Prevalence of hypertension and noise-induced hearing loss in Chinese coal miners
Introduction
Environmental noise endangers human health by damaging the extra-auditory system as well as the auditory system (1). Observational and experimental studies suggested that noise can increase annoyance levels (2,3), undermine sleep quality and cause daytime drowsiness (4), worsen patient outcomes and staff performance in hospitals (5), and impair cognitive performance in school children (6,7). It may induce these physiological and psychosocial responses, and ultimately extra-auditory system disorders, by stimulating the hypothalamus-pituitary-endocrine system and by altering blood dynamics and hormone levels (8).
Although some studies linked occupational noise exposure to hypertension (9-12), the epidemiologic evidence was not consistent (13,14). Owing to dominant confounding factors such as lifestyle and genetic predisposition, it is difficult to accurately assess the contribution of occupational noise to hypertension.
Long-term and high-intensity noise directly impacted hearing and caused noise induced hearing loss (NIHL) (15). NIHL was characterized by high-frequency hearing loss followed by gradual loss of low-frequency (16). NIHL is permanent irreversible damage and there are no effective treatments currently.
The present study was aimed to assess whether Chinese coal miners are at risk of developing hypertension and NIHL, and whether occupational noise exposure was a risk factor for hypertension.
Materials and methods
Participants
Datun Coal Power Company in China has four coal preparation plants, a coal-fired power plant, a coal thermal power plant, an electrolytic aluminium plant, and also has a mechanical repair, construction and installation, motor transport and logistics service units.
In order to establish whether Chinese coal miners were at risk of developing hypertension and NIHL, and whether occupational noise exposure was a risk factor of hypertension, we recruited 738 volunteers from the company for this study, according to the inclusion criteria that one should be a Han Chinese with over 10-year career, and be free from the medication history of anti-hypertensive or ototoxic drugs (e.g., aminoglycosides, macrolide antibiotics), previous ear infections, severe head trauma, electrocardiogram abnormalities, having been worked in shifts or at night, exposure to explosive noise and use of PPE. This cross-sectional study was designed and approved by the Institute of Occupational Disease Prevention, Jiangsu Provincial Center for Disease Prevention and Control. The 738 volunteers were divided into two groups according to the levels of occupational noise. Volunteers who experienced occupational noise ≥5 dB (A) were included into the noise-exposed group, while those who experienced occupational noise <85 dB (A) were included into the control group. The noise-exposed group was composed of 360 volunteers who engaged in the noise-generating activities such as wood sawing, forging, and casting. The control group was composed of 378 volunteers including managers, transport drivers, and maintenance workers. The study was conducted in accordance with the Helsinki Declaration and approved by the local ethics committees.
Questionnaires
A questionnaire was used to obtain personal information such as age, sex, length of service, lifestyle (smoking and drinking), exposure to explosive noise, use of personal protective equipment (PPE), past and previous health status, family history of cardiovascular diseases (CVD), and use of ototoxic drugs. Smoking was defined as more than one cigarette per day for the last six months; drinking was defined as more than one alcoholic beverage per week for the last six months. Use of PPE was based on the percentage of time that the subjects wore PPE and the type of PPE (e.g., earplugs and earmuffs). All the subjects filled out the questionnaire after giving informed consent and before a physical examination.
Clinical measurements
All the subjects were required to fast for 10 h before the medical examination to ensure the accuracy of blood glucose and lipid indicators. And the subjects should were required to rest for at least 15 min and refrained from smoking for at least 15 min before blood pressure measurement. Blood pressure was measured by a trained nurse using a mercury sphygmomanometer on the left arm of a patient seated. The cuff-size is 12–14 cm. Three measurements were made and the mean value was used. Each measurement had an interval of 5 min, and all measurements were taken between 8 and 10 AM. Subjects were classified as hypertensive if the systolic blood pressure (SBP) was ≥140 mm Hg or the diastolic blood pressure (DBP) was ≥90 mm Hg according to the World Health Organization (WHO) 2007 classification. Systolic hypertension is defined as SBP ≥140 mm Hg, and diastolic hypertension is defined as DBP ≥90 mm Hg. Height (m) and weight (kg) were measured by using an automatic measuring instrument, and body mass index (BMI) was calculated as weight (kg)/height2 (m2). Total cholesterol (TC), triglyceride (TG), high-density lipoprotein (HDL), low-density lipoprotein (LDL) levels were measured biochemically in blood samples.
Pure tone audiometry and environmental noise evaluation
An otolaryngologist inspected the ears of all the subjects. All the subjects had undergone pure tone audiometry tests in a sound-attenuating chamber with a background noise level <25 dB (A). Both ears were tested by using ascending pure tones at frequencies of 0.5, 1, 2, 3, 4, and 6 kHz. The subjects were required to avoid a noisy environment over 12 h before test. Trials were repeated at least 3 times to determine the lowest signal intensity, which served as the final threshold value for each ear. The mean threshold values at 0.5, 1, and 2 kHz were used to determine low-frequency hearing status, while the mean threshold values at 3, 4, and 6 kHz were used to determine high-frequency hearing status. A notch of NIHL was showed around 3 to 6 kHz, and threshold values at high-frequency were substantially worse than threshold values at low-frequency. Audiometric deficit or hearing loss was defined as a hearing threshold >25 dB at high frequency or at both high and low frequencies. The diagnostic criteria of occupational NIHL were based on the Chinese occupational health standard (GBZ49-2002, http://www.zybw.net). On a certain test frequency, normal hearing was defined as binaural hearing level ≤25 dB, unilateral hearing loss was defined as monaural hearing is >25 dB, and bilateral hearing loss was defined as binaural hearing level >25 dB.
Workplace noise was measured by using a sound pressure noise meter (Noise-Pro, Quest, Oconomowoc, WI) at 10 am, 3 pm, and 5 pm for three consecutive days, twice per year and evaluated, according to China national criteria for noise in the workplace (GBZ43-2002, http://www.zybw.net). To determine the actual noise levels, the equivalent continuous a-weighted sound pressure was normalized to a nominal eight-hour per day (LEX, 8h). A sound pressure noise meter was chosen to measure the occupational noise levels of fixed position. An individual noise dosimeter was used for the levels of flow positions measurement. The eight-hour continuous equivalent sound levels (LEX, 8h) of each jobs was calculated by the following formula.
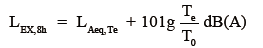
here Te represents the actual working time of one working day, LAeq, Te represents the equivalent sound level of the actual working day, and T0 represents the eight-hour standard working time.
Statistical analyses
Continuous data were shown as mean ± standard deviation and were analyzed by using independent-sample, two-sided t-tests. Categorical data were analyzed by using two-sided chi-square tests. Binary logistic regression was used to assess the association between occupational noise level and hypertension by computing odds ratios (ORs) and 95% confidence intervals (CIs) while controlling for potential confounding factors. Multivariate logistic regression was used to assess the association between occupational noise level and hearing loss by computing age-adjusted OR and 95% CIs. Differences would be considered significant if the P value was <0.05. All the analyses were carried out by using SPSS 13.0 software.
Results
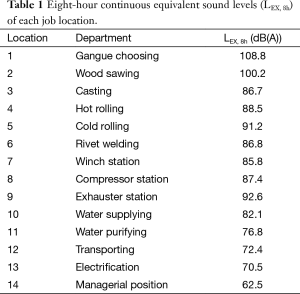
According to the different departments, all the subjects in this study were exposed to noise levels from 60 to 110 dB of eight-hour continuous equivalent sound (LEX, 8h). Table 1 indicated the measurements of the LEX, 8h in 14 different locations.
Full table
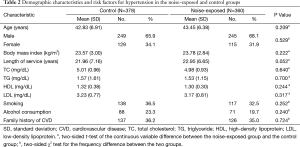
The demographic characteristics and potential risk factors associated with high blood pressure in noise-exposed and control groups are shown in Table 2. There were no significant differences in age, sex, body mass index, length of service, total cholesterol level (TC), triglyceride level (TG), high-density lipoprotein (HDL), low-density lipoprotein (LDL), smoking, alcohol consumption, or family history of CVD between the groups (P>0.050).
Full table
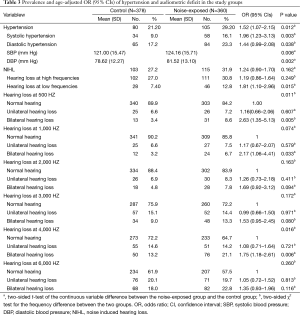
Table 3 shows the percentages of subjects with hypertension, systolic hypertension and diastolic hypertension were significantly higher in noise-exposed group than control group: hypertension, 29.2% vs. 21.2% (P=0.012); systolic hypertension, 16.1% vs. 9.0% (P=0.003); and systolic hypertension, 23.3% vs. 17.2% (P=0.038). Taking the control group as reference, we found that the noise-exposed group had the increased risk of hypertension (age-adjusted OR =1.52, 95% CI =1.07–2.15) and systolic hypertension (age-adjusted OR =1.96, 95% CI =1.23–3.13). The mean values of SBP and DBP of the noise-exposed groups were significantly higher than the control group (P=0.006 and P=0.002 respectively).
Full table
Hearing loss at low frequencies was significantly more prevalent in noise-exposed group than control group: 12.8% vs. 7.4% (P=0.015); bilateral hearing loss at 500 Hz: 8.6% vs. 3.4% (P=0.005); bilateral hearing loss at 1,000 Hz: 6.7% vs. 3.2% (P=0.033), bilateral hearing loss at 4,000 Hz: 21.1% vs. 13.2% (P=0.006). We found that the noise-exposed group had the increased risk of hearing loss at low frequencies (age-adjusted OR =1.81, 95% CI =1.10–2.96), bilateral hearing loss at 500 Hz (age-adjusted OR =2.63, 95% CI =1.35–5.13), bilateral hearing loss at 1,000 Hz (age-adjusted OR =2.17, 95% CI =1.06–4.41), and bilateral hearing loss at 4,000 Hz (age-adjusted OR =1.75, 95% CI =1.18–2.61) when we took the control group as reference.
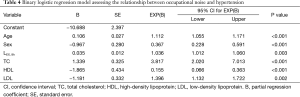
Table 4 shows a binary regression model was established for a more accurate assessment for the relation between noise-exposed intensity and hypertension. This model included several potential risk factors for hypertension: age, LEX, 8h, NIHL, sex, BMI, length of service, TC, TG, HDL, LDL, education level, smoking, alcohol consumption, and family history of CVD. Applying the backward method and removing variables according to the condition of the likelihood ratio test result, six factors entered into the regression model. We found that such factors were significantly correlated with high blood pressure as following: age (OR =1.112, 95% CI =1.055–1.171), sex (OR =0.367, 95% CI =0.228–0.591), LEX, 8h (OR =1.036, 95% CI =1.012–1.060), TC (OR =3.817, 95% CI =2.020–7.013), HDL (OR =0.155, 95% CI =0.066–0.363), LDL (OR =1.396, 95% CI =1.132–1.722).
Full table
Discussion
In this cross-sectional study, we found the relationship between occupational noise exposure and high blood pressure as well as hearing loss, despite the similarity of confounding factors.
Overall, hypertension, systolic hypertension and diastolic hypertension were more prevalent in noise-exposed group than control group. SBP and DBP levels could increase in response to the exposure to high noise levels. These findings implied that occupational noise increased the prevalence blood pressure owing to its influence on both the SBP and the DBP. This result was consistent to the previous studies (10,17,18). In our study, occupational noise exposed group had the higher risk of hypertension compare to the control group (age-adjusted OR =1.52, 95% CI =1.07–2.15).
The mechanism of noise-induced hypertension was not yet clear. However, it can be assumed that noise, as an environmental stressor, signals the activation of the automatic nervous and endocrine systems and the consequent release of stress hormones such as catecholamines (19). When released, catecholamines enhance myocardial contractility and increase blood pressure, and cardiac output via modulation of β-1 receptors (20).
In order to exclude the influence of the confounding factors on the relation of noise levels and hypertension, we also established a regression model to adjust the confounding risk factors for further test. The model included six variables: age, sex, TC, HDL, LDL and LEX, 8h. The results showed that the older and male were more likely to develop high blood pressure than younger and female. The higher levels of TC, LDL and the lower level of HDL were also the risk factors for hypertension. Noise-exposed level was still an independent risk factor for hypertension after controlling the potential confounding factors, which was consistent with the report by Tomei et al. (21).
Long-term, high-intensity noise exposure negatively impacted hearing, and caused both high and low frequency hearing loss (22,23). The noise deteriorated hearing in high tones primarily. Of the systems in the body, the auditory system was the most sensitive part to external noise (24). And we found that the exposure to occupational noise could increase the risk of hearing loss, this is indicated that subjects who had long occupational noise exposure were more likely to suffer from hearing loss.
Our study showed that confounding factors had relations to hypertension and established a tentative connection between occupational noise and hypertension. However, as it was cross-sectional, it could not explain this effect. Based on the results of the present study, we would perform a prospective cohort study in the future to determine how the occupational noise to promote hypertension. Other factors will also be considered in future study, such as environment noise, noise annoyance, the salt intake in diet factors and the exercise frequency in lifestyle risk factors. Finally, selection bias may exist in this survey as a result of the healthy worker effect. The average length of service was up to about 20 years in both groups. The exposed workers had habituated to the environment with high occupational noise intensity, while the workers who were sensitive to noise had been away from their noisy posts.
In conclusion, we found that the occupational noise had an effect on the hypertension and hearing loss of Chinese coal miners. And the occupational noise was an independent risk factor for hypertension and could increase the values of SBP and DBP.
Acknowledgements
The authors thank all of the participants.
Funding: This work was supported by Jiangsu Province’s Outstanding Medical Academic Leader program (LJ201130), Projects of Jiangsu Society Development (BS2005661), and was partly supported by the Preventive Medicine Research Projects of Jiangsu Provincial Commission (Y2013008), Kunshan Municipal Society Development (KS1354) and the National Natural Science Foundation of China (nsfc61175069).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Basner M, Babisch W, Davis A, et al. Auditory and non-auditory effects of noise on health. Lancet 2014;383:1325-32. [Crossref] [PubMed]
- Héritier H, Vienneau D, Frei P, et al. The association between road traffic noise exposure, annoyance and health-related quality of life (HRQOL). Int J Environ Res Public Health 2014;11:12652-67. [Crossref] [PubMed]
- Okokon EO, Turunen AW, Ung-Lanki S, et al. Road-traffic noise: annoyance, risk perception, and noise sensitivity in the Finnish adult population. Int J Environ Res Public Health 2015;12:5712-34. [Crossref] [PubMed]
- Holt JB, Zhang X, Sizov N, et al. Airport noise and self-reported sleep insufficiency, United States, 2008 and 2009. Prev Chronic Dis 2015;12:E49. [Crossref] [PubMed]
- Trickey AW, Arnold CC, Parmar A, et al. Sound levels, staff perceptions, and patient outcomes during renovation near the neonatal intensive care unit. HERD 2012;5:76-87. [Crossref] [PubMed]
- Stansfeld SA, Berglund B, Clark C, et al. Aircraft and road traffic noise and children's cognition and health: a cross-national study. Lancet 2005;365:1942-9. [Crossref] [PubMed]
- Clark C, Crombie R, Head J, et al. Does traffic-related air pollution explain associations of aircraft and road traffic noise exposure on children's health and cognition? A secondary analysis of the United Kingdom sample from the RANCH project. Am J Epidemiol 2012;176:327-37. [Crossref] [PubMed]
- Chang TY, Liu CS, Huang KH, et al. High-frequency hearing loss, occupational noise exposure and hypertension: a cross-sectional study in male workers. Environ Health 2011;10:35. [Crossref] [PubMed]
- Stokholm ZA, Bonde JP, Christensen KL, et al. Occupational noise exposure and the risk of hypertension. Epidemiology 2013;24:135-42. [Crossref] [PubMed]
- Sancini A, Caciari T, Rosati MV, et al. Can noise cause high blood pressure? Occupational risk in paper industry. Clin Ter 2014;165:e304-11. [PubMed]
- Sbihi H, Davies HW, Demers PA. Hypertension in noise-exposed sawmill workers: a cohort study. Occup Environ Med 2008;65:643-6. [Crossref] [PubMed]
- Lee JH, Kang W, Yaang SR, et al. Cohort study for the effect of chronic noise exposure on blood pressure among male workers in Busan, Korea. Am J Ind Med 2009;52:509-17. [Crossref] [PubMed]
- Inoue M, Laskar MS, Harada N. Cross-sectional study on occupational noise and hypertension in the workplace. Arch Environ Occup Health 2005;60:106-10. [Crossref] [PubMed]
- Rapisarda V, Ledda C, Ferrante M, et al. Blood pressure and occupational exposure to noise and lead (Pb): A cross-sectional study. Toxicol Ind Health 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Singh LP, Bhardwaj A, Deepak KK. Occupational noise-induced hearing loss in Indian steel industry workers: an exploratory study. Hum Factors 2013;55:411-24. [Crossref] [PubMed]
- Henderson E, Testa MA, Hartnick C. Prevalence of noise-induced hearing-threshold shifts and hearing loss among US youths. Pediatrics 2011;127:e39-46. [Crossref] [PubMed]
- Huang D, Song X, Cui Q, et al. Is there an association between aircraft noise exposure and the incidence of hypertension? A meta-analysis of 16784 participants. Noise Health 2015;17:93-7. [Crossref] [PubMed]
- Chang TY, Hwang BF, Liu CS, et al. Occupational noise exposure and incident hypertension in men: a prospective cohort study. Am J Epidemiol 2013;177:818-25. [Crossref] [PubMed]
- Spreng M. Possible health effects of noise induced cortisol increase. Noise Health 2000;2:59-64. [PubMed]
- Münzel T, Gori T, Babisch W, et al. Cardiovascular effects of environmental noise exposure. Eur Heart J 2014;35:829-36. [Crossref] [PubMed]
- Tomei G, Sancini A, Tomei F, et al. Prevalence of systemic arterial hypertension, electrocardiogram abnormalities, and noise-induced hearing loss in agricultural workers. Arch Environ Occup Health 2013;68:196-203. [Crossref] [PubMed]
- Lie A, Skogstad M, Johannessen HA, et al. Occupational noise exposure and hearing: a systematic review. Int Arch Occup Environ Health 2016;89:351-72. [Crossref] [PubMed]
- Gomes J, Lloyd O, Norman N. The health of the workers in a rapidly developing country: effects of occupational exposure to noise and heat. Occup Med (Lond) 2002;52:121-8. [Crossref] [PubMed]
- Duarte AS, Ng RT, de Carvalho GM, et al. High levels of sound pressure: acoustic reflex thresholds and auditory complaints of workers with noise exposure. Braz J Otorhinolaryngol 2015;81:374-83. [Crossref] [PubMed]


