma is made. Considering the auxiliary examinations, unidirectionally thoracoscopic resection of left lower lung with lymphadenectomy was finally performed in the order of inferior pulmonary veins → left inferior bronchus → left inferior pulmonary artery and the underdevelopment fissure in turn.
Procedure of key surgical positions
Unidirectionally progressive resection under video-assisted thoracoscopy is adopted in the operation, i.e., operate right below the operation port, and dissect the tissue to be removed from the surface. Follow a single direction to advance, and expose, dissociate, and divide in the order of pulmonary vein, bronchus, artery, fissure. Upon that the target structure will expose itself effortlessly after the previous anatomic structure is disposed, having no need to circumvent a particular structure to isolate the deeper-located tissue.
This protocol basically work on the pedicle area of the lung, making it apt to resect huge mass under thoracoscopy. Flips and overturns of lobar tissue hardly appear in the process, diminishing artificial interventions on pulmonary tissues and blood supply, which abates pains, muscle damages, and complication incidences postoperatively.
During operation the surgeon could avoid dissociate vessels in parenchyma or underdeveloped pulmonary fissure because dissection of pulmonary fissure is unnecessary in this method.
In summary unidirectionally progressive lobectomy conforms the requirements of tumor resection better than the other ways technically.
Still-remaining debates about VATS are focusing on whether its dissection of mediastinal lymph nodes is as complete as the open thoracotomy’s. Regarding our practicing experience, total mediastinal lymph node dissection is safe and feasible, for the 2nd, 3rd, 4th, 7th–10th lymph node group are resectable in the right and 5th–10th group are resectable in the left.
Unidirectionally progressive lobectomy has been applied to different lobes successfully (5-7). Our program believes this technology would be applied to otherwise lobes, and also mini-invasive pneumonectomies. We are looking forward that the unidirectionally progressive lobectomy will gain more test and spread in the clinic field.
The case is depicted as follow. Your precious advice is grated.
Operation process
General anesthesia is adopted through double-lumen endotracheal intubation, one-lung ventilation on the contralateral, and intravenous injection. Double-lumen intubation is a key step for the operation because it is mandatory to collapse the lung on the side of thoracoscopic surgery to allow smooth access.
The patient took a 90 degree decubitus on his contralateral side.
The operative incisions: the observation port was made in the mid-axillary line of the 7th intercostal section, a 2nd horizontal incision of 4 cm as the main operation port at the 4th intercostal space between the anterior axillary line and the midclavicular line, and a 3rd incision of 1.5 cm as the secondary operation hole at the 9th intercostal space between the axillary line and the bottom scapular line. The surgeons were on the ventral side of the patient, and operated with endoscope apparatus in front of the monitor screen.
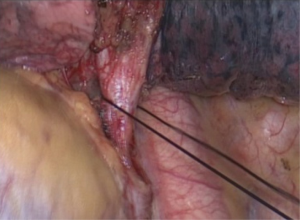
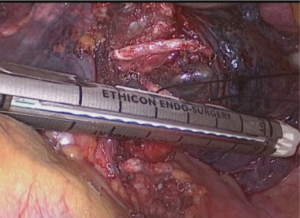
The main surgery procedure (Figure 2) is divided into four steps and each step is illustrated below.
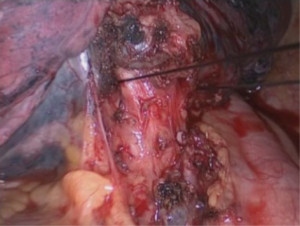
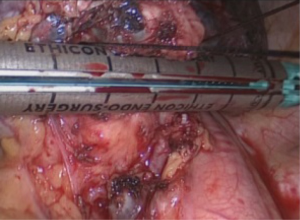
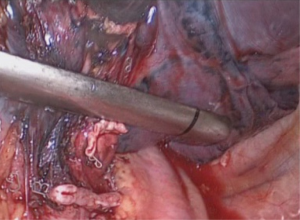
The left inferior pulmonary vein was first isolated (Figures 3,4). After that proceed to the bronchus (Figures 5,6) without flipping the lobe. Then resect the inferior pulmonary artery (Figures 7,8). Finally deal with the pulmonary fissure and remove the lobe outside (Figures 9-11).

Comments
VATS resection of lung cancer is superior to the tradition fashion in that it is performed with incisions as small as only 3 to 5 cm, avoiding rib retraction and extensive transection of chest muscles. Thus a better protection of the neuromuscular system, significantly reduced postoperative pain, blood loss, as well as the incidence of postoperative complications are expected.
Still-remaining debates about VATS are focusing on whether its dissection of mediastinal lymph nodes is as complete as the open thoracotomy’s. Regarding our practicing experience, total mediastinal lymph node dissection is safe and feasible, for the 2nd, 3rd, 4th, 7th–10th lymph node group are resectable in the right and 5th–10th group are resectable in the left. Empirically-speaking, the dead spot-free coverage and certain amplification of the surgical field in VATS allow further thorough lymph node dissection compared with traditional open surgery.
Obviously enlarged lymph nodes often indicate the presence of metastases, which are associated with a high risk of capsule rupture and potential tumor seeding during thoracoscopic resection. Therefore, we do not recommend this surgical technique for patients with known significant enlargement of hilar or mediastinal lymph nodes, or as confirmed by preoperative PET-CT or CT.
Besides thorough lymph nodes resection, a difficulty in managing rupture of blood vessels is also a major concern of VATS. The unidirectional procedure of VATS lobectomy has shaken off the shackles of traditional process, making it easier to perform the lobectomy under thoracoscopy in a smooth and simple way. The unidirectional thoracoscopic lobectomy is performed within the hilar soft tissue structure following a single direction without entering the lung parenchyma, or tearing or cutting the lung tissue, so that little injury is brought to the parenchyma. At the final step of fissure resection, any bronchial and pulmonary vascular interference has been removed, making it simple to cutting the tissue with a linear stapler, which significantly reduces the risk of postoperative air leaks. In particular, direct resection with the stapler is possible for patients with a poorly developed fissure, in which separation of the pulmonary artery is not necessary. This can significantly reduce blood loss and surgical time, and lower the difficulty of operation. The unidirectional thoracoscopic lobectomy also reduces lung injury by avoiding repeated flipping of the lung tissue.
Acknowledgements
Funding: Sub-subject of nationally supportive subject—Research and Application of Appropriate Technology in Control and Prevention of Common Diseases in Xinjiang Autonomous Region (No. 2013BAI05B02); “Twelfth Five Year” major drug discovery projects of China (No. 2012zx09101103).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Liu L, Che G, Pu Q, et al. Lobectomy by video-assisted thoracic surgery unidirectionally. Chinese Journal of Thoracic and Cardiovascular Surgery 2008;24:156-8.
- Villamizar NR, Darrabie MD, Burfeind WR, et al. Thoracoscopic lobectomy is associated with lower morbidity compared with thoracotomy. J Thorac Cardiovasc Surg 2009;138:419-25. [PubMed]
- Flores RM, Park BJ, Dycoco J, et al. Lobectomy by video-assisted thoracic surgery (VATS) versus thoracotomy for lung cancer. J Thorac Cardiovasc Surg 2009;138:11-8. [PubMed]
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [PubMed]
- Cai K, Ren P, Feng S, et al. Unidirectionally progressive left pneumonectomy & mediastinal lymph node dissection. J Thorac Dis 2013;5:886-91. [PubMed]
- Cai K, Wu H, Ren P, et al. Unidirectionally progressive resection of lower right lung cancer under video-assisted thoracoscopy. J Thorac Dis 2013;5 Suppl 3:S310-4. [PubMed]
- Cai K, Zhao H, Wu H, et al. Unidirectionally progressive resection of left upper pulmonary lobe under video-assisted thoracoscopy. J Thorac Dis 2014;6:1843-7. [PubMed]
- Cai K, Yan Y, Feng S, et al. Unidirectionally progressive resection of lower left lung carcinoma under video-associated thoracoscopy. Asvide 2015;2:163. Available online: http://www.asvide.com/articles/741