Video-assisted thoracoscopic surgery tracheal resection and carinal reconstruction for tracheal adenoid cystic carcinoma
Introduction
Tracheal resection and carinal reconstruction for tracheogenic carcinoma remains a challenging procedure with high mortality and morbidity rates (1). In the past we have successfully performed thoracoscopic half carinal resection and thoracoscopic bronchial sleeve resection in patients with central lung cancer (2). Based on our previous experience we decided to perform video-assisted thoracoscopic surgery (VATS) tracheal resection and carinal reconstruction for tracheal adenoid cystic carcinoma (ACC) and describe here our initial experience.
Case presentation
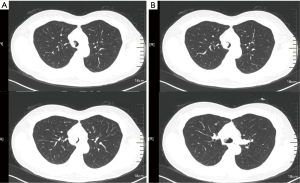
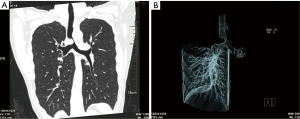
A 47-year-old female presenting with cough, wheezing and shortness of breath was referred to our hospital for treatment of a distal tracheal tumor detected by enhanced chest computerized tomography (CT). The chest CT (Figure 1) showed a mass in the distal trachea involved with the carina and right main bronchus. Reconstructed chest CT (Figure 2) revealed that the exophytic extension of the tumor measured 2.1 cm × 1.2 cm. Neither mediastinal lymphadenopathy nor obvious invasion to surrounding structures was noted. Using a flexible bronchoscopy, we found a submucosal tracheal tumor partially blocking the opening of the right main bronchus. A bronchoscopic biopsy was performed, and the tumor was found to be ACC. An examination of pulmonary function revealed severely restricted respiratory function; the forced expiratory volume in the first second (FEV1) was 0.461 L, 17% of predicted value.
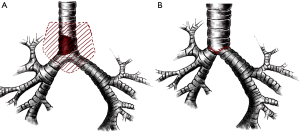
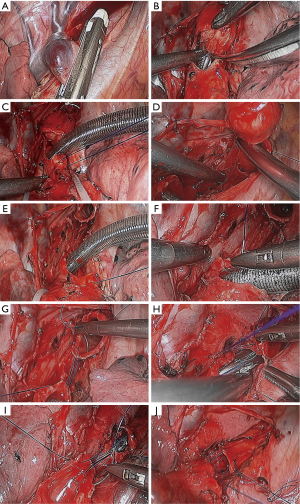
Surgical technique (Figure 3)

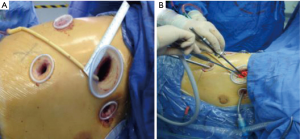
Combined intravenous anesthesia was achieved using a single-lumen 6.5-mm endobronchial tube (Well Lead Inc., Guangzhou, Guangdong, China) intubation. A bronchoscope was used to ensure proper positioning of the endobronchial tube for left lung ventilation. Overall, four incisions were made (Figure 4A): a 10-mm camera incision, placed in the seventh intercostal space (ICS) along the right anterior axillary line; a 10-mm auxiliary incision, located in the same ICS along the posterior axillary line; a 4-cm main incision, located in the fourth ICS on the right anterolateral chest wall; and finally a 10-mm incision in the second ICS along the right anterior axillary line, this 10 mm incision was made for placement of an endobronchial tube for cross-field ventilation specifically necessary for this operation (Figure 4B). Soft incision protectors (Hakko Co. Ltd, Japan) were used for all four incisions.
Before dissection, the mediastinal pleura were inspected to assess the mobility of the tumor and its invasion into surrounding structures. Once radical surgery (Figure 5) was guaranteed, the azygos vein was dissected and transected using 35-mm Endo cutter (Ethicon Inc., Somerville, NJ, USA) (Figure 6A); after which, the distal trachea and bilateral bronchi were divided. Major attention was required to protect the bronchial arteries and vagus nerve. First, the distal trachea was cut off (Figure 6B). Then, the oral endobronchial tube was withdrawn and replaced by use of a cross-field 6.0 mm reinforced endobronchial tube (Well Lead Inc., Guangzhou, Guangdong, China) (Figure 6C) placed through the fourth (10 mm) incision (Figure 4B). The proximal of bilateral main bronchus were transected 1 cm from the opening. Then the tumor was resected 0.5 cm away from the proximal trachea (Figure 6D). The right main bronchus was resected twice more, and the last margin was 0.5 cm away from the initial R1 resection margin confirmed by intraoperative frozen section diagnosis. While waiting for the third frozen section diagnoses of the right bronchus, a figure-of-eight suture was performed between the remnants of the bilateral main bronchus to create a proper angle of newly reconstructed carina (Figure 6E). After which, end-to-end anastomosis between remnant trachea and the left bronchus was performed on the left joint of membranous and cartilaginous trachea using 3–0 Prolene (Ethicon Inc., Somerville, NJ, USA) running suture; suture started on the cartilaginous section (Figure 6F,G). Once posterior wall anastomosis was completed, the cross-filed 6.0 mm reinforced endobronchial tube was retracted through the thoracic incision, and the oral 6.5 mm endobronchial tube was reinserted to the left main-stem bronchus (Figure 6H). After use of endobronchial intubation re-ensued, one quarter of the primary end-to-end anastomosis remained unfinished (Figure 6I): finally, the right bronchus was re-implanted into the aperture using 3–0 Prolene (Ethicon Inc., Somerville, NJ, USA) running sutures (Figure 6J). After confirming no air leakage from suture lines, thoracic surgery was completed by placement of two intercostal drainage tubes and closure of the thoracic incisions.
Surgical outcome
The total operative time was 280 minutes. Sixty-two minutes were spent waiting for confirmation on the three frozen sections, and exact time for airway reconstruction was 58 minutes. The estimated intraoperative blood loss was 200 mL. Postoperative extubation was achieved in the recovery room. The drainage tubes were removed on postoperative day two (POD2) and POD4. Postoperative recovery was uneventful. As a precautionary measure, the patient’s cervical motion was restricted by use of a cervical collar, until she was discharged on POD15. Pathology revealed ACC of the tumor, and a result of negative for all six subcarinal lymph nodes and the surgical margin.
The general condition of the patient was restored and normal life resumed 1 month after the operation without complaints of cough or pain. The follow-up examination of pulmonary function revealed normal respiratory function; the FEV1 was 2.31 L, 87% of predicted value.
Discussion
ACC of the airway is a relatively rare, low-grade malignant tumor. Our goal was to restore airway continuity, and provide pathological complete resection for this patient’s condition, which demanded surgical intervention (tracheal resection and carinal reconstruction). However, this is a challenging procedure in most medical centers even when performed under open thoracotomy because of the high rates of postoperative morbidity and mortality (1).
With accumulation of VATS experiences (2,4-8), we planned VATS tracheal resection and carinal reconstruction to bring our patient the greatest benefit with the least trauma, and quickest recovery. Before surgery, bronchoscopic evaluation confirmed tumor invasion by multiple biopsies of the trachea, carina and the opening of bilateral bronchus. The use of autologous flaps has been reported for closure of airway defects. In this case, however, the right lung was intact, there was no extra tension on the suture site, and no air was leaking from the primary suture lines, therefore, flaps were not used to enforce the anastomosis and the patient recovered well.
Inspired by progressive innovation in airway administration of anesthesia for VATS (5,9), we used the cross-field ventilation: endobronchial intubation through a 10 mm thoracic incision to maintain left lung ventilation. Though the additional cross-field ventilation is a complex and time consuming procedure, it is a necessity in the completion of this difficult carinal reconstruction. However necessary it may be, this cross-field endobronchial tube may obstruct the view of the first anastomosis site, and may require periodical retraction during anastomosis to improve exposure.
It was not until 1 month after the surgery that we started reviewing the relevant reports. We found that there was a similar cross-field endobronchial ventilation technique previously used to perform tracheoplasty (10). However, we performed a VATS carinal reconstruction that provides the most serious challenge to thoracic surgeons, as it requires two separate sets of anastomosis: an initial incomplete anastomosis between the trachea and left main bronchus and a second anastomosis, of probable unfit openings, between the remaining aperture of the first anastomosis and the right main bronchus.
And further reviewing the relevant publications, we found a similar procedure was successfully performed under high-frequency jet ventilation (HFJV) (11). However, in our practice, we observed that HFJV can cause moderate right lung ventilation, which would affect the operative view. There were also concerns that the use of HFJV could be a risk factor for development of acute respiratory distress syndrome (ARDS) (12). And the cross-field ventilation that we used, maintained more stable and safer ventilation than HFJV. Therefore, the extra surgical trauma created by a fourth incision was compensated by more stable vital signs, better operative vision, shorter operative time, and, as a result, less trauma.
In conclusion, VATS tracheal resection and carinal reconstruction brings the patient both functional and oncological benefits. To the best of our knowledge, this thoracoscopic procedure is the first reported VATS carinal reconstruction using cross-field ventilation in the world.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mitchell JD, Mathisen DJ, Wright CD, et al. Clinical experience with carinal resection. J Thorac Cardiovasc Surg 1999;117:39-52; discussion 52-3. [PubMed]
- Xu X, Chen H, Yin W, et al. Thoracoscopic half carina resection and bronchial sleeve resection for central lung cancer. Surg Innov 2014;21:481-6. [PubMed]
- He J, Wang W, Li J, et al. VATS tracheal resection and carinal reconstruction for tracheal ACC. Asvide 2016;3:053. Available online: http://www.asvide.com/articles/804
- Huang J, Li J, Qiu Y, et al. Thoracoscopic double sleeve lobectomy in 13 patients: a series report from multi-centers. J Thorac Dis 2015;7:834-42. [PubMed]
- Liu J, Cui F, Li S, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. [PubMed]
- Shao WL, Liu LX, He JX, et al. Bronchial sleeve resection and reconstruction of pulmonary artery by video-assisted thoracic small incision surgery for central lung cancer: a report of 139 cases. Zhonghua Wai Ke Za Zhi 2007;45:1530-2. [PubMed]
- Li S, Chai H, Huang J, et al. Hybrid video-assisted thoracic surgery with segmental-main bronchial sleeve resection for non-small cell lung cancer. Surg Innov 2014;21:180-6. [PubMed]
- Shao W, Liu J, Liang W, et al. Safety and feasibility of video-assisted thoracoscopic surgery for stage IIIA lung cancer. Chin J Cancer Res 2014;26:418-22. [PubMed]
- Guo Z, Shao W, Yin W, et al. Analysis of feasibility and safety of complete video-assisted thoracoscopic resection of anatomic pulmonary segments under non-intubated anesthesia. J Thorac Dis 2014;6:37-44. [PubMed]
- Zhao G, Dong C, Yang M, et al. Totally thoracoscopic tracheoplasty for a squamous cell carcinoma of the mediastinal trachea. Ann Thorac Surg 2014;98:1109-11. [PubMed]
- Nakanishi R, Yamashita T, Muranaka K, et al. Thoracoscopic carinal resection and reconstruction in a patient with mucoepidermoid carcinoma. J Thorac Cardiovasc Surg 2013;145:1134-5. [PubMed]
- Porhanov VA, Poliakov IS, Selvaschuk AP, et al. Indications and results of sleeve carinal resection. Eur J Cardiothorac Surg 2002;22:685-94. [PubMed]