Management of long-term persistent air leakage developed after bullectomy for giant bullous lung disease associated with neurofibromatosis type 1
Introduction
Neurofibromatosis type 1 (NF-1) is an autosomal-dominant dysplasia with multiple clinical manifestations concluding Café-au-lait spots, Lish nodules, and bullous lung diseases (1). Giant bullous emphysema surgery can be an effective procedure for improving airflow and exercise capacity (2). However, persistent air leakage can occur as a major complication of this surgery and can be difficult to manage (3). Covering the staple line with polyglycolic acid (PGA) felt (Neoveil, Gunze Ltd, Kyoto, Japan) can be a good solution for the prevention of postoperative air leakage (4), but its efficacy in the treatment of prolonged pleural fistula remains unclear. This study describes a novel method for the management of long-term persistent air leakage using PGA felt.
Case presentation
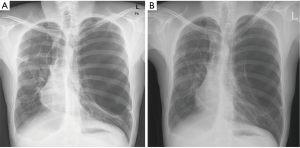
A 32-year-old male patient visited the emergency room for severe dyspnea. He had been diagnosed with NF-1 and sometimes experienced shortness of breath, but had not undergone respiratory work-up. Simple chest radiography and chest tomography revealed left spontaneous pneumothorax and severe bilateral emphysematous lung disease (Figure 1A). Closed thoracostomy with a 28-Fr chest tube was performed, the chest tube could not be removed for 4 days. Most of the left lung was still collapsed due to the presence of huge bullae (Figure 1B). Pneumothorax recurred after 51 days and treatment was repeated. Again, the chest tube could not be removed for 4 days. Chemical pleurodesis was considered for the prevention of recurrence, but was not performed because it could affect future surgeries including lung volume reduction surgery or lung transplantation. A third recurrence of pneumothorax on the same side developed after 6 days and massive air leakage was found. Moreover, the lung was not inflated even after chest tube insertion. Surgery was performed to address the air leakage and remove the huge bullae.
First operation
A double-lumen endotracheal tube was inserted and video-assisted thoracic surgery (VATS) was performed using three ports. One huge and multiple large bullae were present and were compressing the lungs. Air leakage was mainly observed on the apex of the huge bulla, but small leaks were found at multiple sites. Pneumonectomy or left upper lobectomy with multiple wedge resection was needed to remove the largest bulla. Even with the use of invasive procedures, multiple bullae on the left lower lung would still remain. Thus, the surgical plan was changed to reduce the size of the huge bulla and stop the leakage. Multiple endostapling and sandwiching of PGA felt were performed. The size of the huge bulla was reduced by half and the compression effect disappeared; however, multiple air leaks, especially along the staple line, were present. The staple line was covered with PGA felt and fibrin sealant. It took 12 days for the lungs to sustain expansion without thoracic wall suction. Air leakage was still observed during cough, but not during normal breathing on day 24 postoperative. The chest tube was removed on the same day and the lungs did not collapse. On first follow-up (31st postoperative days) in the outpatient clinic, the left lung neither collapsed nor fully filled the pleural space.
Second operation
A second operation was selected as the appropriate course of treatment after third and fourth recurrent pneumothorax, particularly due to the massive air leakage seen at the fourth recurrence. A similar anesthesia technique and VATS procedures were used. There was one large hole (4 mm) causing massive air leakage. There were no other leakage sites. Prolene 4-0 pledget suture was used in an attempt to close the hole. Air leakage was decreased, but still occurred at the suture site and needle puncture holes. Additional sutures appeared useless, so the suture line was covered with PGA felt and fibrous sealant was applied. Air leakage was decreased, but the left lung did not expand without postoperative thoracic wall suction.
Third operation (Figures 2,3)
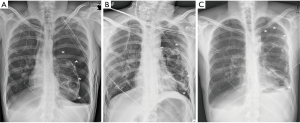
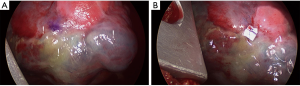
Massive air leakage redeveloped on the 7th postoperative day and the left lung collapsed completely (Figure 2A). Thoracic wall suction was not effective in expanding the left lung and dyspnea was aggravated. On the 14th postoperative day, VATS exploration was done. Air leakage was found at the previous leak site under the PGA felt (Figure 3A). The felt was half-absorbed, but adhered tightly around the leak site (Figure 3A). Prolene 4-0 pledget suture was tried again on the PGA felt. Fortunately, air leakage stopped completely with just a single suture (Figure 3B), and no air leakage was caused by the needle puncture hole. The lung expanded without postoperative thoracic wall suction (Figure 2B). The chest tube was removed on the 5th postoperative day and the patient was discharged the next day. The patient and the left lung in particular were stable on the first follow-up visit (12th postoperative days) at the outpatient clinic (Figure 2C).
Discussion
Long-term persistent air leakage can be stopped completely via sutures on half-absorbed PGA felt. Persistent air leakage is a serious complication and prolongs hospital admission. Moreover, it can be fatal, especially when massive. PGA felt can be used to prevent air leakage (4); various techniques have been reported for this (5-7), but a unique method was applied in this case, when massive air leakage persisted even after initial application of the PGA felt. The surface of the emphysematous lung was thin and fragile, so sutures led to further air leakage at the needle puncture holes, and tension caused the lungs to tear. Covering the suture line with PGA felt was not effective for stopping postoperative air leakage; however, another operation was successful. A recent report (8) suggested that the membrane of the bullae could be reinforced with PGA felt. In this case, a second trial of sutures on the PGA felt stopped the air leak immediately, not only at the main lesion, but also at the needle puncture hole.
However, it is not clear whether this technique is effective with a single application of PGA felt and sutures at the same time. There was a delay of 13 days between the second and third operations in this case. A month passed before pathologic evidence of reinforcement of the bullae with PGA felt was observed in another report (8). Therefore, this method appears most suitable in long-term persistent air leakage even after PGA felt application. However, the duration between PGA application and suture should not be greater than 5 months. Because the felt can completely disappear after 5 months, bullae reinforcement should not be anticipated after this point.
In conclusion, effective management of air leakage is important in the field of general thoracic surgery. Delayed suture on PGA felt can be an easy and effective treatment option for long-term persistent air leakage in giant bullous lung disease associated with neurofibromatosis type 1.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Zamora AC, Collard HR, Wolters PJ, et al. Neurofibromatosis-associated lung disease: a case series and literature review. Eur Respir J 2007;29:210-4. [PubMed]
- Neviere R, Catto M, Bautin N, et al. Longitudinal changes in hyperinflation parameters and exercise capacity after giant bullous emphysema surgery. J Thorac Cardiovasc Surg 2006;132:1203-7. [PubMed]
- Krishnamohan P, Shen KR, Wigle DA, et al. Bullectomy for symptomatic or complicated giant lung bullae. Ann Thorac Surg 2014;97:425-31. [PubMed]
- Lee S, Park SY, Bae MK, et al. Efficacy of polyglycolic acid sheet after thoracoscopic bullectomy for spontaneous pneumothorax. Ann Thorac Surg 2013;95:1919-23. [PubMed]
- Saito T, Kaneda H, Konobu T, et al. The covering with forceps-assisted polymeric biodegradable sheet and endostapling method: a simplified technique for wide coverage and reinforcement of staple-line in video-assisted thoracoscopic bullectomy for spontaneous pneumothorax. Interact Cardiovasc Thorac Surg 2011;12:103-5. [PubMed]
- Shinya N, Oka S, Miyabashira S, et al. Improvement of the tissue-adhesive and sealing effect of fibrin sealant using polyglycolic acid felt. J Invest Surg 2009;22:383-9. [PubMed]
- Maniwa T, Kaneda H, Saito Y. Management of a complicated pulmonary fistula caused by lung cancer using a fibrin glue-soaked polyglycolic acid sheet covered with an intercostal muscle flap. Interact Cardiovasc Thorac Surg 2009;8:697-8. [PubMed]
- Kuwata T, Shinohara S, Takenaka M, et al. The impact of covering the bulla with an absorbable polyglycolic acid (PGA) sheet during pneumothorax surgery. Gen Thorac Cardiovasc Surg 2015. [Epub ahead of print]. [PubMed]


