Thymectomy via a subxiphoid approach: single-port and robot-assisted
Introduction
To treat myasthenia gravis and anterior mediastinal tumors, thymectomy is conventionally performed via a median sternotomy; however, many less invasive surgical procedures are now possible. These include video-assisted thoracoscopic thymectomy (VATS) (1,2) via a lateral thoracic approach, transcervical thymectomy (3) via a cervical incision, and a subxiphoid approach (4). Currently, most hospitals that perform endoscopic thymectomy use a lateral thoracic approach to perform thoracoscopic thymectomy, even for robot-assisted surgery (5). However, the lateral thoracic approach makes it difficult to identify the contralateral phrenic nerve, and securing a visual field in the neck is challenging. We have previously reported on single-port thymectomy (SPT), which involves performing thymectomy via a single subxiphoid incision, and dual-port thymectomy (DPT), which is similar to SPT but involves the addition of a port in the right parasternal intercostal space to improve the surgery. Furthermore, we have reported on trans-subxiphoid robotic thymectomy (TRT), which is performed using the da Vinci surgical system (Intuitive Surgical, Sunnyvale, CA, USA) (6-9). The subxiphoid approach is an endoscopic surgical procedure to resect the thymus from below the xiphoid process. Moreover, because the camera can be inserted into the midline of the body, as opposed to the lateral thoracic approach, it is easier to identify the bilateral phrenic nerves and to secure a good visual field in the neck. The purpose of this paper was to explore the initial findings of our experiences in performing thymectomy with subxiphoid approaches and to discuss the indications for each approach.
Material and methods
Surgical technique
Single-port thymectomy (SPT)
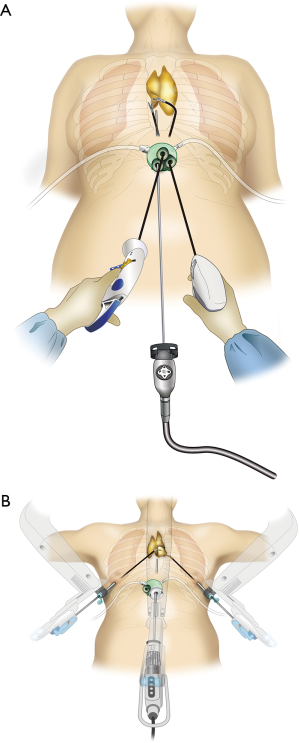
The patient was placed in the supine position with the legs apart. In most cases, differential pulmonary ventilation was not required. The surgeon stood between the patient’s legs, while the endoscopist stood on the right side of the patient and operated the camera. First, a 3-cm long horizontal incision was made that was 1 cm caudal to the xiphoid process. The attachment of the rectus abdominis muscle was dissected away from the xiphoid process, thereby exposing it. The posterior surface of the sternum was blindly dissected using a finger. A vertical incision that was approximately 1 cm in length was made in the rectus abdominis muscle fascia, and a space was created to enable port insertion in the posterior surface of the fascia. Ports that are employed for single-port access surgery, namely a SILS port (Covidien, Mansfield, MA, USA), an X-gate (Akita Sumitomo Bakelite Co., Akita, Japan), or a GelPOINT Mini (Applied Medical, Rancho Santa Margarita, CA, USA), were used. Three child ports were inserted into the main port that was used for single-port access surgery. In the cases using the SILS port and X-gate, three 5-mm port entrances were inserted into the single aperture surgical port, and in the case of the GelPOINT Mini, three 10-mm port entrances were inserted into the single aperture port. One of the entrances was used for the insertion of the camera. One of the child ports was used to insert the camera scope, which was a 30° oblique-view, 5-mm-rigid camera scope. CO2 insufflation was performed at 8 mmHg. The positive pressure, which was caused by CO2 insufflation, aided the dissection of the thymus from the posterior surface of the sternum and extended the space for the surgical field. In most of the subjects, the bilateral mediastinal pleural membranes and both the thoracic cavities were opened. In thymoma cases with suspected infiltration of a unilateral thoracic cavity, the contralateral thoracic cavity was not opened. Anatomically, the two upper poles of the thymus are connected to the thyroid gland; therefore, both upper poles positioned cephalad to the innominate vein need to be separated from the thyroid gland, trachea, and brachiocephalic artery. This requires opening a surgical field in the cervical region to obtain an optimal view. We passed a 2-mm Kirschner wire beneath the presternal skin, which enlarged the posterior surface of the sternum when elevated, to secure a visual field in the neck, particularly the space in the neck. However, even when the wire was not passed, it was found that using CO2 insufflation alone dorsally displaced the mediastinum and heart, and resulted in a sufficiently favorable visual field in the neck. Therefore, this wire technique was not used from the tenth case onward. An Autonomy grasper (Cambridge Endo, Framingham, MA, USA) was operated with the surgeon’s left hand, while a LigaSure™-V or Maryland LigaSure™ (Covidien) was operated with the right hand, and the thymus and thymoma were dissected away from the pericardium (Figure 1A). The resected thymus was inserted into a bag inside the mediastinum and extracted en masse via the subxiphoid incision.
Trans-subxiphoid robotic thymectomy (TRT)
Similar to the SPT technique, a 3-cm horizontal incision was created that was 1-cm inferior to the xiphoid process. A port for single-port access surgery was inserted and CO2 insufflation was performed at 8 mmHg. The thymus was dissected away from the posterior surface of the sternum. Furthermore, the mediastinal pleura were cut bilaterally and both the thoracic cavities were opened. Two 1-cm skin incisions were made on either side in the parasternal sixth intercostal space along the anterior axillary line, and a port that was used for da Vinci robotic surgery was inserted. The da Vinci surgical system (Intuitive Surgical) was then docked from the cranial side. A port for the 12-mm camera was inserted into the subxiphoid single-port access surgery port and attached to the da Vinci camera scope. The da Vinci arms were then attached to the two ports, which were parasternal placed in the sixth intercostal space along the anterior axillary line (Figure 1B). A monopolar spatula or bipolar Maryland forceps, was attached to the right-arm of the da Vinci robot, and either bipolar fenestrated grasping forceps or Cadiere forceps was attached to the left arm. At times to expand the surgical field, the assistant used Autonomy Grasper 45-cm forceps (Cambridge Endo), which is used for single-port surgery. The thymic vein was cut using an EndoWrist Vessel Sealer (Intuitive Surgical).
When treating myasthenia gravis, an extended thymectomy is performed. This involves resecting all the adipose tissues anterior to the phrenic nerve. When treating anterior mediastinal tumors that are unrelated to the myasthenia gravis, a thymectomy is performed with the complete resection of the thymus together with the mass.
The subjects included 80 patients who underwent thymectomy via a subxiphoid approach, performed by two surgeons (T.S. and S.T.). The patients were selected from among 99 surgical cases of myasthenia gravis or anterior mediastinal tumors at Fujita Health University Hospital between March 2011 and November 2015.
The surgical indications for SPT were cases that were preoperatively diagnosed as not having phrenic nerve, pericardial, or vascular infiltration. If a partial lobectomy could be performed, tumor infiltration of the lungs was an indication for SPT. In cases with suspected vascular infiltration, a median sternotomy was indicated; however, TRT was performed in one case with suspected infiltration of the left brachiocephalic vein. In Japan, robot-assisted surgery for lung cancer or anterior mediastinal tumors is not covered under national health insurance; therefore, the patients must bear the surgery cost. Among the cases where there was a possible infiltration of the phrenic nerve, pericardium, or blood vessels by anterior mediastinal tumor, TRT was indicated in patients who requested it after they agreed to bear the treatment cost.
The patients were divided into SPT (n=72) and TRT groups (n=8). A comparative investigation of the following factors between the groups was performed: operative time, blood loss volume, postoperative hospital stay duration, and period of postoperative oral analgesic use. The background characteristics of the patients in each group are shown in Table 1. There was a significant difference in the percentage of thymomas between the two groups (P=0.0003). One case in the SPT group had a tumor that was adherent to right upper lobe; therefore, we performed a simultaneous partial lung resection. Four cases in SPT group were converted to DPT after encountering difficulties with the surgery because of excessive adipose tissue, pectus excavatum, risk of bleeding from a thymic hemangioma, and an iatrogenic pericardial incision. On the day after surgery, all cases were orally administered loxoprofen (60 mg three times daily), which was continued according to the patient’s wishes. In both groups, intramuscular injections of pentazocine at a dose of 15 mg or sodium diclofenac suppositories at a dose of 50 mg were administered on the day of surgery and the day after surgery, according to the patient’s wishes. However, from postoperative day 2, none of the patients received intramuscular pentazocine or sodium diclofenac suppositories. There were no cases with a positive tumor margin. One case in the TRT group was postoperatively diagnosed with thymic carcinoma and underwent postoperative radiotherapy.
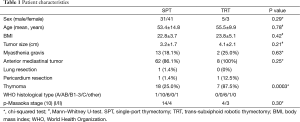
Full table
This study was approved by the ethics committee at the Fujita Health University.
Statistical analysis
The data are expressed as mean ± standard deviation. Comparative analyses were performed using the Chi-squared test for the 0-1 data, and the Mann–Whitney U-test for the ordinal and continuous data. In all of the analyses, statistical significance was set at a P value of <0.05. The Statview version 5.0 software package (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses.
Results
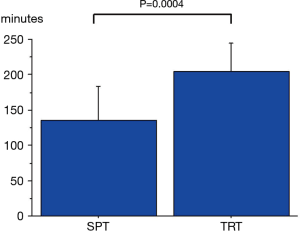
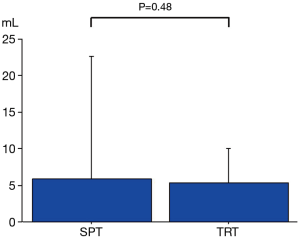
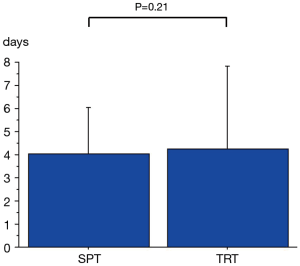
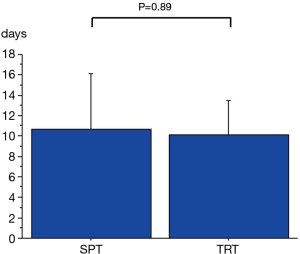
The operative time was shorter in the SPT group compared with that in the TRT group (135±48 and 204±40 min, respectively; P=0.0004; Figure 2). There were no significant differences between the groups in terms of blood loss volume (5.9±16.8 and 5.4±4.6 mL, respectively; P=0.48; Figure 3), postoperative hospital stay duration (4.0±2.0 and 4.3±3.6 days, respectively; P=0.21; Figure 4), or period of postoperative oral analgesic use (10.7±5.4 and 10.1±3.4 days, respectively; P=0.89; Figure 5). There were no intraoperative complications, such as intraoperative bleeding in either group. In the SPT group, there was one case (1.4%) of postoperative left phrenic nerve paralysis and one case (1.4%) of transient paroxysmal atrial fibrillation. No deaths occurred.
Discussion
In recent years, VATS and robot-assisted thymectomy have been generally performed using a lateral thoracic approach to avoid a median sternotomy (5). However, when using a lateral thoracic approach, it is difficult to identify the contralateral phrenic nerve and to secure the surgical field in the neck. We have previously reported on SPT, DPT, and TRT as the three approaches for performing thymectomy via the subxiphoid approach (5-7). The advantages of using a subxiphoid approach include the fact that sternotomy is unnecessary, there is less pain, and the cosmetic outcome is superior. Another advantage is that the camera scope can be inserted via the subxiphoid approach, meaning that the same visual field can be obtained as the median sternotomy approach. Furthermore, it is easier to identify the neck and bilateral phrenic nerves than performing a VATS thymectomy via a lateral thoracic approach (9). In addition, when using a lateral thoracic approach, if there is an injury to the left brachiocephalic vein, it is difficult to clamp the vessel peripherally at the site of the injury. However, because surgery is performed in the supine position when operating via a subxiphoid approach, one advantage is that the procedure can be rapidly converted to a median sternotomy and the injury can be repaired.
In this study, we investigated the early outcomes of the two subxiphoid approaches. In terms of the operative time, TRT was longer; however, we believe this was because of the time it takes to set up the robotic system and the higher proportion of thymomas in the TRT group. Previously, we reported that the blood loss volume and the period of postoperative analgesic use were lower during SPT, and that the surgery was more minimally invasive compared with VATS thymectomy via a lateral thoracic approach (9). The results demonstrated that there were no significant differences in TRT compared to SPT in terms of the blood loss volume, postoperative hospital stay duration, and period of postoperative analgesic use. This indicates that TRT may be as equally minimally invasive as SPT. Moreover, there were few complications, and irrespective of the approach, the surgery was safely performed.
SPT is the least invasive approach because the intercostal space is not crossed, resulting in a lack of intercostal nerve injuries. However, one disadvantage of SPT is the difficulty of the surgery. Training is required to learn the highly specific technique of single-port surgery. For the dissection of the left lobe of the thymus, the grasper forceps are bent to the right to pull the thymus to the right side of the patient. The surgeon is required to cross the hands. For the dissection of the right lobe of the thymus, the grasper forceps are bent to the left to pull the thymus to the left side of the patient. Training with a dry box is effective for learning these techniques. However, because the instruments and camera are inserted via a single port during SPT, there is interference between the instruments and suturing is difficult.
During DPT, which is performed using the same approach as SPT but with an additional port, there is no interference caused by the surgeon using the forceps in both hands, and, compared with SPT, the surgical procedure and suturing are significantly easier. When this approach is used, a single intercostal space is crossed; therefore, intercostal nerve injury can only occur in one intercostal space. However, when performing VATS thymectomy, three or more intercostal spaces are crossed, meaning that the extent of pain and intercostal nerve injury are less frequent when performing DPT. We recommend performing DPT first for the surgeon to become accustomed to the subxiphoid approach before initiating SPT. DPT is a useful approach when treating cases in which technical challenges arise or in cases that require suturing, such as pericardial reconstruction. These challenges may be noted before initiating SPT or during SPT.
The major advantage of the da Vinci surgical system is the articulated arm. Articulated forceps make it possible to perform dissection in a natural direction within a narrow space. This is a major advantage compared with the linear tools that are used during normal VATS surgery. On the basis of our experience, combined resection of the pericardium or reconstruction of the pericardium using prosthesis is possible during DPT; however, it is not easy to perform. We have found that the use of the robotic system makes surgery easy to perform. We do not have any experience of vessel closure other than the use of a stapler; however, a robotic system support may be required when more precise vascular closure is required. The robotic system makes it possible to perform endoscopic surgery, which to date surgeons have not been able to perform manually.
Owing to its minimal invasiveness, we consider SPT to be indicated in cases without infiltration that require thymectomy or extended thymectomy. SPT can be performed until partial lobectomy, even in cases where the tumor has infiltrated the lungs (11). In cases where infiltration of the pericardium is suspected, DPT and TRT are more appropriate than SPT because of the requirement for suturing the resulting deficit in the pericardium. In cases where there is infiltration of the heart, great vessels, or left brachiocephalic vein, it is standard to perform a median sternotomy; however, if there is only partial infiltration of the left brachiocephalic vein, then DPT or TRT could be used. In cases where the thymoma has infiltrated the surrounding organs, the extent of infiltration should be used to determine whether to select DPT, TRT, or median sternotomy.
There were a number of limitations to this study. This was a non-randomized, retrospective study, the sample size was small, and the surgical indications were biased. For example, TRT was performed on patients who consented to bear the treatment cost, which is not covered under health insurance. This, therefore, led to an appreciable selection bias.
In conclusion, it is possible to perform surgery safely via a subxiphoid approach. Selecting the appropriate subxiphoid approach on the basis of the degree of progression of the thymoma is imperative.
Going forward, we will need to investigate the long-term treatment outcomes of treating myasthenia gravis and thymoma via a subxiphoid approach.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Landreneau RJ, Dowling RD, Castillo WM, et al. Thoracoscopic resection of an anterior mediastinal tumor. Ann Thorac Surg 1992;54:142-4. [PubMed]
- Sugarbaker DJ. Thoracoscopy in the management of anterior mediastinal masses. Ann Thorac Surg 1993;56:653-6. [PubMed]
- Cooper JD, Al-Jilaihawa AN, Pearson FG, et al. An improved technique to facilitate transcervical thymectomy for myasthenia gravis. Ann Thorac Surg 1988;45:242-7. [PubMed]
- Kido T, Hazama K, Inoue Y, et al. Resection of anterior mediastinal masses through an infrasternal approach. Ann Thorac Surg 1999;67:263-5. [PubMed]
- Cerfolio RJ, Bryant AS, Minnich DJ. Operative techniques in robotic thoracic surgery for inferior or posterior mediastinal pathology. J Thorac Cardiovasc Surg 2012;143:1138-43. [PubMed]
- Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [PubMed]
- Suda T, Ashikari S, Tochii D, et al. Dual-port thymectomy using subxiphoid approach. Gen Thorac Cardiovasc Surg 2014;62:570-2. [PubMed]
- Suda T, Tochii D, Tochii S, et al. Trans-subxiphoid robotic thymectomy. Interact Cardiovasc Thorac Surg 2015;20:669-71. [PubMed]
- Suda T, Hachimaru A, Tochii D, et al. Video-assisted thoracoscopic thymectomy versus subxiphoid single-port thymectomy: initial results†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i54-i58. [PubMed]
- Masaoka A, Monden Y, Nakahara K, et al. Follow-up study of thymomas with special reference to their clinical stages. Cancer 1981;48:2485-92. [PubMed]
- Suda T, Ashikari S, Tochii S, et al. Single-incision subxiphoid approach for bilateral metastasectomy. Ann Thorac Surg 2014;97:718-9. [PubMed]


