Chest wall stabilization and reconstruction: short and long-term results 5 years after the introduction of a new titanium plates system
Introduction
Chest wall integrity and stability are the main factors that ensure the protection of intrathoracic organs and an adequate respiratory function. The thoracic surgeon often has to deal with neoplastic, traumatic and malformative diseases affecting the chest wall and requiring the demolition and reconstruction or stabilization of the thoracic cage. For this purpose, many techniques have been proposed, including the use of various and different materials, but to date there are still no clear guidelines in the management of chest wall diseases.
About 5 years ago, in 2010, a new dedicated titanium plates system (Synthes®) was introduced for the treatment of chest wall diseases and is nowadays available in the current practice of the thoracic surgeon (1,2). However, to the best of our knowledge, just one study about long-term outcome of patients in whom these plates were implanted, and only for post-traumatic chest wall stabilization, has been published (3). In our retrospective study we report short and long-term results obtained with this new system for the stabilization and reconstruction of the chest wall in neoplastic, traumatic and malformative diseases.
Materials and methods
From January 2010 to December 2014, 27 consecutive patients (22 males, 5 females), with a median age of 60 years (range: 16–83 years), were treated with the dedicated Synthes® titanium system (plates, splints and screws) for sternum and ribs reconstruction and stabilization (Synthes®, Solothurn, Switzerland). In particular, we used both the dedicated sternal system (Synthes® Sternal Fixation System) and the dedicated rib system (Synthes® MatrixRIB Fixation System).
As concerns the indications, there were 11 patients with neoplastic diseases (3 with primary and 8 with secondary chest wall tumor), 15 with traumatic diseases (5 flail chest, 5 multiple ribs fractures, 3 sternal dehiscence-diastasis, 1 sternal fracture, and 1 sternoclavicular joint dislocation) and 1 with malformative disease (1 Poland syndrome).
Regarding neoplastic chest wall diseases, we treated 3 patients with primary tumors (2 chondrosarcoma and 1 plasmacytoma) and 8 with secondary tumors (1 metastasis from bladder carcinoma, 1 metastasis from liver carcinoma, 1 metastasis from breast cancer, 5 infiltrating metastases by contiguity from primary lung cancer).
Concerning traumatic chest wall diseases there were 5 patients with flail chest, 5 with multiple rib fractures (≥4), 3 with sternal dehiscence-diastasis (in 2 cases complication of sternotomy for coronary artery bypass graft surgery and in 1 case due to cardiopulmonary resuscitation after cervico-sternotomy for removal of a giant endothoracic goiter), 1 with sternal fracture, 1 with sternoclavicular joint dislocation.
The only case of malformative chest wall disease was a patient with Poland syndrome.
All patients underwent pre-operative chest wall tri-dimensional computed tomography (CT) study and, whenever possible, cardio-respiratory function evaluation including electrocardiogram, echocardiogram, spirometry with plethysmography and measurement of DLCO (the majority of patients with trauma could not undergo this last evaluation because of the emergency treatment).
Short-term results were evaluated as: operating time, post-operative morbidity, mortality, hospital stay. Long-term results were evaluated as: survival, plates-related morbidity, spirometric values, chest pain [using the Verbal Rating Scale (VRS) and the SF12 standard V1 questionnaire].
The study did not require ethics approval as our Hospitals had purchased this new titanium system and approved its use for treatment of chest wall diseases; however, all patients gave informed consent before operation, except in cases of emergency surgery (patients with flail chest under mechanical ventilation), where informed consent was obtained from relatives.
Results
A median of 2 (range: 1–10) titanium plates/splints were implanted in each patient.
Median operating time was 150 min (range: 115–430 min) and no intra-operative complication occurred. A dedicated Synthes® specialist assisted the surgeons during the implantation of plates, splints and screws, which were implanted according to the instructions recommended by Synthes®.
As concerns the type of Synthes® titanium system, in the traumatic disease group of 15 patients, 3 cases with sternal dehiscence-diastasis were treated with the dedicated sternal system, while 5 flail chest, 5 multiple ribs fractures, 1 sternal fracture and 1 sternoclavicular joint dislocation with both the dedicated sternal and rib system; in the neoplastic disease group of 11 patients chest wall reconstruction was made with both the dedicated sternal and rib system; in the malformation case (Poland syndrome) we used the dedicated rib system.
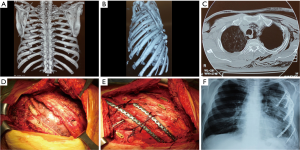
About the materials, in all fifteen patients treated for trauma, titanium plates/splints were the only material used for chest wall stabilization (Figure 1). As regards the eleven patients treated for neoplastic chest wall diseases, in two of the three cases with primary tumor (one chondrosarcoma undergoing sternotomy and the other one resection of three ribs) reconstruction of the thoracic cage was achieved by titanium plates together with the utilization of a mersilene mesh (MERSILENE™ Polyester Fiber Mesh, ETHICON, LLC., USA) while in the other case (plasmacytoma undergoing resection of three ribs) with titanium plates only; in the 8 cases with secondary tumors, reconstruction was obtained by titanium plates together with the utilization of: mersilene mesh in 4 (2 lung adenocarcinoma, 1 lung squamous cell carcinoma, 1 undifferentiated lung cancer), mersilene mesh and pectoralis major muscles in 1 (lung adenocarcinoma), latissimus dorsi muscle flap in 1 (metastasis from bladder carcinoma), mersilene mesh and latissimus dorsi muscle flap in 1 (metastasis from breast cancer), mersilene mesh and serratus anterior muscle and abdominal external oblique muscle in 1 (metastasis from liver carcinoma). In the patient with Poland syndrome the reconstruction and stabilization of the chest wall was achieved by titanium plates together with the utilization of a mersilene mesh and latissimus dorsi muscle flap (Table 1).

Full table
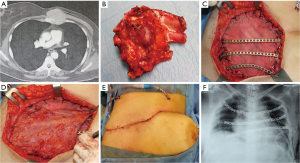
Cooperation with plastic surgeons was necessary when muscle flaps were used for reconstruction of the chest wall (Figure 2).
Post-operative course was uneventful in 15 patients (55.6%). Ten patients (37%) presented various minor complications (anemia 6, prolonged air and fluid leak 2, increased levels of amylasemia and lipaemia 2, fever and seroma 1), which were resolved with medical treatment. In 2 patients (7.4%) major complications occurred: pneumonia with respiratory failure and need for mechanical ventilation, in one case cured with antibiotic therapy and in the other leading to death 41 days after surgery, due to sepsis.
Median post-operative hospital stay was 13 days (range: 5–129 days).
Dividing patients in two groups of traumatic and non-traumatic chest wall disease, median post-operative hospital stay was 26 days (range: 5–129 days) in the first one and 13 days (range: 9–26 days) in the second one. In the first group median post-operative intensive care unit (ICU) stay was 1 day (range: 0–29 days), while in the second group no patient required ICU.
No 30-day post-operative mortality was observed. Our short-term results are summarized in Table 2.
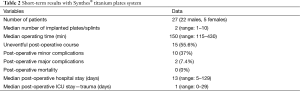
Full table
At a median follow-up of 20 months (range: 1–59 months), 21 patients (78%) were alive, 6 patients (22%) died (one at 41 days from surgery for sepsis due to pneumonia, one at 5 months and another one at 6 months for progression of neoplastic disease, one at 6 months due to cardiac arrhythmia, one at 9 months for heart attack, one at 18 months for distant metastases).
Differentiating patients in two groups of neoplastic and non-neoplastic (traumatic and malformative) chest wall disease, the mean and median follow-up were 15 and 13 months (range: 4–36 months) in the first one and 30 and 31.5 months (range: 1–59 months) in the second one, respectively.
During follow-up, three patients presented long-term plates-related morbidity: plates rupture in 2 cases and dislodgment of the pin of a plate in another one.
The first case of rupture of a sternal plate occurred in a 48-year-old male patient after surgical treatment for a severe anterior flail chest with complete transverse fracture of the sternum: the plate had been placed in a vertical position to allow the reunion of the two bone stumps and follow-up chest X-ray at 18 months from surgery showed rupture of the titanium plate at the middle of its length. As the patient complained intense pain, a new surgical operation was required in order to remove the plate, which was not substituted because a complete and stable bone callus was formed and he is doing well 33 months after surgery.
The second case of plate rupture occurred in a 40-year-old female patient that had been operated on for a rib chondrosarcoma; the titanium plate had been contoured to fit the defect of the thoracic cage caused by three resected ribs and follow-up chest CT scan at 23 months from the operation revealed a rupture of the titanium plate at the middle of its length. However, as the patient was asymptomatic and complained no pain, we decided for a radiological follow-up and the patient is doing well at 35 months from surgery.
Finally, we observed a case of dislodgment of the pin of a sternal plate used for the reconstruction and stabilization of the anterior chest wall 1 month after a sternotomy for a chondrosarcoma in a 50-year-old male patient. As he complained intense pain and there was the risk of dislocation of the two parts of the plate joined by the pin, a second surgical look was necessary for repositioning the pin and the patient is doing well 36 months after surgery.
Excluding from the evaluation five patients who died earlier, median spirometric values at 1-year from surgery were: FVC 3.31 L (90%) (range: 2.42–5.28 L; 73–118%), FEV1 2.46 L (78%) (range: 1.28–3.37 L; 38–104%), DLCO 20.9 mL/mmHg/min (76%) (range: 12.8–31.8 mL/mmHg/min; 48–101%), these data confirming the restoration of a good respiratory function.
On 21 alive patients, evaluated with the VRS, 7 (33.3%) reported no pain (VRS score 0), 10 (47.6%) mild pain (score 2), 4 (19.1%) moderate pain (score 4), no-one severe pain (score >4).
Moreover, at evaluation with the SF12 standard V1 questionnaire, 15 patients (71.5%) reported none or mild pain and 6 (28.5%) moderate pain influencing quality of life.
Our long-term results are summarized in Tables 3,4.

Full table

Full table
Discussion
In recent years, considering the favorable experiences obtained with titanium implants in other fields of prosthetic surgery (orthopedics, maxillofacial surgery), titanium systems constituted by dedicated plates, splints and screws for the reconstruction and stabilization of the chest wall (Synthes®, STRATOSTM) have been produced by industry and the use of titanium has been introduced in the procedures of reconstruction after demolition for neoplastic disease, to fix fractures of the thoracic cage after trauma and sternal dehiscence-diastasis and to treat malformative disease (1,2,4-9).
Titanium is an ideal prosthetic material, as it has a high resistance to corrosion, a low specific weight, a remarkable resistance to traction, it is diamagnetic and compatible with magnetic resonance imaging (MRI), but above all is biologically inert and highly biocompatible. Synthes® titanium system for the chest wall is made up of conformable bars with a variable number of holes, which can be precontoured with dedicated tools and fastened by means of threaded screws to the ribs and to the sternum. To obtain an optimal fixation, it is fundamental to lock the screws to the bone bicortically and to use at least three screws for blocking each side of the bar.
Our study has confirmed the effectiveness of the dedicated Synthes® sternal and rib titanium systems (plates, splints and screws) for the reconstruction and stabilization of the thoracic cage.
The surgical team “feeling” with these new devices was good, confirming the ease of use and the rapid learning curve. This titanium system revealed to be easy to handle and durable, adaptable to a wide variety of chest wall defects, allowing to recreate the anatomical and physiological appearance of the thoracic cage. However, while in all 15 patients treated for trauma, titanium plates/splints were the only material used for chest wall stabilization, in 11 patients treated for neoplastic chest wall diseases and in the patient with malformative disease (Poland syndrome) the reconstruction with the titanium system required integration with traditional technique such as mersilene mesh and various muscle or muscle flaps. These data confirm that after demolition of the chest wall for neoplastic disease or in case of malformative defect of the chest wall, this titanium system should be preferably associated with the use of meshes and muscle flaps.
Cooperation with plastic surgeons was fundamental in large chest wall demolitions for cancer and in the case of Poland syndrome, to prepare muscle flaps for reconstruction of the chest wall.
Median operating time was 150 min and the learning curve fast enough to allow a progressive reduction of surgical time.
No intra-operative complication occurred, also thanks to the fact that a dedicated Synthes® specialist assisted the surgeons during the implantation of plates, splints and screws.
Post-operative course was uneventful in 15 patients (55.6%) and 10 patients (37%) presented only minor complications, which were resolved with medical treatment. In 2 patients (7.4%) pneumonia with respiratory failure and need for mechanical ventilation was the major complication, cured in one case with antibiotic therapy and causing death in the other one, due to consequent sepsis. Actually, these major complications were related to the higher risk of infection in these two patients (pre- and post-operative ICU stay in one and a condition of immunosuppression in the other one).
Median post-operative hospital stay was 13 days, with a really wide range (5–129 days) due to the heterogeneity of patients. However, dividing patients in two groups treated for traumatic and non-traumatic chest wall disease, median post-operative hospital stay was longer (26 days) in the first one compared to the second one (13 days), probably due to the fact that polytrauma patients required more days to recover from other complications or associated problems (abdominal, orthopedic, neurosurgical, vascular, etc.). Moreover, in the first group median post-operative ICU stay was 1 day only, showing the effectiveness of this titanium system, which allowed early weaning from mechanical ventilation, with restoration of a normal respiratory function, avoiding the necessity of tracheostomy and the risk of ICU related complications such as pneumonia. This result is in line with that of other studies, showing a better outcome in patients with flail chest treated with surgical stabilization compared to those who received conservative treatment such as internal pneumatic stabilization, which requires a longer ICU stay with a higher risk of complications and tracheostomy (9-13).
There was no 30-day post-operative mortality, even in large demolition of the thoracic cage for neoplastic disease and in severe polytrauma in which reconstruction and stabilization with this titanium system allowed to restore a normal anatomy and physiology of the chest wall.
At a median follow-up of 20 months, 21 patients (78%) were alive and 6 patients (22%) dead, three for tumor progression, two for cardiac disease and one for pneumonia and sepsis. However, in our experience, distinguishing patients in two groups of neoplastic and non-neoplastic chest wall disease, we observed a shorter mean and median follow-up in the first group (15 and 13 months respectively) compared to the second group (30 and 31.5 months respectively), probably due to the natural history of the underlying tumoral disease.
During follow-up, three patients presented long-term plates-related morbidity: plates rupture in two cases (one patient treated for anterior flail chest and one patient for a rib chondrosarcoma) and dislodgment of the pin of a plate in another one (after sternotomy for chondrosarcoma). A second operation was required in the patient treated for flail chest and that of sternotomy for chondrosarcoma, who were complaining intense chest pain, maybe due to abnormal movements of the plates during breaths; however, in the first case removal of the plates was performed without substitution because a complete and stable bone callus was formed, while in the second one the pin was simply repositioned. In the patient operated for a rib chondrosarcoma the ruptured titanium plate caused no pain at all, thus we decided for a radiological follow-up and the patient is doing well at 35 months from surgery.
It should be underscored that complications were recognized thanks to radiological follow-up (chest X-ray and CT scan), which is always recommended in patient treated with this titanium devices.
Moreover, in both cases plate rupture occurred at the middle of its length and we assume that this site was probably the most stressed point during normal breaths, which is a dynamic condition that again makes radiological follow-up mandatory. A case of fracture of titanium plate (removed due to pain and cough) has been reported in the literature by other authors, which occurred following a chest impact during sport (14), while in our two cases no trauma potentially causing plates rupture was reported by patients.
As concerns long-term results, spirometric values at 1-year from surgery showed the recovery of a good respiratory function, with a median FVC of 3.31 L (90%), FEV1 of 2.46 L (78%) and DLCO of 20.9 mL/mmHg/min (76%), thus confirming the validity of this titanium system in restoring a normal anatomy and physiology of the thoracic cage and of the chest wall. At post-operative observation and follow-up no patient showed or complained about any functional limitation or impairment of respiratory movements. Moreover, in our experience no significant post-operative chest wall deformity was observed. The restoration of a good respiratory function had already been demonstrated in other studies on patients undergoing surgical stabilization compared to those who received conservative treatment for flail chest, although in these studies also different devices had been used for fixation of fractures (Kirschner wires, Judet struts) (9-13). Thus our study is the first one reporting results in term of respiratory function obtained with the Synthes® titanium system, not only in trauma patients but also in those with neoplastic and malformative chest wall diseases.
Another important long-term result regarded the evaluation of the intensity of chest pain and the influence of pain on the quality of life, which were measured and obtained using the VRS and the SF12 standard V1 questionnaire, respectively.
On 21 alive patients, evaluated with the VRS, 7 (33.3%) reported no pain (VRS score 0), 10 (47.6%) mild pain (score 2), 4 (19.1%) moderate pain (score 4), no-one severe pain (score >4), that is more than 80% of patients complained no significant pain.
Moreover, at evaluation of the influence of pain on the quality of life with the SF12 standard V1 questionnaire, most patients (71.5%) reported none or mild pain and only about one third of them (28.5%) complained of moderate pain influencing personal quality of life.
The reduction of pain had already been issued by other Authors, as concerns treatment of trauma patients (11), but not of non-traumatic chest wall diseases too, as was in our study.
In conclusion, an optimal chest wall stabilization and reconstruction in neoplastic, traumatic and malformative diseases was achieved with the Synthes® titanium plates/splints and screws system, with minimal morbidity, no post-operative mortality, acceptable operating time and post-operative hospital stay. Long-term restoration of a normal respiratory function was achieved, with minimal plates-related morbidity and chest pain. Largest studies are needed to better standardize the use of this new titanium system, in order to minimize morbidity and mortality and to improve results in term of respiratory function, chest pain and quality of life.
Acknowledgements
We kindly thank Mr. Francesco Fiore, specialist from DePuy Synthes, for his professionality and his permanent and constant assistance of our surgical team during the implantations, regardless from time and hours of the day. We could use the Synthes® titanium system at the best of its potential thanks to his valuable advice and indications.
Footnote
Conflicts of Interest: This study was presented on the 6th October 2015 at the 29th EACTS Annual Meeting, Amsterdam, The Netherlands, 4–7 October 2015.
References
- Iarussi T, Pardolesi A, Camplese P, et al. Composite chest wall reconstruction using titanium plates and mesh preserves chest wall function. J Thorac Cardiovasc Surg 2010;140:476-7. [Crossref] [PubMed]
- Billè A, Okiror L, Karenovics W, et al. Experience with titanium devices for rib fixation and coverage of chest wall defects. Interact Cardiovasc Thorac Surg 2012;15:588-95. [Crossref] [PubMed]
- Billè A, Okiror L, Campbell A, et al. Evaluation of long-term results and quality of life in patients who underwent rib fixation with titanium devices after trauma. Gen Thorac Cardiovasc Surg 2013;61:345-9. [Crossref] [PubMed]
- Hamad AM, Marulli G, Bulf R, et al. Titanium plates support for chest wall reconstruction with Gore-Tex dual mesh after sternochondral resection. Eur J Cardiothorac Surg 2009;36:779-80. [Crossref] [PubMed]
- Rocco G, Fazioli F, La Manna C, et al. Omental flap and titanium plates provide structural stability and protection of the mediastinum after extensive sternocostal resection. Ann Thorac Surg 2010;90:e14-6. [Crossref] [PubMed]
- Berthet JP, Wihlm JM, Canaud L, et al. The combination of polytetrafluoroethylene mesh and titanium rib implants: an innovative process for reconstructing large full thickness chest wall defects. Eur J Cardiothorac Surg 2012;42:444-53. [Crossref] [PubMed]
- Kalab M, Molitor M, Kubesova B, et al. Use of allogenous bone graft and osteosynthetic stabilization in treatment of massive post-sternotomy defects. Eur J Cardiothorac Surg 2012;41:e182-4. [Crossref] [PubMed]
- Nirula R, Diaz JJ Jr, Trunkey DD, et al. Rib fracture repair: indications, technical issues, and future directions. World J Surg 2009;33:14-22. [Crossref] [PubMed]
- Granetzny A, Abd El-Aal M, Emam E, et al. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg 2005;4:583-7. [Crossref] [PubMed]
- Ahmed Z, Mohyuddin Z. Management of flail chest injury: internal fixation versus endotracheal intubation and ventilation. J Thorac Cardiovasc Surg 1995;110:1676-80. [Crossref] [PubMed]
- Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma 2002;52:727-32; discussion 732. [Crossref] [PubMed]
- Slobogean GP, MacPherson CA, Sun T, et al. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg 2013;216:302-11.e1.
- Bottlang M, Long WB, Phelan D, et al. Surgical stabilization of flail chest injuries with MatrixRIB implants: a prospective observational study. Injury 2013;44:232-8. [Crossref] [PubMed]
- Ng CS, Wong RH, Kwok MW, et al. Delayed fracture of MatrixRIB precontoured plate system. Interact Cardiovasc Thorac Surg 2014;19:512-4. [Crossref] [PubMed]


