
Lung cancer surgery in Denmark
From primary to tertiary care
The Danish hospital system consists of primary, secondary and tertiary care, as well as private clinics, which can be primary or secondary care. The different cares are structured hierarchically, with more specialised treatment in secondary care and the most specialised treatment in tertiary care.
A thorough examination of the hospital system is outside the scope of this article, but the following is an abridged version: in Denmark, partly due to its small size and moderately dense population of 5.8 million, every citizen can have an assigned general physician (GP) within a reasonable distance from their residence. The GP is the primary care. The GP handles approximately 90% of patient contacts in their clinic without a referral, which alleviates the pressure of the hospital system. Patients referred to the department of thoracic surgery, usually start by reporting symptoms or complaints to their GP, although some are chance findings during computed tomography (CT) scans or other imaging for other pathologies. Before referral, the GP diagnoses further with the help of blood samples, X-rays, lung-functioning tests, CT scans, etc. If the diagnosis is unclear or the GP discovers ailments that require specialised care, they then refer to a specialist in the appropriate area. The specialist, which usually works at a hospital, but can be private, will then order supplementary tests. This is the secondary care.
If the general practitioner suspects lung cancer, they usually start by ordering a CT scan with contrast. The general practitioner must refer the patient if one or more of the following criteria are present: (I) malignancy suspect lung infiltrates or tumour in the mediastinum on diagnostic imaging, (II) biopsy from a metastasis indicating primary lung cancer, (III) clear symptoms of possible lung cancer, such as haemoptysis or shortness of breath for more than a week without any other explanation. These types of criteria exist for a variety of different cancers and other illnesses.
If any of the abovementioned criteria are met the GP must refer the patient to a specific algorithm for lung cancer, which covers investigation, treatment, and follow-up/rehabilitation. Firstly, the patient will be scheduled for an appointment with a pulmonologist at a hospital, the secondary care. At the department of pulmonology, the patient will be referred to a so-called “cancer package” consisting of a CT-scan with contrast, positron emission tomography (PET)-CT, lung function tests [forced expired volume in the first second (FEV1), forced vital capacity (FVC), diffusing capacity of the lungs for carbon monoxide (DLCO)], transbronchial or CT guided biopsy and an endobronchial ultrasound (EBUS) according to European Society of Thoracic Surgeons (ESTS) guidelines (1,2). An overview of the timeline in the specific algorithm for lung cancer is illustrated in Figure 1. Moreover, according to Danish law, the workup for suspected cancer must be started within 14 days (excluding weekends and holidays) after referral to the hospital and the time allowed for this is 28 days. After referral to treatment (surgical or oncological), patients have to be treated within 14 days. This responsibility is imposed on the patients’ municipality. If the municipality is unable to offer workup or treatment within the allotted timeframe, they must refer the patient to another municipality (3). Most patients referred to the department of thoracic surgery are referred from the department of pulmonology, however, some come from other specialities, usually patients with mediastinal tumours, lung metastases, sarcomas, etc.

The pulmonologists present all patients at a multidisciplinary tumour board (MDT) with participation of pulmonologists, thoracic surgeons, oncologists, radiologists, specialists in nuclear medicine and pathologists. Patients’ symptoms, previous medical history including co-morbidities, lung functions tests, PET-CT scans and pathology is presented and discussed to evaluate, whether the patient is a candidate for surgery according to guidelines or oncological treatment (4). Furthermore, the thoracic surgeons attend other special MDTs such as thymic tumours, neuroendocrine tumours, and sarcomas.
Organisation
In Denmark, thoracic surgery is centralised at the four University Hospitals based in Aalborg, Aarhus, Odense, and Copenhagen. These cover different regional areas. They are all departments of Cardiothoracic Surgery, and Danish resident doctors are trained in both subspecialities, however, consultants do only practice one of the subspecialities. The wards are separated in either thoracic or cardiac or can be merged depending on the hospital. The intensive care unit (ICU) and the operations rooms are shared. In most centres, the consultants are further subspecialised in specific areas such as video-assisted thoracoscopic surgery (VATS) lobectomy and segmentectomy, minimal invasive oesophageal resections [VATS or robot-assisted thoracic surgery (RATS)], pectus surgery, traumatology, mesothelioma surgery, mediastinal surgery, and advanced endoscopic procedures. The department at Rigshospitalet covers the largest population of 1.83 million people. Lung transplantation, malignant thymic surgery, mesothelioma surgery and paediatric cardiac surgery is centralised at Rigshospitalet. The departments cooperate closely, share their knowledge and experiences and especially difficult cases can be referred internally within the departments.
The Department of Thoracic Surgery at Rigshospitalet is presented as an example. It consists of a ward with 36 beds. Following surgery patients are admitted to a post-anaesthesia care unit (PACU) recovery unit with four beds next to the ward. Smaller procedures such as VATS cyst resections, pleural biopsies, wedge resections and VATS thymectomies stay 2 hours before referral to the ward. VATS lobectomies, segmentectomies, thoracotomies and oesophageal resections stay overnight. Patients come to the ward 2 days before their surgery and are informed and instructed by the operating surgeon, the anaesthesiologist, a nurse from the ward and receive a thorough examination of their current and previous medical history by trained medical students. They then arrive at 7:00 am the day of their operation, which allow for flexibility in the planning of operations, i.e., a patient is absent, or the operation is cancelled due to external circumstances. Usually, the plan for operations is laid out a week or more in advance. Three operating theatres function from 8:00 am to 3:00 pm daily Monday through Friday and twice per week to 6:00 pm for a total of approximately 40 surgeries per week. The ICU is mainly used for cardiac patients, trauma patients and patients with severe complications after thoracic surgery. The thoracic ICU is staffed with anaesthesiologists and nurses trained in anaesthesiology. The anaesthesiologists are specialised as well for thoracic patients, i.e., treatment of extracorporeal membrane oxygenated (ECMO) patients. This interdisciplinary cooperation allows for optimal care and swift recovery. Pre- and postoperative care is guided by the Enhanced Recovery After Surgery (ERAS) Society guidelines for pulmonary surgery (1) and applied in a translated and matched way to the patient cohort at the Copenhagen Hospital as local guidelines. They guide treatment of pre- and postoperative challenges and exist for doctors as well as nurses and other personnel. Every new employee at the department of thorax surgery is required to familiarise themselves with the contents of the local guidelines. There is a high focus on ensuring early mobilisation of patients and several strategies have been implemented, i.e., urinary catheters are avoided for smaller resections and removed at the earliest possible opportunity. Moreover, to encourage daily walks patients are expected to go to the common dining area in the middle of the ward for meals. They can choose to eat in the dining hall or bring their meal back to their room. Every room has a chair and patients are encouraged to sit in the chair instead of lying in their bed, as well as go for walks around the hospital. Equipment for transporting catheter bags, chest-drain tube collectors and intravenous fluids (IV) fluids/antibiotics are provided, to promote mobilisation. Furthermore, patients are encouraged to frequently use fitness bikes placed in the ward. Patients that are having trouble mobilising, due to either pain, fatigue, or other issues, are assigned a physiotherapist specialised in post-operative care for lung resections, which visits them daily at the ward and provide exercises, such as training regimes in bed and often provide a positive expiratory pressure (PEP) device. Chest drains are removed when airflow is <20 mL/min for more than 12 hours and suction per default is set to −2 cmH2O at Rigshospitalet, as studies have shown earlier air-leak cessation, lower total fluid production and thereby earlier removal and possible lower length of stay (5,6), however, optimal level of suction is still to be determined (7) and default settings vary from −2 to −10 cmH2O between centres in Denmark. Preoperatively patients are encouraged to excise, lose weight, cessation of smoking and alcohol with supports groups and/or nicotine plasters, etc.
Outcomes
Tracking operational data in Denmark is very manageable as all patients sign a consent form before their operation. They thereby give access to their journal, which is digitalised, and its use in research and optimisation of quality. Moreover, all operations are logged in a digital system, Epic [Sundheds Platformen (SP)] or in an Electronic Patient Record (EPJ) and easy to access and extract. Furthermore, every citizen in Denmark is included in the Central Person Register (CPR) and assigned a CPR number. The CPR number consists of ten digits, with the first six digits indicating the date of birth and the last digit the persons’ gender. The CPR number is unique for each citizen, will always belong to that person and a CPR number will never be reused. Basic data is also registered in the CPR system, such as name, address, civil status, birth registration information, citizenship(s), kinship and, in relevant cases, incapacity. The CPR system allows for tracking of patients as well as their basic information and combined with a digitalised medical journal gives immense value to research in Denmark.
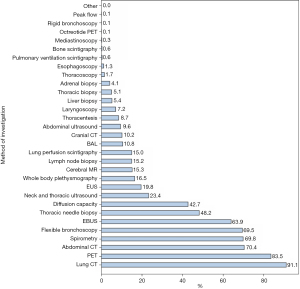
All data from lung cancer patients are reported to the Danish Lung Cancer Registry (DLCR). The total number of reported cases for lung cancer patients in 2020 was 4,817, with 3,912 being non-small cell lung cancer (NSCLC). Thirteen departments of pulmonology and general medical departments managed the work-up. Different methods of work-up were applied (Figure 2). Notably, almost all patients received CT and/or PET and/or bronchoscopy and/or EBUS and/or spirometry. For surgical patients, 98% underwent PET (8).
The resection rate in Denmark 2020 was 27.1%, in total 1,154 resections. The resection rate has increased from 2010 and onwards. The rate of resections varies between geographic regions with Region Sjaelland having the lowest rate of 21.3% and Region Nordjylland having the highest of 34.2%. In 2020, 84.1% were lobectomies, 10.1% wedge resections, 2.9% segmentectomies, 2.3% pneumonectomies and 0.7% exploratory without resection. Fewer exploratory procedures and pneumonectomies are being performed, while more lobectomies and segmentectomies are being performed (Table 1). VATS was the preferred access with 78.5% of lung cancer operations performed like this nationally, but the fraction of VATS varies between centres from 70.9% at Aalborg to 93.5% at Rigshospitalet. Patient length of stay was median 3 days including all four hospitals in Denmark.
Table 1
| Country | Year | Total | Exploratory (%) | Wedge (%) | Segment (%) | Lobectomy (%) | Pneumonectomy (%) |
|---|---|---|---|---|---|---|---|
| Denmark | 2020 | 1,154 | 0.7 | 10.1 | 2.9 | 84.1 | 2.3 |
| 2019 | 1,209 | 1.2 | 11.2 | 2.3 | 83.3 | 2.1 | |
| 2018 | 1,186 | 1.2 | 9.4 | 2.9 | 83.3 | 3.3 | |
| 2017 | 1,083 | 1.3 | 9.0 | 3.1 | 83.4 | 3.1 | |
| 2016 | 1,037 | 1.2 | 11.3 | 1.9 | 82.1 | 3.6 | |
| 2003–2015 | 9,678 | 5.7 | 10.8 | 2.0 | 73.1 | 8.3 |
*, Danish Lung Cancer Register—annual report 2019–2020 (https://www.lungecancer.dk/rapporter/aarsrapporter/).
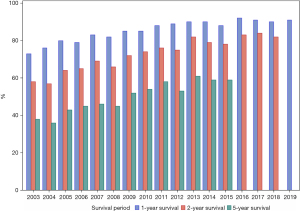
Survival rates for surgical removal of lung cancer have improved over the last 20 years. In 2003 1-year survival was 73%, 2-year survival 58% and 5-year survival 38% compared with 1-year survival rate of 91% from 2019–2020, 2-year survival was 82% from 2018–2020 and 5-year survival was 59% from 2015–2020 (Figure 3).
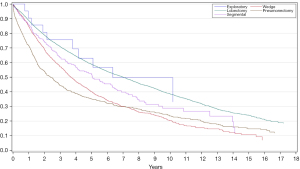
Regarding survival for different modalities of operations from 2003 to 2020, survival rates are superior for patients that have undergone a lobectomy, then in descending order; segmental resections, wedge resections and pneumonectomy for the first 7 years, afterwards pneumonectomy patients’ survivability outperform wedge resections. Importantly, segmental resections are increasing in Denmark, and few of these were performed before 2013. However, segmentectomies are only performed in compromised patients. Examining the recent survival rates lobectomies and segmental resections 1- and 2-year survival rates are similar, however; 5-year survival rates are still superior in the lobectomy group (Figure 4).
In general, according to the DLCR the rate of complications is low, with 72.1% of patients experiencing no complications, 19.3% having one complication and 8.6% having two or more complications. Specifically, during 2020, 0.8% of patients died during hospitalisation, 0.6% required intensive care treatment with a respirator, 1.3% developed empyema, 3.4% required reoperation, 4.5% developed arrhythmias, 9.8% had air leakage and 6.8% suffered from pneumonia.
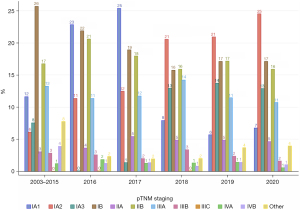
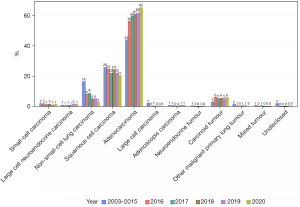
The tumour characteristics can be seen in Figures 5,6. The proportion of adenocarcinomas surgically removed is rising while fewer squamous cell carcinomas and non-small-cell carcinomas are treated surgically.
Discussion/perspectives
The organisation of health care in Denmark, especially the cancer packages allow for quick and consistent diagnosis and treatment. Moreover, the hierarchy of care ensures that only relevant and fully diagnosed patients are being treated at the Departments of Thoracic Surgery, allowing for optimal allocation of resources. Geographically Denmark is a small and highly populated country, and as such GPs are located close to their patients. Moreover, healthcare is free, so no financial barriers exist for the patient concerning examination and treatment. The derived effect of, free health care, organisation, and geography, is early detection of surgical operable conditions and good outcomes for the patient. Specifically, for Denmark, in contrast to other European countries, thoracic surgical treatment is highly centralised at four centres and only performed by board-certified cardiothoracic surgeons possibly adding to positive outcomes.
The total number of operations for lung cancer in Denmark has been on the rise for the last two decades, with the highest number of operated patients in 2019 at 1,209 operations. In 2020 slightly fewer operations were performed, which may be a result of the COVID pandemic. An increasing number of operations in Denmark are performed by VATS, which was introduced in Denmark in 1999 (9). The high VATS rate of 78.5% in 2020 is probably one of the highest national VATS rate in the world. Assuming similar patient cohorts, surgical proficiency and pre- and post-operational care, the short length of hospital stay after lung cancer surgery in Denmark, could partly be explained by the difference in the proportion of VATS being performed, as VATS are associated with shorter hospital stay and fewer complications compared to open surgery (10,11). Concerns regarding a higher cost of VATS compared to open surgery have been raised due to increased operating time and increased use of disposable instruments in VATS, but studies indicate that this cost is offset by fewer complications, faster recovery and lower readmission rates (12). Data indicates, that it might be possible to further shorten the length of hospital stay, as well as decrease infection rates and pain, by omitting chest drains in selected patients that have undergone VATS with wedge resection (13) and lobectomy (14), but further evidence is needed to support this.
Days alive and out of hospital (DAOH) is a new outcome measure and have recently been applied to investigate the effect of implementing the ERAS programme at Rigshospitalet. DAOH integrates overall information of hospitalisation, readmission, and mortality and as such may be important for defining future improvement strategies with the patient in focus. After implementation of ERAS median DAOH after one year postoperatively was 359 days (15).
In general, 1-, 2- and 5-year survival of lung-operated patients have been rising during the last two decades. Although survival rates have stabilised in the past years and patients operated from 2016 to 2019 has had a stable 1-year survival rate at around 90%. This is true as well for patients operated from 2016 to 2018 regarding 2-year survival rate which has stabilised at around 80% and patients operated from 2013 to 2015 regarding 5-year survival which has stabilised at around 60%. That means, following conventional standards, that 5 years after surgery, six out of ten patients are considered cured.
Survival rates are often used as a measurement of successful treatment, and therefore, the abovementioned stagnation could be interpreted as a lack of improvement in the surgical treatment. Another possibility is that these patients are elderly and often suffering from different chronic diseases and have a history of smoking or are active smokers, and as such, it is unreasonable to expect higher survival rates, even though the surgical treatment and rehabilitation are improving. Hopefully, upcoming data will help clarify this.
In general, lung cancer surgery in Denmark is a safe procedure with good survival outcomes and a low risk of in-hospital mortality. Fewer and fewer patients undergo pneumonectomies, and the resection rate is increasing. Most hospital stays are short and complication rates are low. As more operations transition from open to VATS procedures, the national length of hospital stays is expected to shorten further with possible benefits for survival rates and fewer complications.
VATS lobectomy is a technically challenging procedure for thoracic surgeons, and intraoperative complications or damage to blood vessels can have fatal consequences. Practice on synthetic lungs and/or live animals/animal tissue are being used but can be difficult to obtain and requires supervision. In the next coming years, it might be possible to acquire a basic lobectomy competence before operating on patients by using virtual reality simulators with haptic feedback. Haidari et al. (16) showed that a virtual reality simulator can differentiate between novice, intermediate and experienced surgeons for lobectomy of all five lobes regarding blood loss, procedure time and total instrument path length.
An application for a national lung cancer screening program with low-dosage CT has been submitted in 2021 by the Danish Lung Cancer Group. The screening programme has shown to be both feasible (17,18) and reduce mortality (19,20); however, patient selection, cost-effectiveness and further investigation of positive findings are to be defined. A fully implemented screening programme may result in earlier detection of lung cancer, which is suspected to increase the need for segmental resections. This may lead to better overall survival, at least for peripheral NSCLC, compared to lobectomy (21).
Conclusions
Surgery for lung cancer in Denmark is performed with a very high national VATS rate of 78.5% (2020 data). The introduction and continuous use of VATS has resulted in fewer complications and, combined with the implementation of ERAS programme, shorter length of stay, with no detrimental effect on survival. Data from Rigshospitalet on DAOH with 1-year follow-up, showed that patients on average stayed only 6 days in hospital the following year.
The resection rate and survival after surgery have improved continuously since 2010 with a national resection rate in 2020 of 27.1% and a five-year survival of 60% for all stages.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Alan D. L. Sihoe) for the series “Thoracic Surgery Worldwide” published in Journal of Thoracic Disease. The article has undergone external peer review.
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-371/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-371/coif). The series “Thoracic Surgery Worldwide” was commissioned by the editorial office without any funding or sponsorship. TDC has in the last 36 month been on the speaker bureaus for AstraZeneca and Bristol-Myers Squibb and has been in an Advisory Board for Sanofi and AstrZeneca. RHP serves as an unpaid editorial board member of Journal of Thoracic Disease and he reports speaker fee from Medtronic and AMBU and advisory board membership in AstraZeneca, MSD and Roche. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E, et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019;55:91-115. [Crossref] [PubMed]
-
Sundhedsstyrelsen Danish health authority - Bekendtgørelse om maksimale ventetider ved behandling af kræft og visse tilstande ved iskæmiske hjertesygdomme. Available online: https://www.retsinformation.dk/eli/lta/2015/584
-
Dansk Lunge Cancer Gruppe - Fernando HC. Potential advantage of digital drainage systems using a low-suction approach after video-assisted thoracoscopic surgery lobectomy. J Thorac Dis 2019;11:S1923-4. [Crossref] [PubMed]
- Holbek BL, Christensen M, Hansen HJ, et al. The effects of low suction on digital drainage devices after lobectomy using video-assisted thoracoscopic surgery: a randomized controlled trial†. Eur J Cardiothorac Surg 2019;55:673-81. [Crossref] [PubMed]
- Sørensen MF, Holbek BL, Petersen RH, et al. What is the optimal level of suction on digital chest drainage devices following pulmonary lobectomy? Interact Cardiovasc Thorac Surg 2021;32:938-41. [Crossref] [PubMed]
- Rasmussen TR JE, Rasmussen C, Madsen M. National årsrapport 2019-2020. Dansk Lunge Cancer Gruppe/Register. 2021.
- Hansen HJ, Krasnik M, Pedersen JJ. Thoracoscopic lobectomy. The first experiences in Denmark. Ugeskr Laeger 2002;164:1809-13. [PubMed]
- Falcoz PE, Puyraveau M, Thomas PA, et al. Video-assisted thoracoscopic surgery versus open lobectomy for primary non-small-cell lung cancer: a propensity-matched analysis of outcome from the European Society of Thoracic Surgeon database. Eur J Cardiothorac Surg 2016;49:602-9. [Crossref] [PubMed]
- Laursen LØ, Petersen RH, Hansen HJ, et al. Video-assisted thoracoscopic surgery lobectomy for lung cancer is associated with a lower 30-day morbidity compared with lobectomy by thoracotomy. Eur J Cardiothorac Surg 2016;49:870-5. [Crossref] [PubMed]
- Fiorelli A, Forte S, Caronia FP, et al. Is video-assisted thoracoscopic lobectomy associated with higher overall costs compared with open surgery? Results of best evidence topic analysis. Thorac Cancer 2021;12:567-79. [Crossref] [PubMed]
- Holbek BL, Hansen HJ, Kehlet H, et al. Thoracoscopic pulmonary wedge resection without post-operative chest drain: an observational study. Gen Thorac Cardiovasc Surg 2016;64:612-7. [Crossref] [PubMed]
- Huang L, Kehlet H, Holbek BL, et al. Efficacy and safety of omitting chest drains after video-assisted thoracoscopic surgery: a systematic review and meta-analysis. J Thorac Dis 2021;13:1130-42. [Crossref] [PubMed]
- Huang L, Frandsen MN, Kehlet H, et al. Days alive and out of hospital after enhanced recovery video-assisted thoracoscopic surgery lobectomy. Eur J Cardiothorac Surg 2022;62:ezac148. [Crossref] [PubMed]
- Haidari TA, Bjerrum F, Hansen HJ, et al. Simulation-based VATS resection of the five lung lobes: a technical skills test. Surg Endosc 2022;36:1234-42. [Crossref] [PubMed]
- Pedersen JH, Rzyman W, Veronesi G, et al. Recommendations from the European Society of Thoracic Surgeons (ESTS) regarding computed tomography screening for lung cancer in Europe. Eur J Cardiothorac Surg 2017;51:411-20. [Crossref] [PubMed]
- Pedersen JH, Sørensen JB, Saghir Z, et al. Implementation of lung cancer CT screening in the Nordic countries. Acta Oncol 2017;56:1249-57. [Crossref] [PubMed]
- National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N Engl J Med 2020;382:503-13. [Crossref] [PubMed]
- Suzuki K, Saji H, Aokage K, et al. Comparison of pulmonary segmentectomy and lobectomy: Safety results of a randomized trial. J Thorac Cardiovasc Surg 2019;158:895-907. [Crossref] [PubMed]


