
Thoracic surgery in the Netherlands
Introduction
Thoracic surgery is, to a varying extent, performed all around the world. Its first documented origin dates from 2500 before Christ when the first esophageal wound was closed, while the first resection of lung parenchyma was performed as early as 1499 after Christ (1). These two events demonstrate the broad range of pathologies and procedures covered by the term thoracic surgery. In addition, international differences in the healthcare landscape and its regulations create further diversification.
Since thoracic surgery is rapidly developing in both technical, technological and enhanced recovery areas encompassing minimally invasive approaches, perioperative care and multi-modality treatment of chest diseases, thoracic surgeons are faced with various opportunities and challenges. Due to international healthcare landscape variations, countries and regions may excel in different areas and experience different thoracic surgery-related issues. The aim of the present article is to provide a descriptive review on thoracic surgery in the Netherlands as part of the Thoracic Surgery Worldwide series, elaborating on the organization of thoracic surgery in the Netherlands, touching upon the Dutch healthcare system and regulations, the training and continuing certification of thoracic surgeons, as well as their areas of expertise, research and future challenges and advances.
General information about the Dutch population and the Dutch healthcare system
The Netherlands has 17.6 million inhabitants [2020], of whom 20% are 65 years or older, and 25% are of non-Dutch origin (2). The life expectancy is 81.5 years based on the 2021 index year, and still increases (3). The Dutch population has a relatively good health status owing to good living and working conditions, whereas more than a quarter of the overall burden of diseases is linked to behavioral risk factors such as smoking and obesity (4). Of the 168,678 deaths in the Netherlands reported in 2020, lung cancer (6%) was one of the leading causes of death alongside severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (12%) and dementia (9%) (5). In the upcoming years, the incidence of lung cancer is not expected to decrease due to prior tobacco use. However, as of 2020 smoking is prohibited in all public buildings and in the upcoming years the sale of tobacco will become more and more restricted (6). The stricter tobacco laws have yet to be evaluated for their impact on pulmonary and cardiovascular diseases.
Healthcare in the Netherlands is primarily governed by the 2006 Health Insurance Act (Dutch: Zorgverzekeringswet, Zvw), a demand-driven system which includes a total of 20 private, non-profit healthcare providers in 2021, and is controlled by the independent Dutch Health Care Authority (Dutch: Nederlandse Zorgautoriteit, NZa), funded by the Ministry of Health, Welfare and Sport (7,8). All inhabitants and commuters are legally obliged to secure at least a basic health insurance. Medical care is divided into three levels based on the complexity of the disease. Primary care is provided by general practitioners during the day at small local practices and after-hours at large-scale health centers (Dutch: huisartsenpost), which are often integrated within hospital emergency departments forming an emergency care access point (9). Secondary care is provided by 69 hospital organizations including eight academic hospitals, divided over 116 regional hospital locations and 129 outpatient clinics (10). Among tertiary care providers are 26 large non-academic teaching hospitals affiliated with the Association of Top Clinical Teaching Hospitals (Dutch: Stichting Topklinische Ziekenhuizen, STZ) and eight academic hospitals (11).
The Netherlands dedicated a total of €80,900 million (€4,665 per capita) to health care in 2019, corresponding to 10% of the gross domestic product (GDP) (12). Compared to other European countries, the Netherlands had the lowest percentage (65%) of health expenditure spent on (para)medical care and the highest percentage (27%) on health-related long-term care (12).
Organization of thoracic surgery in the Netherlands
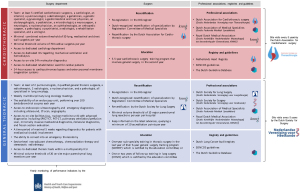
In the Netherlands, thoracic surgery is performed by general thoracic surgeons and cardiothoracic surgeons in 51 different hospitals, of which 15 have a cardiothoracic practice and four centers perform pediatric cardiothoracic surgery (13,14). The majority of thoracic procedures in the Netherlands are performed by approximately 110 general thoracic surgeons, whereas the rest is performed by a subspecialized group of approximately 25 cardiothoracic surgeons of the 135 registered Dutch cardiothoracic surgeons. Of note, both general thoracic surgeons and cardiothoracic surgeons have their own professional association, training program, and standards for (re)certification. An overview of the requirements for (re)certification of (cardio)thoracic surgery centers and surgeons can be found in Figure 1.
Cardiothoracic surgeons
Cardiothoracic surgeons mainly focus on cardiac surgery. As mentioned before, only a selected group cardiothoracic surgeons are subspecialized in thoracic surgery including lung and chest wall conditions. Based on the most recent data available, cardiothoracic surgeons performed 1,134 lung surgeries in 2015, which is about 6% of all cardiothoracic surgeries performed (15). Lung transplantations are exclusively performed by dedicated cardiothoracic surgeons. These lung transplantations are concentrated in three centers: University Medical Center Groningen, University Medical Center Utrecht, and Erasmus Medical Center Rotterdam. The Netherlands is a member of Eurotransplant; an international non-profit organization that acts as a mediator between donor hospitals and transplant centers for the benefit of patients in need of an organ transplant in all its member states (16). In 2021, 92 lungs were transplanted in the Netherlands (17).
In addition to the general requirements to perform healthcare in the Netherlands as a cardiothoracic surgeon (18), cardiothoracic surgeons are required to be a member of the Dutch Association for Cardiothoracic Surgery (Dutch: Nederlandse Vereniging voor Thoraxchirurgie, NVT).
General thoracic surgeons
General thoracic surgery is concerned with surgical interventions for pathologies of the lungs, mediastinum, pleura, diaphragm, and chest wall. Esophageal surgery is seen as part of (upper) gastrointestinal surgery and is not part of the thoracic surgical spectrum. Moreover, there is an overlap in chest wall surgery as this is performed by general thoracic surgeons, cardiothoracic surgeons, trauma surgeons and pediatric surgeons. Pediatric and thoracic surgeons treat chest wall deformities such as pectus excavatum, whereas rib fixations are performed by thoracic and trauma surgeons. Additionally, most general thoracic surgeons are trained in a second subspecialty, such as oncology and gastrointestinal surgery.
In order to maintain certification, thoracic surgeons must perform a minimum of 10 anatomical resections per year (19). Moreover, thoracic surgeons are required to stay informed on the latest technical and scientific advances, querying a minimum of 10 accreditation points per year. Points are awarded for participation in (inter)national thoracic-related medical conferences (e.g., lung surgical rounds), training courses, and symposia, as well as for actively performing research and publishing in peer reviewed journals (19). Furthermore, it is mandatory to be a member of one of the dedicated professional associations, including the Dutch Society for Lung Surgery (Dutch: Nederlandse Vereniging voor Longchirurgie, NVvL) and the Dutch Society for Surgery (Dutch: Nederlandse Vereniging voor Heelkunde, NVvH).
Center requirements to perform general thoracic surgery
For certification, a thoracic surgery center must perform at least 50 thoracic (lung, mediastinal and chest wall) surgeries per year including 20 anatomical parenchymal resections per year (15,20). Following this requirement, low-volume hospitals started to collaborate to meet the volume standard or discontinued their thoracic surgery program. This has led to an increasing number of high-volume hospitals (defined as more than 50 anatomical resections per year) (14). In these so-called high-volume thoracic centers, training and implementation of physician assistants dedicated to the surgical ward and outpatient consultation, allowed for optimization of patient care as well as implementation of enhanced recovery after surgery (ERAS) protocols (21,22).
Training and education of (cardio)thoracic surgeons
To become a thoracic surgeon in the Netherlands, two paths can be followed: a general surgery residency program with a subspecialty for thoracic surgery or a cardiothoracic surgery residency program with a subspecialty for oncological pulmonary surgery, both resulting in a certification for thoracic surgery.
Training and education of a general thoracic surgeon
To become a general thoracic surgeon in the Netherlands, surgical residents undertake a 1-year sub-specialty training in thoracic surgery in the last year of their 6-year general surgery training program. At the end of the specialized education program, the resident is registered as a medical specialist with the Registration Committee of Medical Specialists (Dutch: Registratiecommissie Geneeskundig Specialisten, RGS). This period is generally continued by a one- or two-year thoracic fellowship.
The Dutch Society for Surgery is responsible for the organization of the surgical training program (23). The surgical trainee has to participate in at least 13 clinical surgical activities and 17 key procedures (24). The trainee’s progress is frequently monitored and assessed by the training supervisor, starting with evaluations every three months in the first two years, to half-year evaluations in remaining three and a half years. Amongst others, non-technical skills, Objective Structured Assessments of Technical Skills (OSATS) (25), education (e.g., courses and congresses) and scientific progress (e.g., first author publications) are examined by the training supervisor, whereas theoretical knowledge is tested by an national annual exam (26). At the end of each year of residency, the supervisor assesses if the trainee is suitable to become a general surgeon (26). After a signed declaration by the training supervisor, declaring that the trainee satisfies the requisite conditions for certification for both general surgery and the lung surgery specialization, the surgical trainee is a certified general thoracic surgeon (19).
Compared to the European Guidelines provided by European scientific societies, the Dutch training program for thoracic surgery is less strict. According to the European Guidelines, for example, a minimum of three years of exposure to thoracic surgery is prerequired within a minimum of five years of surgical training (27), while the Dutch sub-specialty training period requires only one year (26). Additionally, a minimal number of operations required to perform during the training period is not yet defined in the Netherlands, whereas the European Board of Thoracic Surgery mandates a minimum of 100 surgeries during the training period (27). Even though there is no volume-based threshold for training, a Dutch thoracic surgical trainee can only be certified as a thoracic surgeon if they achieve the minimum level of expertise per thoracic procedure after formal proficiency assessments by their supervisors. For example, a surgical trainee has to be able to perform an anatomical resection without assistance at the end of their surgical training (proficiency level D) (26).
It is estimated that each year three general thoracic surgeons can be employed in the Netherlands. As more teaching hospitals offer thoracic surgery education, there are currently about 26 general surgery residents training to become a thoracic surgeon. This labor market imbalance for general thoracic surgeons receives current attention.
Training and education of a cardiothoracic surgeon subspecialized in lung cancer surgery
Cardiothoracic surgical residents have a five-and-a-half-year training period. Every cardiothoracic resident receives a general cardiothoracic training program within the first five years, during which the residents achieve a variable degree of proficiency in 14 entrustable professional activities (EPAs) including the treatment of lung, mediastinal, chest wall and pleural diseases (28,29). In the last six months, the cardiothoracic trainee is encouraged to undertake a sub-specialty training of which lung oncology is one option, besides six other cardiac-related sub-specialty training programs (29).
In contrast to other European cardiothoracic training programs, there is no definite exam a cardiothoracic surgical residents must pass to finalize residency. Moreover, residents are not obliged to take or pass the European Board of Cardiothoracic Surgery (EBCTS) examination either, yet. Nevertheless, there are yearly theoretical examinations conducted by the Dutch Association for Cardiothoracic Surgery, and, perhaps most importantly, EPAs are continuously monitored and assessed by the trainers. These EPAs comprise both theoretical and practical knowledge and are examined using OSATS, amongst others (25). There are different stages in achieving such an EPA, which start with (I) observing, (II) performing surgery under direct supervision, (III) under indirect supervision, (IV) without supervision, and (V) as supervisor. For all general, basic EPAs, at least level four is required, which needs to be endorsed by the complete team of trainers.
Although the labor market of the cardiothoracic surgeons was in balance according to the evaluation report assessing the labor market between 2008 and 2015 (15), the ratio between cardiothoracic surgery residents who successfully completed their residency and foreign cardiothoracic surgeons versus retiring cardiothoracic surgeons and cardiothoracic surgeons who quit for other reasons, seems to be increasing.
Requirements of a general thoracic teaching institution
To become a teaching center for thoracic surgery, the following requirements have to be fulfilled in addition to the standard requirements for general surgery (24,26,30):
- Centers are required to have at least two thoracic surgeons who are certified for training and education of lung surgery;
- The thoracic surgery department has to meet the latest Dutch Society for Lung Surgery standards and the Dutch Federation of Oncological Societies (SONCOS) quality standards for lung surgery (19,31);
- The thoracic teaching hospital must perform surgeries for benign lung pathology (thoracic drainage, bullectomies, pleurectomy, lung biopsy, sympathectomy), malign lung pathology (wedge resection, (bi)lobectomy, segmentectomy, pneumonectomy, and decortication), thoracic wall and mediastinum diseases (thoracotomy, empyema drainage, thoracic wall resection, pectus treatments, thoracic wall reconstruction, mediastinoscopy and mediastinal tumor resection);
- The thoracic teaching hospital must provide internships at the radiotherapy and pulmonology department;
- A minimum requirement of at least 40 pulmonary resections in a thoracic teaching hospital.
Requirements of a cardiothoracic teaching institution
The following standards should be guaranteed for cardiothoracic teaching centers (18):
- Centers are required to have (the possibility to consult) at least five cardiothoracic surgeons who are certified for training and education, a cardiologist, an internist, a pulmonologist, a dermatologist, a geriatrician, a geriatric specialist, a gynecologist, a gastrointestinal and liver physician, an otolaryngologists, a pediatrician, a microbiologist, a neurosurgeon, a neurologist, a nuclear physician, an ophthalmologist, an orthopedic surgeon, a pathologist, a psychiatrist, a radiologist, a rehabilitation specialist, and a urologist;
- The hospital must have access to a dedicated cardiology department, dedicated intensive care unit regarding mechanical ventilation and hemodialysis, on-site 24 h molecular diagnostics, and dedicated rehabilitation ward for cardiac patients;
- A minimum requirement of at least 50 lung, mediastinal and chest wall surgeries, and 750 cardiac surgeries in a cardiothoracic teaching hospital;
- 24-hour access to cardiopulmonary bypass and extra-corporeal membrane oxygenation systems.
National quality surveillance for thoracic surgery care
In the Netherlands there is an open culture on discussions regarding complications, morbidity and mortality. These results are continuously benchmarked to provide high-quality care by means of mandatory participation in nationwide registry, institutional morbidity and mortality meetings, and non-obligatory participation in international registries, moral case deliberations (32), the encouragement in asking for second opinions and the collaboration between academic and non-academic hospitals in clinical trials and case discussions. A network of numerous competent authorities (Figure 1) regularly monitors the quality of thoracic surgery delivered at a hospital and assesses, among other things, whether the required clinical practice guidelines are being followed (e.g., SONCOS and Dutch Guideline Database).
Quality surveillance of thoracic centers
The Health and Youth Care Inspectorate (Dutch: Inspectie Gezondheidszorg en Jeugd, IGJ), the main advisory body of the Ministry of Health, Welfare and Sport, is responsible for monitoring the quality of healthcare by supervising public and private providers. Since 2004, performance indicators were introduced for measurable healthcare aspects to assess the quality, safety, efficiency and accessibility of medical services per healthcare institution (33,34). Performance indicators for thoracic surgery include the number of anatomical lung resections, the frequency of deep sternal wound infections, and mandatory participation in the nationwide registries (35). Additionally, each hospital is required to meet the latest SONCOS quality standards for quality assurance and improvement of surgical lung oncology care (31). These quality standards are developed in consultation with the Dutch medical professional associations (31). Besides the SONCOS standards for lung oncology that apply to the lung surgery department (Figure 1), each year at least 50 patients diagnosed with lung cancer have to be treated with surgery, radiation therapy, immunotherapy, chemotherapy or targeted therapy. Additionally, the hospitals are obligated to participate in the nationwide lung cancer registry, the Dutch Lung Cancer Audit (DLCA) (36).
Nationwide lung cancer registry
Across Europe, at least 30 countries collect national cancer data in 2018, with most of the data collected in a national registry for all cancers. Registries based on data collection for lung cancer specifically, and databases specific for thoracic surgery, are only performed in several countries such as Denmark, France and the Netherlands (37). The DLCA is a nationwide registry for lung cancer surgery in the Netherlands.
The DLCA was initially launched by thoracic surgeons in 2012 as Dutch Lung Surgery Audit (DLSA) to monitor and evaluate the quality of lung surgical care (14). In collaboration with the Dutch Society for Lung Surgery and the Dutch Association for Cardiothoracic Surgery, the structure and organization of the DLCA was developed. Since 2016, the registry is evolved in a nationwide multidisciplinary lung cancer registry including data from pulmonologists (DLCA-L), radiotherapists (DLCA-R), and thoracic surgeons (DLCA-S) of all Dutch hospitals and pulmonological and radiotherapeutic domains (38). As mentioned before, each hospital providing lung cancer treatments is required to participate in the national registry. These obligated nationwide DLCA registrations promote self-evaluation and self-reflection, as well as help patients select a surgery center. An obligated outcome and complication registration lowers the reserve on discussing bad outcomes and unexpected complications.
Aside from national benchmarking, three Dutch hospitals contribute in the worldwide registry of the European Society of Thoracic Surgery (ESTS) (39).
Quality surveillance of (cardio)thoracic surgeons
The Dutch Society for Surgery monitors the quality of lung (cancer) surgery every five years as part of a broad assessment of the adherence to quality standards by surgery departments. These criteria were developed in collaboration with the Dutch Society for Lung Surgery (19,20). These standards involve e.g., the presence of institutional treatment protocols, a system for reporting complications and the institutional volume-based threshold of 20 anatomical resections per year. Additionally, the surgery departments must provide thoracic surgery care in correspondence with the Dutch Guideline Database, an evidence-based database including national guidelines for secondary healthcare which are developed and updated by the Dutch Association of Medical Specialists (Dutch: Federatie Medisch Specialisten, FMS) (40). The Dutch Association for Cardiothoracic Surgery performs the quality visits of cardiothoracic departments to monitor and assure the quality of care (41). Figure 1 provides a detailed overview of the quality requirements of thoracic surgery, for lung- and cardiothoracic surgery separately.
Quality surveillance of thoracic training programs and teachers
The Registration Committee of Medical Specialists monitors the quality of training hospitals and teachers based on the standards for surgical training programs, recognition of national training programs and teachers, which are determined by the Medical Specialists Council (Dutch: College Geneeskunde Specialismen, CGS) on behalf of the Royal Dutch Medical Association (Dutch: Koninklijke Nederlandsche Maatschappij tot bevordering der Geneeskunst, KNMG).
Performance of Dutch thoracic surgery centers
The Netherlands provides high-level top clinical care for various thoracic-related procedures by, amongst others, incorporating advanced approaches and novel technologies in perioperative thoracic surgery care. It should be noted that there is no national data available regarding the number of thoracic surgical procedures except for oncological lung surgeries.
Minimally invasive lung cancer surgery
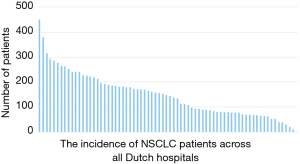
Based on the latest annual report of the DLCA registry from 2019, in total 11,852 patients were suspected of or had proven non-small cell lung cancer (36). Figure 2 presents an overview of the incidence of primary NSCLC patients per Dutch hospital. In 2019, a total of 2,246 anatomical parenchymal lung resections were performed, of which 65% were performed through video-assisted thoracic surgery (VATS, uni- and multiportal), 3% by robotic-assisted thoracic surgery (RATS), 28% by or converted to open surgery and the remaining 3% was unknown (42). The mean perioperative mortality and complication rate were, respectively, 2% and 14% (43). This is in line with the international data from the ESTS registry including data of 113,323 major lung resections with a mean 2% mortality rate and 15% cardiopulmonary complication rate (39).
Inter-hospital differences can be found in procedural volume, complications and length of hospital stay. Based on the DLCA-S hospital-specific annual report in 2020, recent inter-hospital data regarding lung cancer oncology surgery in the Netherlands was acquired. Figure 3A demonstrates the number of anatomical parenchymal resections, varying between 20 to 120 pulmonary resections. Figure 3B and Figure 3C show case-mix adjusted prevalence for respectively a complicated course and 30-day mortality after elective lung surgery and demonstrate that none of the surgery centers were reported as significant outliers when compared to the national mean. Median length of hospital stay after a thoracoscopic anatomical lung resection varies from three to eight days in the Netherlands (21), This relatively large variation may be explained by the local differences in appliance and content of the ERAS programs (21).

Chest wall surgery
Surgical correction of congenital chest wall pathology (of which pectus excavatum is the most common), is conducted in about 10 surgery centers by a selected group of thoracic surgeons. Chest wall surgery can be divided in congenital (e.g., pectus excavatum and carinatum, xiphoidectomy), trauma (e.g., surgical stabilization of rib fractures), and oncological conditions (e.g., resection of chest wall tumors with reconstruction). National data and surgical guidelines on chest wall surgeries are lacking in the Netherlands. Since chest wall surgeries are not nationally registered, the exact number of procedures and surgery centers performing these treatments is unclear. However, regarding pectus excavatum treatment, a national register for diseases leading to hospital treatment, called the Kiwa Prismant registration, recorded the number of surgical treatments for pectus excavatum (44). Despite a decrease in births, there is an increase in the frequency of pectus excavatum treatments (44). This is attributed to increasing awareness.
Thymic and mediastinal surgeries
Historically, the anterior mediastinum was approached through sternotomy, and therefore performed in many (cardio)thoracic surgery centers in the Netherlands. However, due to the relatively low incidence of anterior mediastinal masses and the advent of subspecialized minimally invasive and robotic surgery, thymic and mediastinal surgery can now be considered complex care and is only performed in selected centers; tertiary centers perform surgery of advanced thymoma (Masaoka stages > III) and mediastinal tumors (45), whereas high-volume secondary centers conduct resections of low-grade thymoma (Masaoka stages I–III) and mediastinal tumors. In these medical centers, a minimally invasive approach, either thoracoscopically or robotically, is now standard of care.
Surgical treatment of malignant pleural mesothelioma
The Netherlands ranks in the top five worldwide regarding the incidence of mesothelioma (46,47). Mesothelioma is strongly correlated with asbestos use (46-48), which application peaked between 1970 and 1980 (49). Since 1993, use of asbestos is legally prohibited in the Netherlands. Nevertheless, the long-term effects are present in daily practice with an incidence in 2018 of 3.3 cases per 100,000 person-years (49). Treatment of mesothelioma is performed in tertiary centers. Radical surgery such as extrapleural pneumonectomy is only performed in clinical studies and is not advised as standard curative treatment in the Netherlands due to the high risk of microscopic margin involvement (R1) and serious complications (>50%) (50). Surgery is usually only performed for diagnosis via a surgical pleural biopsy.
Adoption of international guidelines and novel minimally invasive techniques
Dutch thoracic surgeons are generally driven to learn and implement worldwide novel technologies and methods. Most thoracic departments adhere to the European Society of Thoracic Surgery ERAS recommendations and guidelines for work-up and treatment of lung cancer (21,22). For example, after its introduction in the Netherlands in 2006 (51), multiportal VATS was rapidly spread throughout the country resulting in implementation of the technique in more than 75% of cases of anatomical lung resections in 2012 (this data is adapted from the DLSA annual report of 2012). Likewise, uniportal VATS for anatomical resections is adopted from international courses and has been implemented in multiple Dutch hospitals. RATS is also implemented and used in the Netherlands for lung surgery in a few centers. However, in the last five years, its practice has not increased and is still the least used technique (<5%) (42).
Academic research
Most Dutch teaching hospitals have (multiple) PhD-candidates conducting research to obtain a doctoral research degree. Many medical students and surgical residents are encouraged to pursue PhD programs because of the limited number of positions in surgical training programs, and selected surgery centers expect their surgical residents to have (or obtain) academic degree (52). This may explain why the vast majority of Dutch medical specialists nowadays have an academic degree. Currently, the Netherlands has two professors of lung surgery. As surgical subspecializations grow, we expect more professors to be appointed to the field of lung surgery in the coming years.
Globally, the Netherlands ranked 14th with 1,901 clinical trials conducted across all medical disciplines in 2021 (53). Several thoracic-related (inter)national multicenter randomized trials have been initiated by Dutch hospitals and their research groups. Current studies include the OPtriAL (54), investigating the optimal postoperative pain management after lung surgery, the ERATS-trial (55), investigating the incorporation of the ERAS-protocol in lung cancer surgery, the MEDIASTrial (56,57), evaluating whether confirmatory mediastinoscopy can be omitted after tumor negative endosonography, and the FixCon study (58,59), investigating if early fixation of rib fractures is better than conservative treatment. Amidst numerous other studies being conducted, Dutch-led studies have also investigated state-of-the-art software regarding preoperative planning of lung surgery using 3-dimensional computed-tomography reconstructions (60) and virtual reality (61). Both are techniques with promising results, currently finding way into daily clinical practice.
Current challenges in thoracic surgery
An imbalanced labor market
Currently, newly graduated thoracic surgeons struggle to land a job. Having a distinction such as a PhD or prestigious fellowship or both and even multiple, is becoming average and it is becoming increasingly harder to distinguish oneself from the competition. While this can drive the overall quality of the certified surgeons and can definitely improve the overall healthcare, it is unacceptable that well-trained and highly motivated surgeons remain unemployed, not only for the personal implication for young surgeons but also because of the financial burden of surgical training, surgery departments and hospitals. This labor market imbalance for surgeons and other medical specialists is currently topic of debate.
Homogenization of training and education
The Netherlands has a particular training curriculum program for thoracic surgery, as cardiothoracic surgeons and general thoracic surgeons have a separate training curriculum, as well as separate quality rules and professional associations. Other countries have organized thoracic surgical education in a different manner. For example, the United Kingdom provides a general thoracic surgery training program for independent cardiac, thoracic, or cardiothoracic consultants (62), whereas in Australia only cardiothoracic surgeons with a small sub-specialty of thoracic (non-cardiac) surgery are employed (63). Furthermore, in the United States there are three different pathways to become a cardiothoracic surgeon or general surgeon performing thoracic surgery (64), and in Spain thoracic and cardiac surgery are monospecialties (65). Even though comparison data is lacking on performance results in thoracic surgery performed by general thoracic surgeons versus cardiothoracic surgeons in the Netherlands, the Dutch Society for Lung Surgery and the Dutch Association for Cardiothoracic Surgery are currently collaborating to integrate general thoracic surgery training and provide the same set of recertification requirements for non-cardiac thoracic surgeons in order to improve patient care.
Centralization of care
In the last few years, concentration of care has been an ongoing topic of debate among the stakeholders involved. Disregarding the drive and specific interest of the primary initiator, centralizing care, particularly complex care, has many clear benefits. Aside from improving patient outcomes, it also realizes increased experience and efficiency as well as it maintains proficiency and reduces clinical variability. The European Thoracic Surgery guidelines therefore propose a minimum volume of major thoracic procedures of more than 150 (±50) and 300 (±50) for standard and higher specialized general thoracic surgery units, respectively. Based on a large data repository analysis including 124,293 patients, hospitals with a volume of more than 150 surgical resections each year showed increased perioperative and long-term (1-year or more) survival compared to hospitals performing less than 70 procedures per year (66). Even though centralization is also associated with potential detriments, it is encouraged by several stakeholders and is expected to be implemented in different degrees and areas of (cardio)thoracic surgery. Its effect on the Dutch thoracic surgical landscape will become visible in the coming years.
Future perspectives and opportunities
Lung cancer screening of high-risk individuals
The implementation of population-based lung cancer screening of high-risk individuals could decrease the percentage of inoperable patients who are diagnosed with stage III (21%) and IV (49%) lung cancer. A Dutch-initiated randomized lung cancer screening trial, known as the NELSON trial, has recently proven to result in a decrease in lung cancer mortality by 26% and to be cost-effective in the Netherlands (67-69). Although lung cancer screening programs are currently implemented in several European centers (70), screening for lung cancer with low-dose computed tomography is presently not yet implemented in the Netherlands because of legal restrictions (67).
Promoting self-health of medical specialists
The Netherlands is one of the leading countries in promoting self-health under surgeons. There is high awareness concerning the required resting period following guards and the fitness-to-perform of the surgeon. The possibility to perform a surgical profession part-time, is becoming generally accepted for both surgical trainees and specialized surgeons. A questionary under cardiothoracic surgical residents, demonstrated that only 23% would prefer a full-time (5-day workweek) and up to 73% would prefer a 4-day workweek (15). Creating a good work-life balance, is not only better for the self-health of the surgeon but can create more job opportunities for unemployed surgeons.
National registrations for other thoracic diseases
At present, there is only a national registration for lung cancer patients (DLCA). To monitor, evaluate and improve surgical care for chest wall, mediastinal, and non-oncological pulmonary surgeries, national databases should be developed with publicly available annual reports. This information may also be useful in the development of national guidelines regarding for chest wall surgeries.
Conclusions
In general, thoracic surgery in the Netherlands has a well-organized quality structure, since thoracic-related professional associations and the government monitor surgery centers every (five) year(s), and thoracic surgeons must be recertified per five years. Furthermore, Dutch thoracic surgery is transparent due to nationwide obligated registries providing open-access annual reports. Training and education of thoracic surgery is particularly structured with separate training programs, professional associations and quality requirements for cardiothoracic surgery and general thoracic surgery. Current challenges such as the unbalanced labor market, centralization of surgical care, and the lack of mandatory data registration for non-oncological thoracic surgical care have to be addressed.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Alan D. L. Sihoe) for the series “Thoracic Surgery Worldwide” published in Journal of Thoracic Disease. The article has undergone external peer review.
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-482/prf
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-482/coif). The series “Thoracic Surgery Worldwide” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Khaitan PG, D'Amico TA. Milestones in thoracic surgery. J Thorac Cardiovasc Surg 2018;155:2779-89. [Crossref] [PubMed]
- Bevolking; geslacht, leeftijd, generatie en migratieachtergrond, 1 januari [Internet]. Centraal Bureau voor Statistiek (CBS) Statline. 2021 [cited 2022 Apr 5]. Available online: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/37325/table
- Prognose periode-levensverwachting; geslacht en leeftijd, 2021-2070 [Internet]. Centraal Bureau voor Statistiek (CBS) Statline. 2021 [cited 2022 Apr 5]. Available online: https://www.cbs.nl/nl-nl/cijfers/detail/85091NED
- OECD/European Observatory on Health Systems and Policies. Netherlands: Country Health Profile 2021:1-24. (State of Health in the EU).
- Overledenen; doodsoorzaak (uitgebreide lijst), leeftijd, geslacht [Internet]. Centraal Bureau voor Statistiek (CBS) Statline. 2022 [cited 2022 Apr 5]. Available online: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/7233/table?fromstatweb
- Maatregelen overheid om roken te ontmoedigen [Internet]. Rijksoverheid. 2020 [cited 2022 Apr 5]. Available online: https://www.rijksoverheid.nl/onderwerpen/roken/roken-ontmoedigen
- Kroneman M, Boerma W, van den Berg M, et al. Netherlands: Health System Review. Health Syst Transit 2016;18:1-240. [PubMed]
- Kerncijfers zorgverzekeraars [Internet]. Nederlandse Zorgautoriteit. 2021 [cited 2022 Apr 5]. Available online: https://www.nza.nl/zorgsectoren/zorgverzekeraars/kerncijfers-zorgverzekeraars
- Giesen P, Smits M, Huibers L, et al. Quality of after-hours primary care in the Netherlands: a narrative review. Ann Intern Med 2011;155:108-13. [Crossref] [PubMed]
- Gijsen R, Deuning C. Ziekenhuiszorg | Aanbod | Instellingen [Internet]. VZinfo.nl. [cited 2022 Apr 5]. Available online: https://www.vzinfo.nl/ziekenhuiszorg/aanbod/instellingen
- Heida JP, den Engelsen B, Baeten S, van Gent C. Product market definition in hospital care in the Netherlands [Internet]. The Hague: Strategies in Regulated Markets B.V (SiRM); 2018 Dec [cited 2022 Apr 5] p. 1-151. Available online: https://www.acm.nl/en/publications/product-market-definition-hospital-care-netherlands
- Dutch health expenditure 10th highest in Europe [Internet]. Centraal Bureau voor Statistiek (CBS). 2020 [cited 2022 Apr 10]. Available online: https://www.cbs.nl/en-gb/news/2020/47/dutch-health-expenditure-10th-highest-in-europe
- Hartoperaties in Nederland [Internet]. Hartstichting.nl. [cited 2022 Apr 5]. Available online: https://www.hartstichting.nl/hart-en-vaatziekten/hartcentra-en-vaatcentra
- Ten Berge M, Beck N, Heineman DJ, et al. Dutch Lung Surgery Audit: A National Audit Comprising Lung and Thoracic Surgery Patients. Ann Thorac Surg 2018;106:390-7. [Crossref] [PubMed]
- Siregar S, Hjörtnaes J, Palmen M, et al. Behoefteraming cardiothoracaal chirurgen 2016-2026 [Internet]. Nederlandse Vereniging voor Thoraxchirurgie; 2017 May [cited 2022 Apr 5] p. 1-33. Available online: https://www.nvtnet.nl/opleiding/behoefteraming
- Eurotransplant [Internet]. eurotransplant.org. [cited 2022 Apr 5]. Available online: https://www.eurotransplant.org/
- Yearly statistics overview [Internet]. Eurotransplant; 2021 [cited 2022 Apr 5] p. 1-3. Available online: https://www.eurotransplant.org/statistics/yearly-statistics/
- Besluit cardio-thoracale chirurgie [Internet]. College Geneeskundige Specialismen; 2018 Jan [cited 2022 Apr 5] p. 2–6. Available online: https://www.knmg.nl/opleiding-herregistratie-carriere/cgs/regelgeving/cardio-thoracale-chirurgie-3.htm
- Voorwaarden certificering [Internet]. Nederlandse Vereniging voor Longchirurgie. [cited 2022 Apr 5]. Available online: https://nvvl-longchirurgie.nl/voorwaarden-certificering
- Normering Chirurgische Behandelingen 8.1 [Internet]. Nederlandse Vereniging voor Heelkunde; 2021 Apr [cited 2022 Apr 5] p. 1-39. Available online: https://heelkunde.nl/themas/thema?dossierid=688148&title=Normering
- von Meyenfeldt EM, Hoeijmakers F, Marres GMH, et al. Variation in length of stay after minimally invasive lung resection: a reflection of perioperative care routines? Eur J Cardiothorac Surg 2020;57:747-53. [PubMed]
- Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E, et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019;55:91-115. [Crossref] [PubMed]
- Veldkamp J. General surgical training in the Netherlands. Bull R Coll Surg Engl 2007;89:92-3. [Crossref]
- Besluit Heelkunde 2021 [Internet]. College Geneeskundige Specialismen; 2021 Jan [cited 2022 Apr 5] p. 1-8. Available online: https://www.knmg.nl/opleiding-herregistratie-carriere/cgs/regelgeving/heelkunde-1.htm
- Martin JA, Regehr G, Reznick R, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 1997;84:273-8. [PubMed]
- Opleidingsplan Heelkunde SCHERP 2.1 [Internet]. College Geneeskundige Specialismen; 2021 Jan [cited 2022 Apr 5] p. 1-170. Available online: https://www.knmg.nl/opleiding-herregistratie-carriere/cgs/regelgeving/heelkunde-1.htm
- Brunelli A, Falcoz PE, D'Amico T, et al. European guidelines on structure and qualification of general thoracic surgery. Eur J Cardiothorac Surg 2014;45:779-86. [Crossref] [PubMed]
- Brasel KJ, Klingensmith ME, Englander R, et al. Entrustable Professional Activities in General Surgery: Development and Implementation. J Surg Educ 2019;76:1174-86. [Crossref] [PubMed]
- Opleidingsplan cardiothoracale chirurgie [Internet]. Nederlandse Vereniging voor Thoraxchirurgie; 2018 [cited 2022 Apr 5] p. 1-88. Available online: https://www.nvtnet.nl/opleiding/opleidingsplan
- Go/No Go voor alle differentiaties versie 3 [Internet]. Nederlandse Vereniging voor Heelkunde; 2019 Oct [cited 2022 Apr 5] p. 1-9. Available online: https://heelkunde.nl/themas/thema?dossierid=688137&title=Erkenning%252bopleiding
- SONCOS normeringsrapport - versie 9 [Internet]. Stichting Oncologische Samenwerking; 2021 [cited 2022 Apr 5] p. 1-48. (Multidisciplinaire normering oncologische zorg in Nederland). Available online: https://www.soncos.org/kwaliteit/normeringsrapport/
- What is Moral Case Deliberation [Internet]. Amsterdam Universitair Medisch Centra. [cited 2022 Apr 5]. Available online: https://www.vumc.nl/research/ethiek-recht-humaniora/dienstverlening-support/ethiek-support-ethics-support/wat-is-moreel-beraad-what-is-moral-case-deliberation.htm#:~:text=Een%20Moreel%20Beraad%20is%20een,met%20behulp%20van%20een%20gespreksleider
- van der Voort H, Kerpershoek E. Measuring measures: introducing performance measurement in the Dutch health care sector. Public Money Manag 2009;30:63-8. [Crossref]
- Inspectie Gezondheidszorg en Jeugd [Internet]. IGJ.nl. [cited 2022 Apr 5]. Available online: https://www.igj.nl/
- Indicatoren Hartchirurgie [Internet]. Nederlandse Vereniging voor Thoraxchirurgie. [cited 2022 Apr 5]. Available online: https://www.nvtnet.nl/kwaliteit/indicatoren
- Dutch Institute for Clinical Auditing [Internet]. DICA. [cited 2022 Apr 5]. Available online: https://dica.nl/dlca/home
- Rich A, Baldwin D, Alfageme I, et al. Achieving Thoracic Oncology data collection in Europe: a precursor study in 35 Countries. BMC Cancer 2018;18:1144. [Crossref] [PubMed]
- Groei van de Dutch Lung Cancer Audit (DLCA) [Internet]. DICA. 2017 [cited 2022 Apr 5]. Available online: https://dica.nl/jaarrapportage-2017/dlca
- Falcoz PE. ESTS Database annual report [Internet]. European Society of Thoracic Surgeons; 2021 Jun [cited 2022 Apr 5] p. 1-72. Available online: https://www.ests.org/ests_database/database_reports.aspx
- Over de Richtlijnendatabase [Internet]. Richtlijnendatabase. [cited 2022 Apr 5]. Available online: https://richtlijnendatabase.nl/instructies.html
- Handboek kwaliteitsvisitatie [Internet]. Nederlandse Vereniging voor Thoraxchirurgie; 2020 Jan [cited 2022 Apr 5] p. 1-66. Available online: https://www.nvtnet.nl/kwaliteit/kwaliteitsvisitaties
- Basistabel DLCA-S (2015-2019) [Internet]. Dutch Institute for Clinical Auditing; 2019 [cited 2022 Apr 5]. Available online: https://dica.nl/dlca/home
- Beck N, Hoeijmakers F, van der Willik EM, et al. National Comparison of Hospital Performances in Lung Cancer Surgery: The Role of Case Mix Adjustment. Ann Thorac Surg 2018;106:412-20. [Crossref] [PubMed]
- Zuidema WP, van der Steeg AFW, Oosterhuis JWA, et al. Trends in the Treatment of Pectus Excavatum in the Netherlands. Eur J Pediatr Surg 2021;31:261-5. [Crossref] [PubMed]
- Marcuse F, Hochstenbag M, De Baets MHV, et al. Robotic Thymectomy for Thymomas: A Retrospective Follow-up Study in the Netherlands. Ann Thorac Surg 2021; Epub ahead of print. [Crossref] [PubMed]
- Bianchi C, Bianchi T. Global mesothelioma epidemic: Trend and features. Indian J Occup Environ Med 2014;18:82-8. [Crossref] [PubMed]
- Bianchi C, Bianchi T. Malignant mesothelioma: global incidence and relationship with asbestos. Ind Health 2007;45:379-87. [Crossref] [PubMed]
- Stayner L, Welch LS, Lemen R. The worldwide pandemic of asbestos-related diseases. Annu Rev Public Health 2013;34:205-16. [Crossref] [PubMed]
- van Kooten JP, Belderbos RA, von der Thüsen JH, et al. Incidence, treatment and survival of malignant pleural and peritoneal mesothelioma: a population-based study. Thorax 2022; Epub ahead of print. [Crossref] [PubMed]
- Richtlijn diagnostiek en behandeling van het mesothelioom [Internet]. Nederlandse Vereniging van Artsen voor Longziekten en Tuberculose; 2011 Sep [cited 2022 Apr 5] p. 1-33. Available online: https://www.nvalt.nl/kwaliteit/richtlijnen/oncologie/
- Belgers EH, Siebenga J, Bosch AM, et al. Complete video-assisted thoracoscopic surgery lobectomy and its learning curve. A single center study introducing the technique in The Netherlands. Interact Cardiovasc Thorac Surg 2010;10:176-80. [Crossref] [PubMed]
- Wijnhoven BPL. Surgical training and research in the Netherlands. Keio J Med 2019;68:68. [Crossref] [PubMed]
- Number of trial registrations by location, disease, phase of development, age and sex of trial participants (1999-2021) [Internet]. 2022 [cited 2022 Apr 5]. Available online: https://www.who.int/observatories/global-observatory-on-health-research-and-development/monitoring/number-of-trial-registrations-by-year-location-disease-and-phase-of-development
- Trial NL9243, Optimal postoperative Pain management After Lung surgery (OPtriAL): multicenter randomised clinical trial [Internet]. Utrecht, the Netherlands: Cochrane Netherlands; 2021 Apr [cited 2022 Apr 5]. Available online: https://www.trialregister.nl/trial/9243
- Meyenfeldt EMV, van Nassau F, de Betue CTI, et al. Implementing an enhanced recovery after thoracic surgery programme in the Netherlands: a qualitative study investigating facilitators and barriers for implementation. BMJ Open 2022;12:e051513. [Crossref] [PubMed]
- Bousema JE, Annema JT, van der Heijden EHFM, et al. MEDIASTinal staging of non-small cell lung cancer by endobronchial and endoscopic ultrasonography with or without additional surgical mediastinoscopy (MEDIASTrial): a statistical analysis plan. Trials 2021;22:168. [Crossref] [PubMed]
- Trial NL6344, MEDIASTinal staging of non-small cell lung cancer by endobronchial and endoscopic ultrasonography with or without additional surgical mediastinoscopy [Internet]. Utrecht, the Netherlands: Cochrane Netherlands; 2017 Jul [cited 2022 Apr 5]. Available online: https://www.trialregister.nl/trial/6344
- Trial NL7043, Early Fixation versus Conservative therapy of multiple, simple rib fractures (FixCon); a multicenter randomized controlled trial [Internet]. Utrecht, the Netherlands: Cochrane Netherlands; 2019 Jan [cited 2022 Apr 5]. Available online: https://www.trialregister.nl/trial/7043
- Wijffels MME, Prins JTH, Polinder S, et al. Early fixation versus conservative therapy of multiple, simple rib fractures (FixCon): protocol for a multicenter randomized controlled trial. World J Emerg Surg 2019;14:38. [Crossref] [PubMed]
- Sardari Nia P, Olsthoorn JR, Heuts S, et al. Interactive 3D Reconstruction of Pulmonary Anatomy for Preoperative Planning, Virtual Simulation, and Intraoperative Guiding in Video-Assisted Thoracoscopic Lung Surgery. Innovations (Phila) 2019;14:17-26. [Crossref] [PubMed]
- Sadeghi AH, Maat APWM, Taverne YJHJ, et al. Virtual reality and artificial intelligence for 3-dimensional planning of lung segmentectomies. JTCVS Tech 2021;7:309-21. [Crossref] [PubMed]
- Pons A, Lim E. Thoracic surgery in the UK. J Thorac Dis 2022;14:575-8. [Crossref] [PubMed]
- Wright GM. Thoracic surgery in Australia. J Thorac Dis 2022;14:579-84. [Crossref] [PubMed]
- Byrd CT, Williams KM, Backhus LM. A brief overview of thoracic surgery in the United States. J Thorac Dis 2022;14:218-26. [Crossref] [PubMed]
- Varela G, Hernando-Trancho F, Rodríguez Suárez PM, et al. Thoracic surgery in Spain. J Thorac Dis 2022;14:779-87. [Crossref] [PubMed]
- Lüchtenborg M, Riaz SP, Coupland VH, et al. High procedure volume is strongly associated with improved survival after lung cancer surgery. J Clin Oncol 2013;31:3141-6. [Crossref] [PubMed]
- Hendriks LEL, Dingemans AC, De Ruysscher DKM, et al. Lung Cancer in the Netherlands. J Thorac Oncol 2021;16:355-65. [Crossref] [PubMed]
- de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N Engl J Med 2020;382:503-13. [Crossref] [PubMed]
- Al Khayat MNMT, Eijsink JFH, Postma MJ, et al. Cost-effectiveness of screening smokers and ex-smokers for lung cancer in the Netherlands in different age groups. Eur J Health Econ 2022;23:1221-7. [Crossref] [PubMed]
- van der Aalst CM, Ten Haaf K, de Koning HJ. Implementation of lung cancer screening: what are the main issues? Transl Lung Cancer Res 2021;10:1050-63. [Crossref] [PubMed]


