
Mechanical complications of acute myocardial infarction: a not “mechanical” preventive and therapeutic strategy
Mechanical complications (MC) remain a rare but devastating complication of myocardial infarction (MI). The most communally encountered MC in clinical practice are ventricular septal rupture, papillary muscle rupture and free wall rupture.
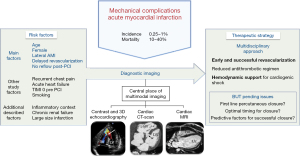
Although the reperfusion strategy using fibrinolytic or primary percutaneous coronary intervention (PCI) has significantly reduced the rate of MC over the past 30 years, the incidence of MC reported in the largest study to date is 0.27% but remains associated with very high rate of in-hospital mortality (1). Unfortunately, despite numerous technical progresses, no evidence of reduction of this mortality rate has been observed over the past two decades (2). The recent context of the COVID-19 pandemic roughly reminded us the prognostic impact of MC. Several reports have observed a decrease of ST-segment elevation myocardial infarction (STEMI) admission and a longer ischemic time associated with an increase of MC and a subsequent unusual over-mortality (3,4). It will at least have enabled these classical, but almost forgotten, complications of MI to back to stage.
In this issue of the Journal of Thoracic Disease, Xu et al. (5) have performed a case control study from a total of 22,016 STEMI patients admitted in two Chinese hospitals from 2013 to 2021. A total of 195 patients with MC (0.53% of the population) were analyzed and compared with a control group of 390 patients. The authors aimed to highlight factors independently associated with the occurrence of MC. Among them, female gender, age, total ischemic time, and post-PCI no reflow are well-known factors associated with MC (4). On the other hand, the authors underline the 5-fold higher risk of MC in high lateral wall acute MI (AMI). It is an interesting and relative new finding with practical implications as a suggested longer monitoring or more frequent echocardiogram controls. The authors speculated some technical and anatomic reasons for this observation. However, despite based on a large cohort, some limitations of this study should be considered. Beyond the observational design and subsequent limitations, the results cannot be easily extrapolated to the majority of actual populations with a very low rate of primary PCI, observed in only half of STEMI patients while it was by far the more effective strategy to reduce incidence of MC. Moreover, the definition of MC is not clearly reported and no centralized cardiac imaging was proposed with a potential underestimation of MC incidence and subsequent inadequate conclusions concerning risk factors.
However, the diagnosis of MC remains challenging. It should be systematically researched in case of new cardiac murmur, acute heart failure or cardiogenic shock, particularly within the 5 days following AMI. Besides the physical examination, imaging tests such as two-dimensional echocardiography and colour Doppler are useful and practical, since they have high specificity and can be performed at bedside. Trans-thoracic echocardiography is the fist-line exam but the sensibility of echocardiography is limited particularly in case of very apical or basal septal defect. Timing of the clinical presentation is key for establishing the differential diagnosis and deciding the urgency and type of imaging required for the management of patients. In hemodynamically stable patients, a multimodal imaging including trans-oesophageal echocardiography, cardiac computed tomography (CT) scan or magnetic resonance imaging (MRI) could be useful to improve the diagnostic performance in case of uncertain echocardiographic findings. Moreover, for the management of septal defect, these additional imaging exams allow accurate measurements to evaluate feasibility of percutaneous closure.
Besides conventional management of acute heart failure and cardiogenic shock, the therapeutic strategy of MC is based on hemodynamic support and percutaneous or surgical reparation particularly in case of septal defect. Although it was largely downgraded in cardiogenic shock recommended management without demonstrated clinical benefit (6), intra-aortic balloon pump seems to keep a key indication for treatment of MC by reducing left ventricular pressure and reduce myocardial oxygen consumption, improve coronary blood flow, limiting infarct extension and buying time for the hibernating myocardium to recover. Even if the treatment of free wall rupture is unfortunately rarely possible, specific management should be proposed for other complications: urgent valvular surgery for massive mitral insufficiency and closure of septal defect. For this specific case, the optimal timing remains controversial. Although based on observational studies, the lower mortality window seems to be following day 4 after the diagnosis to avoid prolonged support associating with more vascular, thrombotic or bleeding complications and the beginning of septal cicatrisation (7).
The optimal choice between surgery and percutaneous closure remains also controversial. To date, there are not defined specific factors to predict successful of procedure and subsequent reduction of clinical events. In the present study, surgical repair was the preferred definitive treatment of septal reparation despite a very high one-year rate of mortality observed in 54.6% of patients. Nevertheless, although there was not really discussed by the authors, percutaneous closure of septal defect appears, henceforth, proposed in first line in most intensive and cardiac teams following technical progresses and physician expertise. As a consequence, surgery should be limited to relatively rare unattainable percutaneous closure as very basal or apical septal defect, very large defect, bulky intracardiac thrombus, no percutaneous access and, obviously, limited to operable patient without inacceptable comorbidities or hemodynamic instability.
In conclusion, the diagnostic and treatment of MC is unfortunately not always “mechanical” for physicians. Despite a significant reduction of incidence, cardiologists and intensivists need to keep vigilant in the acute phase of MI using in particular multimodal imaging to avoid missing the diagnostic of MC that remains a real milestone of patient prognostic. However, as suggested in the following take home figure (Figure 1), beyond the usual clinical presentations, risk factors of mechanical complication after MI as predictive factors of a successful closure need to be completed by further studies to improve the management of these highly severe patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Thoracic Disease. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-2022-09/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Elbadawi A, Elgendy IY, Mahmoud K, et al. Temporal Trends and Outcomes of Mechanical Complications in Patients With Acute Myocardial Infarction. JACC Cardiovasc Interv 2019;12:1825-36. [Crossref] [PubMed]
- Moreyra AE, Huang MS, Wilson AC, et al. Trends in incidence and mortality rates of ventricular septal rupture during acute myocardial infarction. Am J Cardiol 2010;106:1095-100. [Crossref] [PubMed]
- Bonnet G, Weizman O, Trimaille A, et al. Characteristics and outcomes of patients hospitalized for COVID-19 in France: The Critical COVID-19 France (CCF) study. Arch Cardiovasc Dis 2021;114:352-63. [Crossref] [PubMed]
- Bouisset F, Deney A, Ferrières J, et al. Mechanical complications in ST-elevation myocardial infarction: The impact of pre-hospital delay. Int J Cardiol 2021;345:14-9. [Crossref] [PubMed]
- Xu Z, Li Y, Zhang R, et al. Risk factors for cardiac rupture after acute ST-segment elevation myocardial infarction during the percutaneous coronary intervention era: a retrospective case-control study. J Thorac Dis 2022;14:1256-66. [Crossref] [PubMed]
- Thiele H, Zeymer U, Neumann FJ, et al. Intraaortic balloon support for myocardial infarction with cardiogenic shock. N Engl J Med 2012;367:1287-96. [Crossref] [PubMed]
- Sánchez Vega JD, Alonso Salinas GL, Viéitez Florez JM, et al. Optimal surgical timing after post-infarction ventricular septal rupture. Cardiol J 2022; Epub ahead of print. [Crossref] [PubMed]


