
The association of coronary non-calcified plaque loading based on coronary computed tomography angiogram and adverse cardiovascular events in patients with unstable coronary heart disease-a retrospective cohort study
Introduction
Coronary atherosclerotic heart disease is currently one of the most clinically common cardiovascular diseases, mostly occurring in middle-aged and elderly people, and often leads to higher case fatality and disability rates (1,2). Unstable coronary artery disease is a more common manifestation of coronary heart disease (CHD), and its early prevention and diagnosis and treatment have become hot spots and difficulties in clinical practice. Although some scholars regarded interleukin-18 and high-sensitivity C-reactive protein as predictors of adverse cardiovascular events in CHD patients, these two indicators are not specific and can be increased in many diseases. In recent years, studies have found that coronary computed tomography angiogram (CCTA) has the characteristics of non-invasive, high resolution, and can accurately determine the characteristics of tubular wall plaques, which has high application value in the diagnosis of CHD (3,4). Coronary plaque loading can be divided into calcified plaque loading and non-calcification plaque loading, although calcified plaque loading also has a certain impact on coronary blood flow, but because the calcification plaque is relatively stable, it is not easy to fall off, so it does not often lead to myocardial infarction. However, non-calcified plaque loading is easy to fall off, non-calcified plaques account for the majority of the coronary plaques, its main component is cholesterol, the outer layer of non-calcific plaque only covers the fiber cap, so it is easy to fall off, leading to myocardial infarction (5-7). The present study was to investigate the association of coronary non-calcified plaque loading and adverse cardiovascular events in patients with unstable CHD. We present the following article in accordance with the STARD reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-933/rc).
Methods
Participants
We retrospectively and continuously collected 206 patients with unstable CHD who were treated at the 74 Group Military Hospital of PLA Army from January 2018 to September 2020. The enrollment criteria were as follows: (I) unstable CHD; (II) CCTA had been performed; (III) age 18–80 years; and (IV) complete clinical data. The exclusion criteria were as follows: (I) acute pericarditis; (II) myocarditis; (III) electrolyte abnormalities; (IV) malignant tumors or serious cardiopulmonary, liver, kidney, and autoimmune diseases; and (V) pregnant and lactating women. All cases were followed up for 1 year and divided into an observation group (group with adverse events, n=56) and a control group (no adverse events, n=150). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of 74 Group Military Hospital of PLA Army (No. 2021087). Individual consent for this retrospective analysis was waived.
CCTA examination
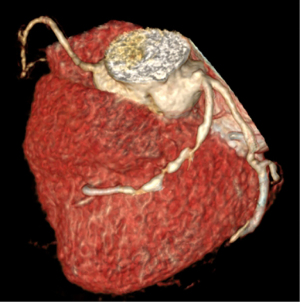
A Siemens Dual Source Spiral CT (Siemens, Erlangen Germany) was used to perform CCTA. The parameter settings were as follows: tube voltage 120 kV, current 80 mA, pitch 0.15–0.21 mm, scanning time 7–11 s, and thickness 0.620 mm, speed 0.25 s/rpm. Contrast medium was injected intravenously through the elbow using a high-pressure syringe, and 85–90 mL of Ultravist (Bayer HealthCare, Berlin, Germany) and 40 mL of normal saline were injected at a rate of 4.5–5.5 mL/s, and then scanned. The collected primary data were transferred to the workstation for image reconstruction and analysis of blood vessel stenosis and plaque nature. Non-calcification loading of coronary arteries was determined as follows: calculate the non-calcified plaque volume, vascular volume, non-calcifying plaque loading, non-calcification plaque loading = non-calcified plaque volume/vascular volume (Figure 1).
Data collection
The following data were collected: (I) general information such as age, gender, body mass index (BMI), hypertension, diabetes, history of alcoholism, smoking history, and disease history. (II) Non-calcified plaque volume, vascular volume, and non-calcifying plaque loading. (III) Carotid intima-media thickness and left ventricular ejection fraction (LVEF).
Diagnostic method
Adverse cardiovascular events: all the patients were followed up for 1 year after surgery, an adverse cardiovascular event was defined if the patient experienced angina, cardiac insufficiency, occasional malignant arrhythmias, malignant arrhythmias, recurrent myocardial infarction, heart failure, or cardiac arrest.
Statistical analysis
The data analysis was conducted using the software SPSS 26.0 (IBM Corp., Armonk, NY, USA), and P<0.05 indicated that the difference was statistically significant (two-sided). The measured data of both groups of patients were in line with the normal distribution, and the differences between the two groups were analyzed by independent sample t-test. The differences of counting data between the two groups were analyzed by chi-square test; The diagnostic value of coronary non-calcified plaque loading parameters for adverse cardiovascular events was analyzed by receiver operating characteristic (ROC) curve test. Risk factors for adverse cardiovascular events in patients with unstable CHD were investigated using multivariate logistics regression analysis.
Results
Comparison of general data of patients between the two groups
The proportion of hypertensive patients in the observation group was significantly higher than that in the control group (75.00% vs. 53.33%, P=0.005). There was no significant statistical difference in other general clinical data between the two groups (P>0.05) (Table 1).
Table 1
| Grouping | Observation group (n=56) | Control group (n=150) | t/χ2 value | P value |
|---|---|---|---|---|
| Gender (male) | 30 (53.57%) | 84 (56.00%) | 0.097 | 0.755 |
| Diabetes | 35 (62.50%) | 73 (48.67%) | 3.129 | 0.077 |
| Hypertension | 42 (75.00%) | 80 (53.33%) | 7.927 | 0.005 |
| History of smoking | 26 (46.43%) | 68 (45.33%) | 0.019 | 0.888 |
| Alcoholism | 30 (53.57%) | 76 (50.67%) | 0.138 | 0.710 |
| Average age (years) | 64.23±3.56 | 63.53±3.67 | 1.229 | 0.221 |
| Average course (years) | 8.34±5.34 | 7.86±5.26 | 0.580 | 0.562 |
| Average BMI (kg/cm2) | 30.26±4.23 | 29.78±4.17 | 0.732 | 0.465 |
Smoking history: ≥1 cigarette per day for 1 year, or the total amount of smoking ≥360 cigarettes per year; alcoholism: drinking ≥2 times a week, liquor ≥50 mL each time, or beer ≥500 mL each time. SD, standard deviation; BMI, body mass index.
Comparison of non-calcified plaque loading in coronary arteries between the two groups
Compared with the control group, the non-calcified plaque volume of the cases in the observation group was significantly increased (160.10±44.02 vs. 128.06±42.22 mm3, P=0.000). Non-calcified plaque loading was significantly increased (26.93%±7.98% vs. 21.46%±7.62%, P=0.000) (Table 2).
Table 2
| Grouping | Observation group (n=56) | Control group (n=150) | t value | P value |
|---|---|---|---|---|
| Non-calcified plaque volume (mm3) | 160.10±44.02 | 128.06±42.22 | 4.791 | 0.000 |
| Vascular volume (mm3) | 600.87±60.60 | 603.97±57.77 | 0.339 | 0.735 |
| Non-calcified plaque loading (%) | 26.93±7.98 | 21.46±7.62 | 4.529 | 0.000 |
SD, standard deviation.
Comparison of LVEF and carotid intima-media thickness between the two groups
Compared with the control group, the carotid intima-media thickness of the observation group was significantly increased (1.49±0.17 vs. 1.40±0.18 mm, P=0.001) and LVEF was significantly reduced (53.28%±7.39% vs. 58.02%±7.91%, P=0.000) (Table 3).
Table 3
| Grouping | Observation group (n=56) | Control group (n=150) | t value | P value |
|---|---|---|---|---|
| Carotid intima-media thickness (mm) | 1.49±0.17 | 1.40±0.18 | 3.389 | 0.001 |
| LVEF (%) | 53.28±7.39 | 58.02±7.91 | 3.895 | 0.000 |
LVEF, left ventricular ejection fraction; SD, standard deviation.
Diagnostic value of different indicators for recurrence of adverse cardiovascular events in patients with unstable CHD within 1 year
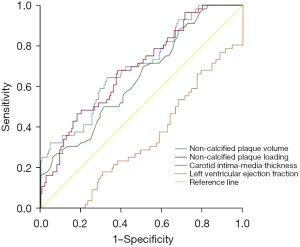
Non-calcified plaque volume, non-calcified plaque loading, carotid intima-media thickness, and LVEF all had certain diagnostic value for adverse cardiovascular events that recur within one year in patients with unstable CHD (P<0.05) (Table 4 and Figure 2).
Table 4
| Variables | AUC | SE | P value | 95% AUC | Optimal diagnostic cut-offs |
|---|---|---|---|---|---|
| Non-calcified plaque volume (mm3) | 0.698 | 0.041 | 0.000 | 0.618–0.778 | 145.58 mm3 |
| Non-calcified plaque loading (%) | 0.688 | 0.040 | 0.000 | 0.609–0.767 | 23.40% |
| Carotid intima-media thickness (mm) | 0.641 | 0.042 | 0.002 | 0.558–0.725 | 1.515 mm |
| LVEF (%) | 0.336 | 0.041 | 0.000 | 0.256–0.417 | 56.57% |
CHD, coronary heart disease; AUC, area under the curve; SE, standard error; LVEF, left ventricular ejection fraction.
Risk factors for recurrence of adverse cardiovascular events in patients with unstable CHD within 1 year
Multivariate logistics regression analysis showed that the non-calcified plaques volume >145.58 mm3, the carotid intima-media thickness >1.515 mm, the LVEF <56.57%, and hypertension were risk factors for recurrence of adverse cardiovascular events within 1 year in patients with unstable CHD (P<0.05) (Table 5).
Table 5
| Variables | B value | S.E. | Wald | P value | Exp(B) | 95% CI |
|---|---|---|---|---|---|---|
| Non-calcified plaque volume >145.58 mm3 | 1.206 | 0.346 | 12.134 | 0.000 | 3.340 | 1.695–6.584 |
| Carotid intima-media thickness >1.515 mm | 0.701 | 0.351 | 3.979 | 0.046 | 2.015 | 1.012–4.010 |
| LVEF <56.57% | 0.978 | 0.351 | 7.737 | 0.005 | 2.658 | 1.335–5.294 |
| Hypertension | 0.758 | 0.375 | 4.080 | 0.043 | 2.135 | 1.023–4.456 |
| Constant | −4.411 | 1.017 | 18.825 | 0.000 | 0.012 | – |
CHD, coronary heart disease; S.E., standard error; CI, confidence interval; LVEF, left ventricular ejection fraction.
Discussion
With the change of people’s lifestyle, unstable CHD has gradually become an important disease that threatens human life and health. Clinically, the degree of vascular stenosis in coronary angiography is mostly used as the “gold standard” for diagnosing CHD. However, some patients have still experienced adverse cardiovascular events despite the absence of arterial stenosis, and further autopsy results have revealed the presence of a large number of arterial plaques in such patients, so the early diagnosis and intervention of unstable CHD has also gradually attracted attention (8-10). Our study explored the diagnostic value of non-calcified plaque loading in adverse cardiovascular events in patients with unstable CHD. The results showed that non-calcified plaques volume and the non-calcified plaques loading had certain diagnostic value for the recurrence of adverse cardiovascular events within 1 year in patients with unstable CHD (P<0.05). Multivariate logistics regression analysis showed that non-calcified plaques volume >145.58 mm3, carotid intima-media thickness >1.515 mm, the LVEF <56.57%, and hypertension were risk factors for recurrence of adverse cardiovascular events within 1 year in patients with unstable CHD (P<0.05).
The CCTA is a noninvasive imaging method that has emerged in recent years, which accurately and clearly shows the coronary arteries and ventricular wall. The current literatures report that CCTA plays an important role in the diagnosis of coronary atherosclerotic disease (11-13). Myocardial infarction due to coronary plaque shedding is an important cause of adverse cardiovascular events. Coronary plaque loading can be divided into calcified plaque loading and non-calcified plaque loading; calcified plaque is relatively stable and does not detach easily, and non-calcified plaque does detach easily, resulting in adverse cardiovascular events (14-16). In addition, when non-calcified plaque loading increases, it can also lead to coronary artery stenosis, resulting in insufficient myocardial blood supply, which in turn leads to myocardial remodeling, and can eventually lead to adverse cardiovascular events. In addition, the ROC curve analysis of this study showed that the diagnostic value of non-calcified plaque volume and loading for the recurrence of adverse cardiovascular events within 1 year in unstable CHD patients was comparable to that of carotid intima-media thickness, LVEF, hypertension, and so on. The carotid intima-media thickness, LVEF, and hypertension have been confirmed to be good predictors of adverse cardiovascular events (17-20), which indicates that the use of CCTA to measure the volume and loading of non-calcified plaques is of good value in diagnosing adverse cardiovascular events that recur within 1 year in patients with unstable CHD.
In summary, CCTA measurement of coronary non-calcified plaque loading can be used as a predictor for adverse cardiovascular events in patients with unstable CHD.
Limitations
This study had some limitations including that it was a retrospective clinical study and failed to explore the formation mechanism of non-calcified plaque loading. Moreover, the sample size is relatively small.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-933/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-933/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-933/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of 74 Group Military Hospital of PLA Army (No. 2021087). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huang H, Liu J, Liang Y, et al. Prevalence and Mortality of Hypochloremia Among Patients Suffering From Coronary Artery Disease and Congestive Heart Failure: An Analysis of Patients in CIN-I and MIMIC-III Databases. Front Med (Lausanne) 2021;8:769646. [Crossref] [PubMed]
- Bao K, Huang H, Huang G, et al. Platelet-to-hemoglobin ratio as a valuable predictor of long-term all-cause mortality in coronary artery disease patients with congestive heart failure. BMC Cardiovasc Disord 2021;21:618. [Crossref] [PubMed]
- Infante T, Cavaliere C, Punzo B, et al. Radiogenomics and Artificial Intelligence Approaches Applied to Cardiac Computed Tomography Angiography and Cardiac Magnetic Resonance for Precision Medicine in Coronary Heart Disease: A Systematic Review. Circ Cardiovasc Imaging 2021;14:1133-46. [Crossref] [PubMed]
- Patel VI, Roy SK, Budoff MJ. Coronary Computed Tomography Angiography (CCTA) vs Functional Imaging in the Evaluation of Stable Ischemic Heart Disease. J Invasive Cardiol 2021;33:E349-54. [PubMed]
- Xu DP, Xu JP, He ZL, et al. Correlation between Characteristics of Coronary Plaque and Chinese Medicine Syndromes of Coronary Heart Disease: A Cross-Sectional Study Analysed by Intravascular Ultrasound. Chin J Integr Med 2022;28:840-6. [Crossref] [PubMed]
- Li Z, He Y, Wang S, et al. Association between triglyceride glucose index and carotid artery plaque in different glucose metabolic states in patients with coronary heart disease: a RCSCD-TCM study in China. Cardiovasc Diabetol 2022;21:38. [Crossref] [PubMed]
- Gudmundsson EF, Björnsdottir G, Sigurdsson S, et al. Carotid plaque is strongly associated with coronary artery calcium and predicts incident coronary heart disease in a population-based cohort. Atherosclerosis 2022;346:117-23. [Crossref] [PubMed]
- Jiang H, Li L, Chen W, et al. Application of Metabolomics to Identify Potential Biomarkers for the Early Diagnosis of Coronary Heart Disease. Front Physiol 2021;12:775135. [Crossref] [PubMed]
- Adams A, Bojara W, Schunk K. Early Diagnosis and Treatment of Coronary Heart Disease in Asymptomatic Subjects With Advanced Vascular Atherosclerosis of the Carotid Artery (Type III and IV b Findings Using Ultrasound) and Risk Factors. Cardiol Res 2018;9:22-7. [Crossref] [PubMed]
- Adams A, Bojara W, Schunk K. Early Diagnosis and Treatment of Coronary Heart Disease in Symptomatic Subjects With Advanced Vascular Atherosclerosis of the Carotid Artery (Type III and IV b Findings Using Ultrasound). Cardiol Res 2017;8:7-12. [Crossref] [PubMed]
- Andreini D, Modolo R, Katagiri Y, et al. Impact of Fractional Flow Reserve Derived From Coronary Computed Tomography Angiography on Heart Team Treatment Decision-Making in Patients With Multivessel Coronary Artery Disease: Insights From the SYNTAX III REVOLUTION Trial. Circ Cardiovasc Interv 2019;12:e007607. [Crossref] [PubMed]
- Mohammadzadeh A, Farzaneh M, Zahedmehr A, et al. Coronary CT Angiography and Dual-Energy Computed Tomography in Ischemic Heart Disease Suspected Patients. Arch Iran Med 2019;22:376-83. [PubMed]
- Han D, Beecy A, Anchouche K, et al. Risk Reclassification With Coronary Computed Tomography Angiography-Visualized Nonobstructive Coronary Artery Disease According to 2018 American College of Cardiology/American Heart Association Cholesterol Guidelines (from the Coronary Computed Tomography Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry [CONFIRM]). Am J Cardiol 2019;124:1397-405. [Crossref] [PubMed]
- Roberts WC. Quantitative Extent of Atherosclerotic Plaque in the Major Epicardial Coronary Arteries in Patients with Fatal Coronary Heart Disease, in Coronary Endarterectomy Specimens, in Aorta-Coronary Saphenous Venous Conduits, and Means to Prevent the Plaques: A Review after Studying the Coronary Arteries for 50 Years. Am J Cardiol 2018;121:1413-35. [Crossref] [PubMed]
- Zhou H, Wang X, Zhu J, et al. Relation of Carotid Artery Plaque to Coronary Heart Disease and Stroke in Chinese Patients: Does Hyperglycemia Status Matter? Exp Clin Endocrinol Diabetes 2018;126:134-40. [Crossref] [PubMed]
- Held C, White HD, Stewart RAH, et al. Inflammatory Biomarkers Interleukin-6 and C-Reactive Protein and Outcomes in Stable Coronary Heart Disease: Experiences From the STABILITY (Stabilization of Atherosclerotic Plaque by Initiation of Darapladib Therapy) Trial. J Am Heart Assoc 2017;6:005077. [Crossref] [PubMed]
- Qian C, Sun Y, Jiang J. Diagnostic Values of Epicardial Adipose Tissue Thickness with Right Common Carotid Artery Elasticity and Intima-Media Thickness for Middle-Aged and Elderly Patients with Coronary Heart Disease. Int J Gen Med 2021;14:633-9. [Crossref] [PubMed]
- Kang HJ, Kim MH, Sung J, et al. Effect of Probucol and/or Cilostazol on Carotid Intima Media Thickness in Patients with Coronary Heart Disease: A Randomized, Multicenter, Multinational Study. J Atheroscler Thromb 2021;28:124-36. [Crossref] [PubMed]
- Wang MH, Heizhati M, Li NF, et al. Development and Validation of a Prognostic Model to Predict High-Risk Patients for Coronary Heart Disease in Snorers With Uncontrolled Hypertension. Front Cardiovasc Med 2022;9:777946. [Crossref] [PubMed]
- Fu M, Zhou D, Tang S, et al. Left atrial volume index is superior to left atrial diameter index in relation to coronary heart disease in hypertension patients with preserved left ventricular ejection fraction. Clin Exp Hypertens 2020;42:1-7. [Crossref] [PubMed]
(English Language Editor: J. Jones)


