Primary tracheobronchial non-Hodgkin lymphoma causing life-threatening airway obstruction: a case report
Introduction
Non-Hodgkin lymphoma (NHL) involving the central airway is uncommon, even though the disease frequently involves extranodal organs. In fact, primary tracheobronchial NHL occurs in less than 1% of all NHL patients (1). Involvement of central airways in NHL can cause respiratory failure (2), make treatment difficult, and lead to poorer prognosis. Here we report a case of primary tracheobronchial NHL in which the patient was suffering rare, life-threatening obstruction of the central airway that prevented us from administering chemotherapy. To alleviate the airway obstruction, we performed interventional bronchoscopy involving cryotherapy, electrocautery and argon plasma coagulation. This allowed us to administer chemotherapy and obtain a good clinical response.
Case presentation
A 56-year-old man was referred to our hospital with complaints of productive cough and progressive dyspnea lasting 20 days. He was afebrile, but he had lost 10 kg in 2 months. Vital signs were normal: temperature, 36.5 °C; respiration rate, 20 bpm; pulse, 78 bpm; blood pressure, 125/70 mmHg. Breathing sounds in the left lung were reduced. Computed tomography (CT) of the chest showed that a tumor was blocking the left main stem bronchus, and enlarged lymph nodes were compressing the trachea and main bronchi (Figure 1A,B). We also observed obvious mediastinal and bilateral hilar lymphadenopathy. Blood gas analysis showed type I respiratory failure (pH 7.44; PaO2, 57 mmHg; PaCO2, 38 mmHg). Blood cell count was normal.
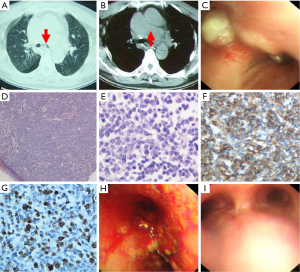
Bronchoscopy revealed widening of the carina, thickening and distortion of the mucosa folds at the end of the trachea and bilateral blockage of the main bronchial stems due to a polypoid mass (Figure 1C). Bronchoscopic forceps biopsy was performed, and eight tissue samples were recovered. Analysis of the samples suggested lymphoma, but this could not be definitively determined on the basis of the small number of cells in the samples.
Patient stress resulting from progressive dyspnea, coupled with our inability to effectively administer chemotherapy, led us to perform interventional bronchoscopy 2 days after patient admission. First the polypoid mass on the less severe side (right main bronchial stem) was removed by cryotherapy (ERBOKRYO CA, ERBE Elektromedizin, Germany) in combination with argon plasma coagulation (VIO 200S, ERBE) and mechanical removal. This completely resolved the obstruction in the right main bronchial stem, and the cryobiopsy provided sufficient samples for definitive pathological diagnosis. Pathological examination showed diffuse infiltration of atypical lymphoid cells with obvious dyskaryosis beneath intact bronchial mucosa (Figure 1D,E). Positive immunochemical staining was observed against CD20 (Figure 1F) and Pax-5, while no staining was observed against CD3, EMA, or Bcl-6. The Ki67 proliferation fraction was high (50%) (Figure 1G). The final diagnosis was diffuse large B cell lymphoma (active B-cell like subtype).
Two days later, we performed a second interventional bronchoscopy to remove the protrusive lesion in the left main bronchial stem (Figure 1H); the same procedure of cryotherapy, electrocautery, and argon plasma coagulation was used as in the first bronchoscopy. The patient’s condition improved substantially after the second bronchoscopy. Most importantly, the patient no longer suffered hypoxia (PaO2, 81 mmHg), allowing us to proceed with chemotherapy. No complications related to either interventional bronchoscopy were observed.
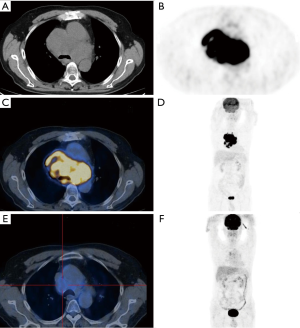
Before initiating systemic chemotherapy, we analyzed the patient using fluorine-18 fluoro-2-deoxyglucose (FDG)-positron emission tomography CT (PET-CT), abdominal contrast CT, and bone marrow aspiration to assess NHL stage.
The patient received a total of six cycles of R-CHOP chemotherapy (rituximab, 375 mg/m2 intravenously, on Day 1; cyclophosphamide, 750 mg/m2 intravenously, on Day 1; doxorubicin, 50 mg/m2 intravenously, on Day 1; vincristine, 1.4 mg/m2 intravenously on Day 1; and prednisone, 100 mg orally daily for 5 days). After only two cycles of chemotherapy, the patient showed complete clinical recovery with no obvious side effects. Bronchoscopy examination after two cycles showed complete recovery of the central airways (Figure 1I). Compared with PET-CT on baseline (Figure 2A-D), PET-CT after two cycles chemotherapy showed obviously reduced involvement in the chest (Figure 2E,F). The patient’s condition remained stable for at least the following 24 months.
Discussion
Primary tracheobronchial NHL is rare, comprising only about 0.23% of all cases of tracheal tumors and affecting only 3.6% of NHL patients with extranodal disease (3); indolent follicular and diffuse B-cell lymphomas are the most common types (4).
The most common symptoms resulting from primary tracheobronchial lymphoma are dyspnea, cough and wheezing. These symptoms are non-specific, as are the radiological manifestations. But dyspnea is a clue of the severity of central airway obstruction. In adult patients, dyspnea on exertion generally indicates that diameter of trachea is less than 8 mm. Dyspnea at rest indicates that the diameter of tracheal is less than 5 mm. The more percentage reduction in the luminal cross-sectional area, the more severity of dyspnea. Respiratory failure is highly prevalent among such patients. If respiratory failure existed, immediate procedure should be taken to eliminate the airway obstruction and maintain the adequate ventilation. Interventional pulmonology are advisable because interventional pulmonology can not only confirm the diagnosis, but an effective treatment.
First, performing bronchoscopy to obtain a pathological diagnosis is critical, but we found that forceps biopsy via bronchoscopy did not provide sufficient material for definitive diagnosis of lymphoma. Subsequent cryobiopsy provided adequate samples that led to definitive diagnosis. Consistent with our experience, previous study compared endobronchial cryobiopsy and forceps biopsy for diagnosing lung cancer, and found that cryobiopsy provides better specimens and provides greater diagnostic accuracy (5).
Second, our clinical experience mirrors previous studies that have used interventional or rigid bronchoscopy to perform endobronchial resection or stent placement in patients with tracheobronchial lymphoma and respiratory failure to eliminate airway obstruction (6). This is a prerequisite to performing the standard treatments of NHL, i.e., tumor-specific chemo- or radiotherapy.
Thirty cases of airway stenosis or occlusion have been reported in patients with NHL (6-8), and treatments have ranged from silicone stents and external radiation therapy, to radiofrequency ablation (9) and endoscopic neodyminum-yttrium-aluminum-garnet (Nd-YAG) laser (10). We opted to use cryotherapy, which has been shown to destroy endobronchial tumors through the cytotoxic effects of freezing. Combining cryotherapy with electrocautery and argon plasm coagulation, we found that the procedure was easy to apply and involved no significant complications. The patient showed a good clinical response to R-CHOP chemotherapy and dramatic recovery of endobronchial lesion. Multi-disciplinary team is crucial for the treatment of primary tracheobronchial NHL, especially in the patients with severe central airway obstruction.
Conclusions
Tracheobronchial involvement of NHL is rare and can be fatal, so it should be considered in the differential diagnosis of airway obstruction that occurs together with mediastinal lymphadenopathy. Cryotherapy is an effective method to obtain samples for definitive diagnosis. When combined with other interventions, it can alleviate airway obstruction of tracheobronchial NHL and enable the patient to receive tumor-specific chemotherapy or other treatments.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Solomonov A, Zuckerman T, Goralnik L, et al. Non-Hodgkin's lymphoma presenting as an endobronchial tumor: report of eight cases and literature review. Am J Hematol 2008;83:416-9. [PubMed]
- Tan DS, Eng PC, Lim ST, et al. Primary tracheal lymphoma causing respiratory failure. J Thorac Oncol 2008;3:929-30. [PubMed]
- Kiani B, Magro CM, Ross P. Endobronchial presentation of Hodgkin lymphoma: a review of the literature. Ann Thorac Surg 2003;76:967-72. [PubMed]
- Cordier JF, Chailleux E, Lauque D, et al. Primary pulmonary lymphomas. A clinical study of 70 cases in nonimmunocompromised patients. Chest 1993;103:201-8. [PubMed]
- Hetzel J, Eberhardt R, Herth FJ, et al. Cryobiopsy increases the diagnostic yield of endobronchial biopsy: a multicentre trial. Eur Respir J 2012;39:685-90. [PubMed]
- Takami A, Okumura H, Maeda Y, et al. Primary tracheal lymphoma: case report and literature review. Int J Hematol 2005;82:338-42. [PubMed]
- Önür ST, Dalar L, Sökücü SN. Primary tracheal B-cell lymphoma causing recurrent central airway obstruction. Arch Bronconeumol 2014;50:411-2. [PubMed]
- Luick ML, Hansen EK, Greenberg MS, et al. Primary tracheal non-Hodgkin's lymphoma. J Clin Oncol 2011;29:e193-5. [PubMed]
- Sudheendra D, Barth MM, Hegde U, et al. Radiofrequency ablation of lymphoma. Blood 2006;107:1624-6. [PubMed]
- Tsurutani J, Kinoshita A, Kaida H, et al. Bronchoscopic therapy for mucosa-associated lymphoid tissue lymphoma of the trachea. Intern Med 1999;38:276-8. [PubMed]


