National trends in pectus excavatum repair: patient age, facility volume, and outcomes
Introduction
Pectus excavatum (PE) is recognized as the most common anterior chest wall deformity and impacts between 1/300 and 1/400 live births each year (1). For patients diagnosed with sternal depression causing cardiopulmonary compromise, exercise intolerance, or severe cosmetic defect, surgical repair via modified Nuss procedure is frequently offered as treatment. While most patients undergo such repairs as children, a proportion of patients receive treatment as adults. Trends in the demographics of adults undergoing surgical repair of PE and analysis of outcomes as they relate to age at the time of surgery have not previously been analyzed using a representative, national database.
While the modified Nuss procedure has been broadly studied and is accepted as the standard of care for pediatric patients undergoing PE repair, there remains limited high-level evidence on adult repair. Existing literature is exclusively retrospective in nature and predominantly relies on single-institution experiences (2-6). At the patient level, the pediatric literature demonstrates that predominantly male patients undergo modified Nuss procedure. In the adult population, gender balance remains understudied. Existing literature also lacks analysis regarding race, household-income, and insurance status of adults treated for PE. Within the pediatric population, there is evidence of strong Caucasian predominance (>90%) (7).
Regarding postoperative complications, the preponderance of institutional level data suggests worse outcomes for older patients treated via modified Nuss procedure (2-6,8). It remains unclear if these institutional trends are corroborated by national level data. The single prior study utilizing a national database found no significant differences in complications rates between pediatric and adult patients undergoing modified Nuss procedure (9).
The purpose of this study is to utilize a representative national sample to describe the current landscape of adult repair of PE via modified Nuss procedure, with attention to the demographics of patients undergoing adult repair and outcomes as related to patient age and facility procedure volume. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1671/rc).
Methods
Patient data was collected from the National Inpatient Sample (NIS) database between January 2016–Decemeber 2018. The NIS is a large, all-payer inpatient database that is publicly available and allows for the estimation of national trends in the United States (US). Each year of data contains more than 7 million unweighted hospitalizations. Data is collected and maintained by the Healthcare Cost and Utilization Project (HCUP) which is managed by the Agency for Healthcare Research Quality (AHRQ), a division of the US Federal Department of Health and Human Services (HHS). Beginning in 2016, the NIS contains a full-year of data utilizing the ICD-10-CM/PCS codes, thus allowing the separation of modified Nuss procedure from non-specified repairs for PE utilized by ICD-9-CM/PCS. While the term “modified Nuss” has been used broadly in the literature to describe multiple innovations, we employ the term to describe the minimally invasive approach originally developed by Donald Nuss in 1987 utilizing two lateral thoracic incisions via which a sub-sternal steal bar is placed and later modified to allow for the use of thoracoscope to avoid mediastinal injury (10-12). Missing data were reviewed on a case-by-case basis regarding inclusion or exclusion of the given patient. Patient consent was deferred due to the retrospective nature of the analysis and the lack of identifiable information. The Institutional Review Board at Thomas Jefferson University deemed this project exempt (PRC#: 2020-117A, 9/7/21). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) (13).
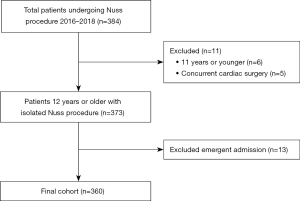
A retrospective cohort analysis was completed for patients 12 years of age or older who underwent a modified Nuss procedure (ICD-10-PCS: 0WU84JZ, supplement chest wall with synthetic substitute, percutaneous endoscopic approach) from 2016–2018. Patients with concurrent cardiac surgery were excluded to better capture complications and charges associated with isolated Nuss repairs, as these additional procedures could potentially bias results (Figure 1).
Data were collected on patient demographics, including: age, sex, race, admission status, and median income quartile by patient zip code (US geographic postal code designations). Data on insurance status was also gathered [Medicare is a federally-funded, public insurance program available to all persons ages 65 or older; Medicaid is a state-based federally subsidized public insurance program with varying qualifications linked to individual or household income-level in each state; private insurance is designated as employer-based insurance programs or those purchased on health insurance marketplaces as a created by the Affordable Care Act (ACA)]. Data was further collected on PE diagnosis (ICD-10: Q676), treatment variables (quantity of diagnoses and procedures, length of stay, and total charges), and surgical complications. Specific detail regarding the severity of chest wall deformity and symptom severity are not included in the NIS data capture and therefore could not be analyzed. Complications were sub-classified according to major vs. minor and type based on the authors’ discretion prior to analysis. Complications which would prolong hospitalization were designated as major (Table 1). Clavien-Dindo classifications are unable to be used when analyzing NIS data given the lack of detail regarding treatment for some complications.
Table 1
| Categorization | Complication |
|---|---|
| Major complication group | |
| Respiratory | Pneumonia |
| Hypoxic respiratory failure | |
| Hypercapnic respiratory failure | |
| Acute pulmonary edema | |
| Acute respiratory distress syndrome | |
| Hematologic | Hemothorax |
| Hemorrhage in respiratory system | |
| Thrombotic | Deep vein thrombosis |
| Clot, axillary vein | |
| Clot, subclavian vein | |
| General post-operative | Vocal cord or larynx paralysis |
| Minor complication group | |
| Respiratory | Air leak |
| Pleural effusion | |
| Exercise-induced bronchospasm | |
| Pulmonary insufficiency | |
| Hematologic | Acute post hemorrhagic anemia |
| General post-operative | Pain, post-operative |
| Fluid overload | |
| Nausea and vomiting | |
| Urinary retention | |
| Subcutaneous emphysema |
Sub-analyses were completed by year, age group, and hospital volume. Patients were grouped by age using categorizations previously reported by Jaroszewski et al. (adolescent: 12–17 years; young adult: 18–29 years; adult: 30+ years) (6). Hospitals which performed greater than the mean number of operations per facility over the 3 years of analysis were categorized as high volume. In contrast, hospitals performing lower than the mean number of operations per facility were deemed low volume centers. After original quartile analysis of the quantity of Nuss operations performed per facility, those performing greater than the mean were deemed high volume. The primary outcome of this study was the likelihood of having a major complication after Nuss repair, frequency and prevalence of minor complications was also explored.
Statistical analysis
Pearson’s χ2 and Student’s t-tests were utilized to compare patient, clinical and hospital characteristics for the cohort of patients undergoing a Nuss repair where appropriate. Fisher’s exact tests were used when expected frequencies were less than 5% for the analysis regarding complication rates. Kolmogorov-Smirnov test was employed to asses for normality. Complications are reported as rate of occurrence. All analyses were completed using STATA/SE 15.1 statistical software (StataCorp LLC, College Station, TX, USA) with a two-sided significance level of P<0.05.
Results
There were 360 patients that met inclusion criteria (Table 2). Age designations were as follows: adolescent: 229 patients (63.6%) vs. young adults: 73 patients (20.3%) vs. adults: 58 patients (16.1%). Among those treated after the age of 30 (adults), the median age was 48 [interquartile range (IQR), 39–62 years]. With regards to the sex, male patients comprised 79.2% [285] of the full cohort. Across three age categorizations, gender balance was as follows: adolescent: 86.9% [199] male vs. young adult: 74% [54] male vs. adult: 55.2% [32] male, P<0.01. Groups also differed in insurance status: adolescent: 73.6% [265] private insurance vs. young adult: 80.8% [59] private insurance vs. adult: 65.5% [38] private insurance, P<0.01. Race differed between age categorizations: adolescent: 80.2% [267] Caucasian vs. young adult: 83.3% [55] Caucasian vs. adult: 85.5% [47] Caucasian, P<0.01. Median total charges differed between age designations: adolescent: $57,312 (IQR, $46,447–69,573) vs. young adult $57,001 (IQR, $45,270–74,213) vs. adult $67,014 (IQR, $51,413–101,514), P=0.01.
Table 2
| Characteristics | Full cohort | 12–17 years | 18–29 years | 30+ years | P value |
|---|---|---|---|---|---|
| N (patients) | 360 | 229 | 73 | 58 | |
| Age (years), median [IQR] | 16 [14, 20] | 15 [14, 16] | 20 [18, 24] | 48 [39, 62] | <0.01 |
| Gender, n (%) | <0.01 | ||||
| Male | 285 (79.2) | 199 (86.9) | 54 (74.0) | 32 (55.2) | |
| Female | 75 (20.8) | 30 (13.1) | 19 (26.0) | 26 (44.8) | |
| Race, n (%) | 0.02 | ||||
| Caucasian | 267 (80.2) | 165 (77.8) | 55 (83.3) | 47 (85.5) | |
| Black | 5 (1.5) | 1 (0.5) | 0 (0.0) | 4 (7.3) | |
| Hispanic | 41 (12.3) | 34 (16.0) | 4 (6.1) | 3 (5.5) | |
| API | 6 (1.8) | 3 (1.4) | 3 (4.5) | 0 (0.0) | |
| Native American | 2 (0.6) | 1 (0.5) | 1 (1.5) | 0 (0.0) | |
| Other | 12 (3.6) | 8 (3.8) | 3 (4.5) | 1 (1.8) | |
| Insurance, n (%) | <0.01 | ||||
| Medicare | 17 (4.7) | 3 (1.3) | 0 (0.0) | 14 (24.1) | |
| Medicaid | 50 (13.9) | 39 (17.0) | 9 (12.3) | 2 (3.4) | |
| Private | 265 (73.6) | 168 (73.4) | 59 (80.8) | 38 (65.5) | |
| Self-pay | 5 (1.4) | 2 (0.9) | 2 (2.7) | 1 (1.7) | |
| No charge | 1 (0.3) | 0 (0.0) | 0 (0.0) | 1 (1.7) | |
| Other | 22 (6.1) | 17 (7.4) | 3 (4.1) | 2 (3.4) | |
| House income by zip code, n (%) | 0.49 | ||||
| 0–25% | 52 (14.6) | 35 (15.4) | 8 (11.1) | 9 (15.8) | |
| 26–50% | 76 (21.3) | 48 (21.1) | 20 (27.8) | 8 (14.0) | |
| 51–75% | 106 (29.8) | 64 (28.2) | 24 (33.3) | 18 (31.6) | |
| 76–100% | 122 (34.3) | 80 (35.2) | 20 (27.8) | 22 (38.6) | |
| Length of stay (days), median [IQR] | 4 [3, 4] | 4 [3, 4] | 3 [2, 4] | 3.5 [2, 5] | 0.20 |
| Total charges in US dollars, median [IQR] | 57,850 [46,447, 73,418] | 57,312 [46,447, 69,573] | 57,001 [45,270, 74,213] | 67,014 [51,413, 101,514] | 0.01 |
IQR, interquartile range; API, Asian and Pacific Islander.
Other than thrombotic complications, all categories of complications differed across age groups (Table 3). Respiratory complications were as follows: adolescent: 3.1% [7] vs. young adult: 13.7% [10] vs. adult: 25.9% [15], P<0.01. For hematologic complications, rates were as follows: adolescent: 0.9% [2] vs. young adult: 20.6% [15] vs. adult: 39.7% [23], P<0.01. Rates of general post-operative complications were as follows: adolescent: 29.3% [67] vs. young adult: 34.3% [25] vs. adult: 39.7% [23], P<0.01. Overall minor complications differed between groups: adolescent: 30.1% [69] vs. young adult: 45.2% [40] vs. adult: 55.8% [32], P<0.01, as did major complications, adolescent: 0.4% [1] vs. young adult: 0% [0] vs. adult: 6.9% [4], P<0.01. Rates of any complications also differed, adolescent: 30.6% [70] vs. young adult: 45.2% [33] vs. adult: 62.1% [36], P<0.01.
Table 3
| Complication | 12–17 years (n=229) | 18–29 years (n=73) | 30+ years (n=58) | P value |
|---|---|---|---|---|
| Respiratory, n (%) | 7 (3.1) | 10 (13.7) | 15 (25.9) | <0.01 |
| Hematologic, n (%) | 2 (0.9) | 15 (20.6) | 23 (39.7) | <0.01 |
| Thrombotic, n (%) | 0 (0.0) | 0 (0.0) | 1 (1.7) | 0.16 |
| General post-operative, n (%) | 67 (29.3) | 25 (34.3) | 23 (39.7) | 0.28 |
| Minor complication, n (%) | 69 (30.1) | 40 (45.2) | 32 (55.8) | <0.01 |
| Major complication, n (%) | 1 (0.4) | 0 (0.0) | 4 (6.9) | 0.01 |
| Any complication, n (%) | 70 (30.6) | 33 (45.2) | 36 (62.1) | <0.01 |
There were 141 facilities designated as low-volume facilities and seven facilities designated as high-volume (Table 4). Of the cohort, 68.2% (249 patients) underwent procedures at low-volume facilities and 30.8% (111 patients) were treated at high-volume facilities. Groups differed regarding median patient age, low-volume: 16 years (IQR, 14–18) vs. high-volume: 18 (IQR, 15–27), P<0.01. They also differed in gender balance, low-volume: 80.7% [201] male vs. high-volume: 75.7% [84] male, P<0.01. Insurance status also differed, low-volume: 69.5% [173] private vs. high-volume: 82.9% [92] private. Length of stay differed, low-volume: 4 (IQR, 3–5) days vs. high-volume: 3 (IQR, 2–4) days, P<0.01.
Table 4
| Characteristics | Low-volume (<7 Nuss repairs) | High-volume (≥7 Nuss repairs) | P value |
|---|---|---|---|
| N (patients) | 249 | 111 | |
| N (facilities) | 141 | 7 | |
| Age (years), median [IQR] | 16 [14, 18] | 18 [15, 27] | <0.01 |
| Age group (years), n (%) | <0.01 | ||
| 12–17 | 179 (71.9) | 50 (45.0) | |
| 18–29 | 36 (14.5) | 37 (33.3) | |
| 30+ | 34 (13.7) | 24 (21.6) | |
| Gender, n (%) | 0.28 | ||
| Male | 201 (80.7) | 84 (75.7) | |
| Female | 48 (19.3) | 27 (24.3) | |
| Race, n (%) | 0.21 | ||
| Caucasian | 175 (77.8) | 92 (85.2) | |
| Black | 3 (1.3) | 2 (1.9) | |
| Hispanic | 29 (12.9) | 12 (11.1) | |
| API | 6 (2.7) | 0 (0.0) | |
| Native American | 1 (0.4) | 1 (0.9) | |
| Other | 11 (4.9) | 1 (0.9) | |
| Insurance, n (%) | 0.01 | ||
| Medicare | 16 (6.4) | 1 (0.9) | |
| Medicaid | 43 (17.3) | 7 (6.3) | |
| Private | 173 (69.5) | 92 (82.9) | |
| Self-pay | 2 (0.8) | 3 (2.7) | |
| No charge | 1 (0.4) | 0 (0.0) | |
| Other | 14 (5.6) | 8 (7.2) | |
| House income by zip code, n (%) | 0.10 | ||
| 0–25% | 39 (15.8) | 13 (11.9) | |
| 26–50% | 58 (23.5) | 18 (16.5) | |
| 51–75% | 75 (30.4) | 31 (28.4) | |
| 76–100% | 75 (30.4) | 47 (43.1) | |
| Length of stay (days), median [IQR] | 4 [3, 5] | 3 [2, 4] | <0.01 |
| Total charges in US dollars, median [IQR] | 57,345 [44,801, 71,596] | 60,168 [50,051, 77,292] | 0.10 |
IQR, interquartile range; API, Asian and Pacific Islander.
Rates of any complication differed between these volume designations (Table 5): low-volume: 32.1% [80] vs. high-volume: 53.2% [59], P<0.01. Overall minor complication rates differed, low-volume: 30.9% [77] vs. high-volume: 51.4% [57], P<0.01. Facilities differed in rates of respiratory complications, low-volume: 4.0% [10] vs. high-volume: 19.8% [22], P<0.01 and hematologic complications, low-volume: 3.2% [8] vs. high-volume: 28.8% [32], P<0.01. The most frequent minor complications at high-volume centers were pleural effusion and acute post-hemorrhagic anemia. Events over time for each age group are presented in Table 6.
Table 5
| Complication | Low-volume (n=249) | High-volume (n=111) | P value |
|---|---|---|---|
| Respiratory, n (%) | 10 (4.0) | 22 (19.8) | <0.01 |
| Hematologic, n (%) | 8 (3.2) | 32 (28.8) | <0.01 |
| Thrombotic, n (%) | 1 (0.4) | 0 (0.0) | 1.00 |
| General post-operative, n (%) | 73 (29.3) | 42 (37.8) | 0.11 |
| Minor complication, n (%) | 77 (30.9) | 57 (51.4) | <0.01 |
| Major complication, n (%) | 3 (1.2) | 2 (1.8) | 0.65 |
| Any complication, n (%) | 80 (32.1) | 59 (53.2) | <0.01 |
Table 6
| Age (years) | Year | Major complication, n=5 (1.4%) | Minor complication, n=134 (17.2%) | Respiratory, n=32 (8.9%) |
Hematologic, n=40 (11.1%) |
Thrombotic, n=1 (0.3%) | General post-operative, n=115 (31.9%) |
|---|---|---|---|---|---|---|---|
| 12–17 (n=229) | 2016 | 1 (100.0) | 30 (43.5) | 5 (71.4) | 1 (50.0) | 0 (0.0) | 29 (43.3) |
| 2017 | 0 (0.0) | 25 (36.2) | 1 (14.3) | 0 (0.0) | 0 (0.0) | 24 (35.8) | |
| 2018 | 0 (0.0) | 14 (20.3) | 1 (14.3) | 1 (50.0) | 0 (0.0) | 14 (20.9) | |
| 18–29 (n=73) | 2016 | 0 (0.0) | 12 (36.4) | 5 (50.0) | 6 (40.0) | 0 (0.0) | 8 (32.0) |
| 2017 | 0 (0.0) | 10 (30.3) | 3 (30.0) | 4 (26.7) | 0 (0.0) | 7 (28.0) | |
| 2018 | 0 (0.0) | 11 (33.3) | 2 (20.0) | 5 (33.3) | 0 (0.0) | 10 (40.0) | |
| 30+ (n=58) | 2016 | 2 (50.0) | 8 (25.0) | 6 (40.0) | 5 (21.7) | 1 (100.0) | 5 (21.7) |
| 2017 | 0 (0.0) | 12 (37.5) | 5 (33.3) | 5 (21.7) | 0 (0.0) | 9 (39.1) | |
| 2018 | 2 (50.0) | 12 (37.5) | 4 (26.7) | 13 (56.5) | 0 (0.0) | 9 (39.1) |
Percentage of complication displayed as total percentage over the individual age group per complication grouping.
There were six missing data elements identified: Four patients lacked household income data, two patients were missing data regard total charges. These patients were included in the final analysis, appropriate adjustments were made in income and charge analyses to reflect these missing data.
Discussion
This analysis has utilized a representative, national sample to demonstrate significant trends in utilization and outcomes of modified Nuss repair related to patient age. As shown in prior literature, the majority of patients in this sample undergoing Nuss procedure are under the age of 18. This data also demonstrates a substantive number of young adults and adults undergoing surgical repair each year. The data suggests more patients than expected undergo repairs during the 5th decade of life. To our knowledge, this has not previously been described. We believe this finding raises important questions about pathways to adult repair of PE. From this data, it is unclear if these patients are aware of their conditions and delay treatment or rather remain undiagnosed until time of repair as adults. In cases in which patients have delayed treatment, it is also unclear what factors influence these decisions. It’s possible that, in this adult cohort, some patients deferred treatment due to the lack of minimally invasive repair available at the time of diagnosis. It is further hypothesized that increasing symptom severity in older age could underpin this trend. Although the Haller index, a validated and widely utilized radiologic measurement of sternal depression, is understood to decrease with age as the shape of the chest wall shifts to a more circular transverse shape (14), it is possible that severity of symptoms simultaneously increases given age-related deterioration in physiologic reserve. Further research is needed to better understand the motivations and decision-making surrounding adult patients undergoing correction of PE.
We have found that the proportion of women undergoing repair differs by age group. In this dataset, there is near gender parity amongst those treated with modified Nuss after the age of 29. It remains unclear what factors drive this trend. Of note, a recent large radiologic cohort study found a slight female predominance of PE utilizing two standardized metrics for chest wall measurement (14). Further research is needed to better understand gender-balance and timing of repair for PE.
Regarding complications, we have identified differences in rates of complications amongst age groups. Our data shows variations based on age in all categories of complications that were analyzed as well as in both major and minor designations. Our results align with previous retrospective literature on the topic from single institution experiences (3-5,8). This prior evidence demonstrates that operative times are significantly longer in patients over 30 (6), that there is a trend toward more frequent sternal bar rotation or displacement (which is attributed to the stiffer chest walls found in older patients) (4,6), and evidence that older age is associated with higher rates of wound infection (4,15). Rates of postoperative urinary tract infection, ileus, readmission and pneumonia have been also shown to be higher for patients over 30 (6,16). Ultimately, there is some evidence that procedures performed on patients after the age of 30 are less successful than those performed on younger patients (6). It has been argued that the decreased compliance of adult chest walls may impact the success of Nuss repair and drive increased rates of some complications (17,18).
Our data and the above literature conflicts with the single previously published large database study evaluating outcomes for adult patients undergoing repair. This study showed no difference in complication rates when comparing pediatric and adult patients treated with modified Nuss procedure (9). It is unclear what underlying differences in data or analysis may have led to these conflicting results. Because of this disparity, further analysis utilizing NSQIP data, NIS data, and other large datasets is needed to corroborate findings.
Regarding facility volume, this analysis shows differences in lengths of stay between low and high-volume centers. This data also suggests that overall complication rates may be comparable or higher at high-volume centers. This trend appears to be driven by minor complications. It conflicts with previous literature on the relationship between volume and outcomes in the context of adult thoracic surgery, where regionalization and specialization of procedures have been linked to overall improved outcomes (19,20). Of note high-volume facilities in this dataset were found to have operated on older patients, a group which was identified as having higher complication rates. Further research is needed to evaluate the extent to which the effect of patient age may bias results related to facility volume and outcomes. Overall, we argue that this data shows that the modified Nuss procedure is being performed safely at both high- and low-volume facilities. This aligns with previous literature surrounding the learning curve for the Nuss procedure showing that after 10 proctored procedures Nuss can safely be performed by surgeons previously untrained in the technique (18).
Finally, with regard to charges, this research shows that modified Nuss repairs in patients 30 and above were associated with higher charges than for younger patients. To our knowledge, no data has been published regarding charges and age at the time of PE repair, and factors underpinning this trend thus remain understudied. Of note, we observed no difference in length of stay across age designations, suggesting alternative drivers of higher charges for older patients. Potential contributing factors may include the higher complication profile of older patients, and the previously described trend toward utilizing more sternal bars in adult patients (21,22). Although the data collected by the NIS does not allow for cost analysis, this analyses shows that further evaluation regarding cost-effectiveness as it relates to patient age and timing of repair is warranted.
There are several important limitations to this study. First, the NIS data analyzed includes approximately 20% of all inpatient hospital encounters in the US each year. It is thus possible major centers performing high volumes of Nuss repair have been inadvertently excluded from this analysis. This could bias our results against the benefit achieved at very high-volume institutions, and this possibility would undermine our analysis with regards to trends in regionalization. Second, because this dataset represents an aggregation of claims retrospectively abstracted mainly for billing, the information related to clinical outcomes may be less reliable than what may be found in other datasets. This would have a non-directional impact on our outcomes, but could lead to an overall false estimation of the safety profile of the procedure. Third, the NIS lacks a variable to describe Haller Index or other measures of PE severity thus limiting our comparison. Fourth, we are limited in the granularity of our analysis of complications due to lack of information about how complications were treated, thus inhibiting the use of the Clavien-Dindo classifications. Finally, because of this study’s retrospective nature, additional sources of bias are introduced, including selection bias. Nonetheless, as a representative sample, there is high generalizability for this NIS study, though our outcomes should be corroborated by further analysis and, ultimately, prospective data.
This analysis shows that the Nuss procedure for correction of PE continues to be widely employed. We illustrate that both major complications and charges increase with patient age. The analysis further demonstrates a trend towards gender parity in adult pectus repair not previously described in the literature, and illustrates an older median age (48 years) for adult patients than previously described. This data raises important questions about the motivations of patients seeking repair later in life, and about the relationship between gender and timing of PE repair. The analysis also questions the utility of regionalization given overall favorable outcomes for procedures performed at low-volume centers. Further research is needed on these topics.
Acknowledgments
Funding: We would like to thank the Saligman Family Foundation for their support of this research.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1671/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1671/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1671/coif). OTO reports receiving honoraria from Intuitive for a webinar within the last year and a grant for BMSF to support his clinical trials research. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Patient consent was deferred due the retrospective nature of the analysis and the lack of identifiable information. The Institutional Review Board at Thomas Jefferson University deemed this project exempt (PRC#: 2020-117A, 9/7/21). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chung CS, Myrianthopoulos NC. Factors affecting risks of congenital malformations. I. Analysis of epidemiologic factors in congenital malformations. Report from the Collaborative Perinatal Project. Birth Defects Orig Artic Ser 1975;11:1-22. [PubMed]
- Mansour KA, Thourani VH, Odessey EA, et al. Thirty-year experience with repair of pectus deformities in adults. Ann Thorac Surg 2003;76:391-5; discussion 395. [Crossref] [PubMed]
- Coln D, Gunning T, Ramsay M, et al. Early experience with the Nuss minimally invasive correction of pectus excavatum in adults. World J Surg 2002;26:1217-21. [Crossref] [PubMed]
- Kim DH, Hwang JJ, Lee MK, et al. Analysis of the Nuss procedure for pectus excavatum in different age groups. Ann Thorac Surg 2005;80:1073-7. [Crossref] [PubMed]
- Cheng YL, Lee SC, Huang TW, et al. Efficacy and safety of modified bilateral thoracoscopy-assisted Nuss procedure in adult patients with pectus excavatum. Eur J Cardiothorac Surg 2008;34:1057-61. [Crossref] [PubMed]
- Jaroszewski DE, Ewais MM, Chao CJ, et al. Success of Minimally Invasive Pectus Excavatum Procedures (Modified Nuss) in Adult Patients (≥30 Years). Ann Thorac Surg 2016;102:993-1003. [Crossref] [PubMed]
- Tetteh O, Rhee DS, Boss E, et al. Minimally invasive repair of pectus excavatum: Analysis of the NSQIP database and the use of thoracoscopy. J Pediatr Surg 2018;53:1230-3. [Crossref] [PubMed]
- Schalamon J, Pokall S, Windhaber J, et al. Minimally invasive correction of pectus excavatum in adult patients. J Thorac Cardiovasc Surg 2006;132:524-9. [Crossref] [PubMed]
- Kauffman JD, Benzie AL, Snyder CW, et al. Short-term Outcomes After Pectus Excavatum Repair in Adults and Children. J Surg Res 2019;244:231-40. [Crossref] [PubMed]
- Nuss D, Kelly RE Jr, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545-52. [Crossref] [PubMed]
- Nuss D. Recent experiences with minimally invasive pectus excavatum repair "Nuss procedure". Jpn J Thorac Cardiovasc Surg 2005;53:338-44. [Crossref] [PubMed]
- Nuss D, Obermeyer RJ, Kelly RE. Nuss bar procedure: past, present and future. Ann Cardiothorac Surg 2016;5:422-33. [Crossref] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310:2191-4. [Crossref] [PubMed]
- Biavati M, Kozlitina J, Alder AC, et al. Prevalence of pectus excavatum in an adult population-based cohort estimated from radiographic indices of chest wall shape. PLoS One 2020;15:e0232575. [Crossref] [PubMed]
- Aronson DC, Bosgraaf RP, van der Horst C, et al. Nuss procedure: pediatric surgical solution for adults with pectus excavatum. World J Surg 2007;31:26-9; discussion 30. [Crossref] [PubMed]
- Johnson WR, Fedor D, Singhal S. Systematic review of surgical treatment techniques for adult and pediatric patients with pectus excavatum. J Cardiothorac Surg 2014;9:25. [Crossref] [PubMed]
- Weber PG, Huemmer HP, Reingruber B. Forces to be overcome in correction of pectus excavatum. J Thorac Cardiovasc Surg 2006;132:1369-73. [Crossref] [PubMed]
- de Loos ER, Daemen JHT, Pennings AJ, et al. Minimally invasive repair of pectus excavatum by the Nuss procedure: The learning curve. J Thorac Cardiovasc Surg 2022;163:828-837.e4. [Crossref] [PubMed]
- Hannan EL, Radzyner M, Rubin D, et al. The influence of hospital and surgeon volume on in-hospital mortality for colectomy, gastrectomy, and lung lobectomy in patients with cancer. Surgery 2002;131:6-15. [Crossref] [PubMed]
- Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med 2002;346:1128-37. [Crossref] [PubMed]
- Pilegaard HK, Licht PB. Routine use of minimally invasive surgery for pectus excavatum in adults. Ann Thorac Surg 2008;86:952-6. [Crossref] [PubMed]
- Park HJ, Lee SY, Lee CS, et al. The Nuss procedure for pectus excavatum: evolution of techniques and early results on 322 patients. Ann Thorac Surg 2004;77:289-95. [Crossref] [PubMed]