Video-assisted thoracoscopic bronchoplasty/pulmonary arterial angioplasty
Introduction
Central-type lung cancer can invade both bronchial openings and pulmonary artery. For these patients, bronchoplasty/pulmonary arterial angioplasty is often preferred. This surgery requires the simultaneous reconstruction of airway and blood vessel, which can be particularly challenging. In the past, it was often done by using a conventional incision or video-assisted thoracoscopic small incision. In recent years, anecdotal evidences have described the application of complete video-assisted thoracic surgery (c-VATS) bronchoplasty/pulmonary arterial angioplasty in the treatment of this condition (1,2). VATS bronchoplasty/pulmonary arterial angioplasty in the left upper lobe (LUL) is the most commonly applied in clinical settings and will be described here.
Anesthesia
After the induction of general anesthesia, the patient is under double-lumen endotracheal intubation.
Body position
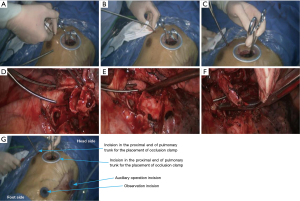
The patient is often placed in a lateral decubitus position on the unaffected side (Figure 1). The waist bridge is elevated to maximize the intercostal spaces and thus facilitate the operation.
Design of incisions
Typically three incisions will be used: observation port (incision): in the 6th or 7th intercostal space at anterior axillary line, about 1cm in length. Main operation incision: in the 3rd or 4th intercostal space at anterior axillary line, about 4 cm in length. Auxiliary operation incision: within the same intercostal space with the observation port; in the 6th or 7th intercostal space at posterior axillary line, about 1 cm in length. Under general anesthesia with double lumen tube, video-assisted thoracoscopic bronchoplasty/pulmonary arterial angioplasty was performed on January 16th 2014 (Figure 2).
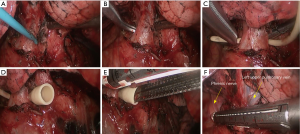
- Dissect the mediastinal pleura with an electric knife. After the tissues around the left upper pulmonary vein are thoroughly dissociated and thus the vein is roughly skeletonized, dissociate the left upper pulmonary vein using a pair of right-angle forceps and then transect the vein using the endoscopic cutter/stapler. The pulmonary fissure is cut open to expose the upper lobe branch of the right upper pulmonary vein, which is then transected using the endoscopic cutter/stapler (Figure 3). To facilitate the stapler to pass through the intervascular space, a silk suture can be used to lift the vein and the endoscopic cutter/stapler can be guided by a urinary catheter.
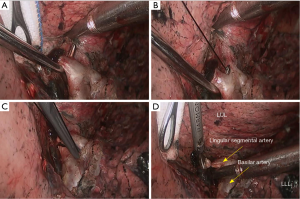
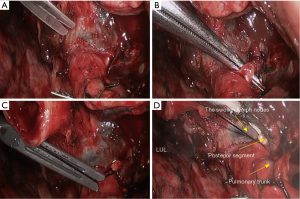
- The left upper lung is lifted upwards for dissecting the pulmonary arterial sheath. Dissect to expose the pulmonary arterial branch in lingular segment of the LUL and then transect it with high intensity focused ultrasound (HIFU) after it is blocked off with thread ligation (Figure 4). The pulmonary arterial branch in posterior segment of the LUL is managed using the same method, followed by the dividing of oblique fissures (Figure 5).
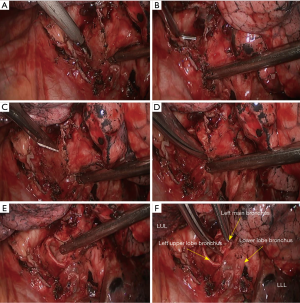
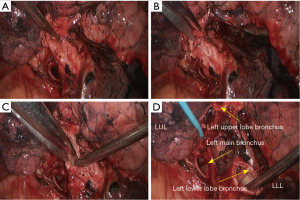
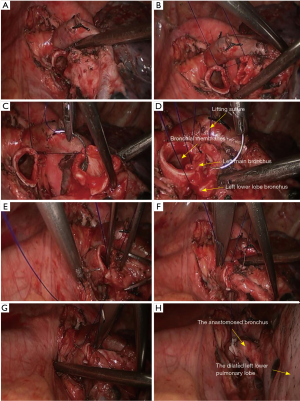
- The left upper lung is lifted upwards to dissociate the LUL bronchus and then transect it (Figure 6). The left lower lobe (LLL) bronchus is dissociated and transected using the same method (Figure 7).
- A 0.5-cm incision is made in the 2nd intercostal space on the anterior chest wall. A thoracoscopic blocking clamp is placed to block off the proximal end of pulmonary trunk. The blocking clamp is inserted via the main operation incision or auxiliary operation incision to block off the distal end of pulmonary trunk (Figure 8).
- After the pulmonary trunk is blocked, the dissection continues to dissociate the posterior segment of LUL artery, which is then ligated with silk suture and transected with HIFU (Figure 9).
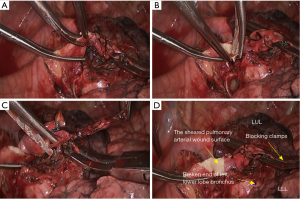
- Remove parts of the pulmonary artery wall, followed by the resection of the left upper pulmonary lobe, which can be temporarily remained inside the pleural space (Figure 10).
- Shearing of the resection margin of the pulmonary artery (Figure 11).
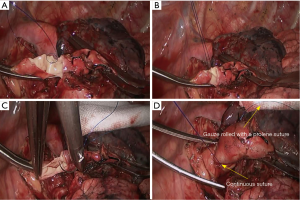
- Pulmonary angioplasty is performed using a 4-0 prolene suture in a continuous simple suture. After the first knot tied with a needle, one suture can be rolled onto a gauze before it is placed into the pleural cavity, so as to avoid entangling of these two sutures during wound closure (Figure 12). Notice: the prolene suture that is temporarily not used for closure can be rolled onto a gauze to avoid the entangling of two sutures.
- The anastomoses of bronchial membranes and cartilages are also performed using the continuous simple suture technique using 3-0 prolene sutures (Figure 13).


Discussion
Concurrent sleeve bronchoplasty and pulmonary arterial angioplasty is a highly challenging thoracic surgery and was even contraindicated in some centers. Safe and effective occlusion of pulmonary artery under thoracoscope is a key step in this surgery. Yu et al. (2) reported 21 patients who had undergone pulmonary lobectomy combined with pulmonary arterioplasty by c-VATS, among whom nine received strict pulmonary artery end-side anastomosis and 12 underwent local resection of pulmonary arterioplasty. The thoracoscopic blocking clamp is used to block pulmonary arteries. Nakanishi et al. (4) described the application of c-VATS lobectomy with partial removal of the pulmonary artery in five patients; in their operations, the conventional thoracotomic vascular blocking clamp was used; the incisions included a 7-cm main operation port and three 12-mm trocar ports in different intercostal spaces for vascular blocking, observation, and lifting.
In our center, we had blocked pulmonary artery using thoracoscopic blocking clamp before the operations; in some other cases, however, we also blocked the pulmonary artery with the conventional thoracotomic vascular blocking clamp after making three incisions, during which no thoracoscopic device is required (5). During the arterial anastomosis, the 4-0 absorbable sutures can be used for continuous suture, which can be performed clockwise along the posterior wall, lower wall, anterior wall, and upper wall. Although the 3-port method and the use of conventional vascular blocking clamp may affect the operation, operators with rich VATS experiences can still smoothly complete vascular anastomosis.
When this procedure is performed under thoracoscope, sleeve bronchoplasty can be performed after pulmonary artery anastomosis, so as to shorten the time required for pulmonary artery blockage. While there are a variety of sleeve bronchoplasty methods, interrupted anastomosis or continuous anastomosis combined with interrupted anastomosis is the major technique used in previous literature. According to our experiences (6), the continuous suture is safe and simple, during which the 3-0 prolene suture is commonly used. However, entangling of sutures may occur during the continuous suture under thoracoscope. After the first stitch, we introduce one end of the Prolene suture from the auxiliary port; then, a suction device is inserted via the auxiliary port to help the operator to wipe the suture, so as to avoid the entangling of sutures. Alternatively, two Prolene sutures that are temporarily not sutured can be rolled onto a gauze before they are placed into the pleural cavity, which can also effectively prevent the entangling of sutures.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Liu L, Mei J, Pu Q, et al. Thoracoscopic bronchovascular double sleeve lobectomy for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;46:493-5. [Crossref] [PubMed]
- Yu DP, Han Y, Zhao QY, et al. Pulmonary lobectomy combined with pulmonary arterioplasty by complete video-assisted thoracic surgery in patients with lung cancer. Asian Pac J Cancer Prev 2013;14:6061-4. [Crossref] [PubMed]
- Chen H, Xu X, He J, et al. Under general anesthesia with double lumen tube, video-assisted thoracoscopic bronchoplasty/pulmonary arterial angioplasty. Asvide 2016;3:150. Available online: http://www.asvide.com/articles/905
- Nakanishi R, Yamashita T, Oka S. Initial experience of video-assisted thoracic surgery lobectomy with partial removal of the pulmonary artery. Interact Cardiovasc Thorac Surg 2008;7:996-1000. [Crossref] [PubMed]
- Huang J, Li J, Qiu Y, et al. Thoracoscopic double sleeve lobectomy in 13 patients: a series report from multi-centers. J Thorac Dis 2015;7:834-42. [PubMed]
- Xu X, Chen H, Yin W, et al. Thoracoscopic half carina resection and bronchial sleeve resection for central lung cancer. Surg Innov 2014;21:481-6. [Crossref] [PubMed]



