Bilateral chylothorax after transsternal total thymectomy: resolution with short period of fasting and total parenteral nutrition
Introduction
Postoperative chylothorax can occur in almost all cases of thoracic surgery and are caused mostly by thoracic duct injury following esophagectomy, ligation of patent ductus arteriosus, aorta surgery, or pneumonectomy. It causes respiratory and metabolic problems and was reported that approximately 25−50% of patients require surgical treatment with mortality of 21% (1). We report of postoperative bilateral chylothorax after transsternal total thymectomy which was treated by one week of fasting with total parenteral nutrition without octreotide injection.
Case presentation
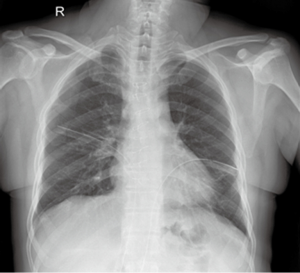
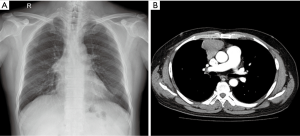
A 50-year-old man who had hypertension, diabetes and chronic kidney disease was referred to our hospital for surgical treatment of anterior mediastinal mass. He did not have chest pain, dyspnea, or myasthenic symptoms though right hilar bulging was noted on the chest X-ray as a routine checkup. Chest computed tomography (CT) showed solid mass anterior to superior vena cava and pericardium with its largest diameter of 7 cm (Figure 1). We decided to remove entire thymic tissue including mass and mediastinal fat.
Under general anesthesia, he underwent total thymectomy via median sternotomy. All fat tissue within the area margined by bilateral phrenic nerves, innominate vein, and diaphragm was removed with concerns of ectopic thymic tissue. Two chest tubes were inserted into bilateral pleural cavity via mediastinum. The procedures were uneventful and there was no visible chylous leak during operation.
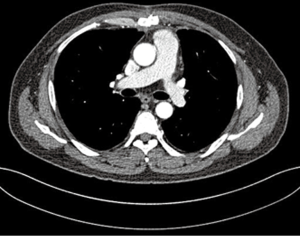
On the postoperative day 2, bilateral pleural drainage was changed from serous clear fluid to milky and turbid fluid with its amount of 470 mL for a day (Figure 2). The biochemical analysis of pleural fluid revealed that triglyceride was 1,226 mg/dL and we confirmed chylothorax. We started fasting, total parenteral nutrition, and maintenance of bilateral pleural drainage. He responded to such conservative management so quickly that fluid via chest tubes returned to be clear with its amount of less than 150 mL for a day. After a week of fasting, we resumed the normal residual diet and pleural fluid changed to milky again on the next day. Although the character of pleural drainage was chylous, we started low fat diet instead of fasting because daily amount of drainage was less than 150 mL. During the three days of low fat diet, pleural drainage was still milky but its amount decreased gradually to 90 mL for a day, we changed normal diet and chest tube was removed on the next day. He was discharged on the postoperative 16 day. Three months after operation, chest CT showed no remarkable findings or residual pleural effusion (Figure 3).
Discussion
Chylothorax results from tear or rupture of thoracic duct or its branches and can occur after various kinds of thoracic surgery. The incidence of postoperative chylothorax is reported to range from 0.5% to 2.2% and more common in esophagectomy or posterior mediastinal operation than pulmonary resection (2). Bilateral chylothorax is rare complication after thymectomy via median sternotomy and Huang et al. reported that 3 out of 217 patients (1.38%) who underwent extended thymectomy due to myasthenia gravis had postoperative chylothorax (3).
There are two groups of lymphatic drainage system in the anterior compartment of mediastinum; one is sternal group and the other is anterior mediastinal (prevascular) group. The latter lies anterior and lateral to the thymus as well as just anterior to the great vessels. The prevascular lymph nodes drain the anterior portion of pericardium, anterior part of heart, thymus, thyroid, diaphragm, and anterior portion of mediastinal pleura (4). Postoperative chylothorax after thymectomy via sternotomy can be caused by disruption of above mentioned small mediastinal lymphatic channels. Such mediastinal lymphatics, remote from thoracic duct, are minor that they are unseen during the operation even they are disrupted during operative procedures (5).
Because chylothorax was confirmed on the second postoperative day and two pleural chest tubes were in situ, initial management was conservative including fasting and total parenteral nutrition. Octreotide was reported that it is effective for the treatment of chylothorax by decreasing volume and promoting absorption of thoracic duct (5). However, we were very cautious to use octreotide because its complications such as abrupt hyperglycemia or hypoglycemia were expected to affect adversely to the control of patient’s diabetes.
One of the most important factor for choosing the treatment option or time (conservative or operation) is considered to be amount of pleural drainage. Although two weeks of fasting is known to be required for treating chylothorax usually, we decided to break fasting after one weak because initial drainage of chylothorax was small when we consider the amount of normal daily flow through thoracic duct. Even when he showed turbid milky pleural drainage again after staring normal diet, daily drainage was less than 150 mL. Normal diet changed to low fat diet instead of fasting and pleural drainage decreased gradually even after normal diet was re-maintained. This was possible because chylothorax followed by surgery of anterior mediastinum may be caused not by thoracic duct injury but by minor lymphatic channel injury.
If the patients who underwent transsternal thymectomy have dyspnea or bilateral pleural effusion on chest X-ray, chylothorax should be considered as a cause although it rarely occurs after thymectomy. Although treatment options are various from conservative to operation (thoracic duct ligation, pleurodesis, or pleurectomy), initial conservative management is usually successful if they do not have massive chylous leak.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Sieczka EM, Harvey JC. Early thoracic duct ligation for postoperative chylothorax. J Surg Oncol 1996;61:56-60. [Crossref] [PubMed]
- Nakano A, Kato M, Watanabe T, et al. OK-432 chemical pleurodesis for the treatment of persistent chylothorax. Hepatogastroenterology 1994;41:568-70. [PubMed]
- Huang CS, Hsu HS, Kao KP, et al. Chylothorax following extended thymectomy for myasthenia gravis. Thorac Cardiovasc Surg 2007;55:274-6. [Crossref] [PubMed]
- Fraser RG, Pare JAP. Diagnosis of disease of the chest. 2nd. Philadelphia: Saunders, 1978.
- Mafé JJ, Caravajal JM, Baschwitz B, et al. Bilateral chylothorax after thymectomy via median sternotomy and resolution through conservative treatment. Eur J Cardiothorac Surg 2003;24:466-8. [Crossref] [PubMed]