Clinical characteristics and risk factors of pulmonary hypertension associated with chronic respiratory diseases: a retrospective study
Introduction
Pulmonary hypertension (PH) is a progressive disease defined by excessive small pulmonary vascular remodeling and increased pulmonary vascular resistance, which can finally lead to right heart failure and even death (1,2). Significant progress has been made in understanding the epidemiology, clinical characteristics and prognosis of PH in recent years (3-7). So far, most of the studies regarding PH focused on idiopathic PH, chronic thromboembolic PH (CTEPH), PH associated with congenital heart disease and with connective tissue disease; PH associated with chronic respiratory disease was usually despised or neglected, although it is also an essential subtype of PH (8).At present, there are only few large epidemiological data related to PH in China, as well as related systematic, large and randomized clinical studies, especially for PH associated with chronic respiratory diseases and/or hypoxia (9,10). Except for chronic obstructive pulmonary disease (COPD)-associated PH, hypoxic diseases, such as bronchiectasis, interstitial lung disease, and obstructive sleep apnea hypopnea syndrome (OSAHS), -induced PH lack systematic studies designed to obtain a comprehensive understanding of their clinical features. Thus, in this study, we aim to search for the common respiratory diseases which are highly-associated with PH, and to describe the clinical characteristics and risk factors associated with the progression to severe PH.
Materials and methods
Patients
This retrospective observational study was conducted at Guangzhou Institute of Respiratory Disease. A total of 693 patients hospitalized from January 2010 to January 2013 were enrolled. All patients had signed written informed consent. All procedures were approved by the Ethics Committee of The First Affiliated Hospital of Guangzhou Medical University. PH was diagnosed by echocardiography examination (tricuspid regurgitation velocity >2.8 m/s and PASP>36 mmHg) (11,12). All patients suffered from one or more chronic respiratory diseases (chronic thromboembolic disease included): congenital heart disease, left heart-related diseases like valvular disease, rheumatologic disease such as systemic lupus erythematosus and sicca syndrome, hyperthyroidism. Chronic Thromboembolic Pulmonary Hypertension (CTEPH) patients were also included, because when we classified those patients with single respiratory disease related to PH, we identified that 5.1% of them diagnose as pulmonary embolism (PE). In those cases which probably could define as CTEPH for their pulmonary artery pressure increased after at least three-month effective anticoagulation and they had embolism in pulmonary arteries. We did not specifically exclude CTEPH form PE in this study for lack of information. Other conditions that may increase the pulmonary arterial pressure were excluded.
Clinical data
The name, gender and age of all the patients were documented. All patients underwent echocardiography with Philips iE33 cardiac color Doppler ultrasonography and were performed by the same technician. Echocardiography (ECHO) is an important modality in the noninvasive assessment of PH and has been used to screen for the disease, determine right and left heart structure and function, and assess response to therapy in patients with PH. The ACCF/AHA 2009 Expert Consensus Document on Pulmonary Hypertension recommended ECHO as the most appropriate screening examination for PH diagnosis. ECHO can assess for right atrial enlargement, right ventricular enlargement, pericardial effusion, left ventricular systolic or nonsystolic dysfunction, left atrial or ventricular enlargement, and valvular disease as part of the initial evaluation of patients suspected of having PH. Moreover, a meta-analysis confirmed that echocardiography is a useful noninvasive way to screen for PH which can determine whether PASP is normal, mildly elevated or remarkably elevated. At present, right heart catheterization (RHC) is the gold standard for diagnosis of PH. However, due to its invasive nature and high cost, the use of RHC is limited in China, so we count on ECHO data in patients with severe PH in our study.
According to international standards of PH classification, patients were divided into 3 groups: the mild group (36≤ PASP <50 mmHg); the moderate group (50≤ PASP <70 mmHg) and the severe group (PASP ≥70 mmHg) (13). For this analysis, we only included COPD patients who met the American Thoracic Society (ATS) definition of spirometry proven COPD (i.e., FEV1/FVC ratio <0.70 on tests meeting ATS quality standards), and those who provided all information needed for GOLD staging and appropriate self-assessment.
Clinical data within 5 days of hospitalization were collected as follows: (I) clinical diagnosis; (II) the onset of symptoms and time; (III) medical history; (IV) personal history and family history; (V) echocardiography [PASP, right ventricular diameter (RV) and right atrium diameter (RA)]; (VI) arterial blood gas analysis [partial pressure of oxygen (PaO2), and partial pressure of carbon dioxide (PaCO2)]; (VII) blood examination [hemoglobin (HB), hematocrit (HCT), mean corpuscular hemoglobin concentration (MCHC)]; (VIII) N-terminal pro brain natriuretic peptide (NT-proBNP); (IX) D-dimer. Risk factors of moderate-to-severe PH (PASP >50 mmHg) including age, HCT, HB, MCHC, RV, RA, PaO2, PaCO2, NT-proBNP and D-dimer, were screened from a total of 396 patients.
Statistical analysis
All statistical analyses were performed by the SPSS 13.0 statistical software package (SPSS Inc; Chicago, Illinois, USA). Data were expressed as the mean ± SD, the number and proportions, or as the median and inter quartile range. Differences among proportions were compared with Pearson Chi-Square test or Fisher’s exact test. Differences among multiple groups were analyzed using the rank test and multiple comparisons were performed by Kruskal-Wallis H test. Survival analyses were performed using Kaplan-Meier method and Log-Rank test to compare differences of the durations from the onset of symptoms to the diagnosis of PH among groups. Risk factors screening accessed the univariate regression analysis and multiple-stepwise logistic regression analysis, and odds ratio (OR) and its 95% confidence interval (CI) was calculated for each variable. A P value <0.05 was considered to be statistically significant.
Results
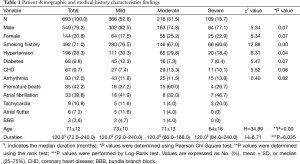
A total of 693 patients were hospitalized with diagnosis of PH. The baseline demographic and clinical characteristics are summarized in Table 1. About 366 (52.8%) patients were classified in the mild group, 218 (31.5%) patients in the moderate group and 109 (15.7%) in the severe group. The mean PASP was 42.0±4.3 mmHg for the mild group; 59.3±5.2 mmHg for the moderate group; and 84.5±12.1 mmHg for the severe group. Baseline characteristics of these patients were: mean age 71±12 years, 79.2% men, smoking/tobacco abuse 71.0%, hypertension 28.3%, diabetes mellitus 9.8%, coronary heart disease 9.7%, and arrhythmia 12.0% of patients. The ratio of patients with smoking history in the mild group was significantly higher than that in the moderate group and the severe group (P<0.01), as was the hypertension history (P<0.05).
Full table
The median duration of all patients from the onset of symptoms to the diagnosis of PH was 120.0 (72.0–240.0) months. There is a significant difference in the duration among the three groups (P<0.05).
Symptoms
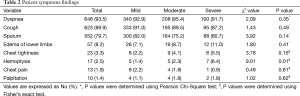
Patient symptoms are summarized in Table 2. The most common symptom was dyspnea (93.5%). Other common symptoms were cough (89.9%), sputum (79.7%), lower extremity edema (8.2%), chest tightness (3.3%), hemoptysis (2.5%), chest pain (1.9%) and palpitations (1.4%). The ratio of hemoptysis was significantly higher in the severe group than that in the mild and moderate groups (P<0.05).
Full table
Respiratory diseases
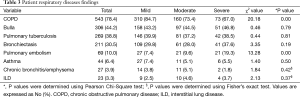
PH-related respiratory diseases found in the patients are shown in Table 3. There were 198 (28.6%) patients with a single respiratory disease related to PH. COPD was the most common PH-related respiratory disease (n=151, 76.3% of patients), and others include bronchiectasis (n=13, 6.6% of patients), pulmonary embolism (n=10, 5.1% of patients), chronic bronchitis/emphysema (n=8, 4.0% of patients), interstitial lung disease (including idiopathic interstitial pneumonia, airway-centered interstitial fibrosis, centrilobular fibrosis, and bronchiolitis interstitial pneumonia) (n=6, 3.0% of patients), OSAHS patients with an extremely high apnea-hypopnea index (AHI) score (n=3, 1.5% of patients), diffuse panbronchiolitis (n=2, 1.0% of patients), asthma (n=2, 1.0% of patients) and others (n=3, 1.5% of patients). However, most patients were found to have at least two or more underlying respiratory diseases (n=495, 71.4% of patients). There were significantly more patients with COPD in the mild group compared to those in moderate and severe groups (P<0.01), whereas the number of patients with pulmonary embolism was significantly higher in the severe group compared to the mild and moderate groups.
Full table
Clinical parameters
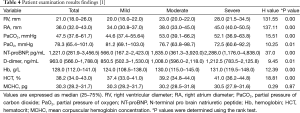
Patients’ examination results are shown in Tables 4,5. There were significant differences concerning those except for the MCHC among the three groups of different severity of PH (P<0.05). MCHC from three tested groups showed no statistic difference (P=0.87) (Table 4). In addition, HB, HCT, PaCO2, NT-proBNP, D-dimer, RV and RA diameter in the severe and the moderate groups were significantly higher than those in the mild group, while PaO2 was inversely lower than that in the mild group (P<0.05) (Table 5).
Full table
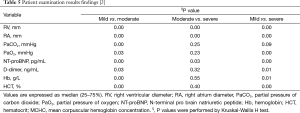
Full table
Risk factors
Clinical data within 5 days of hospitalization were collected from a total of 396 patients. Briefly, 204 (51.50% of patients) patients were in the mild PH group, while 192 (48.48% of patients) were in the moderate-to-severe PH group.
Univariate analysis demonstrates that relevant factors include increased RV size (RV>20 mm), elevated NT-proBNP, HCT, PaCO2, age and PaO2 (P<0.05). Elevated NT-proBNP, HCT and PaCO2 present OR values >1, while age and PaO2 present OR values <1 (Table 6). Variables with significant results in the univariate analysis were also determined by multiple-stepwise logistic regression analysis. Results were displayed in Table 6. Increased RV size (RV >20 mm) (OR=3.53, 95% CI, 2.17–5.74), increased NT-proBNP (OR=2.44, 95% CI, 1.51–3.95), HCT (OR=1.03, 95% CI, 1.00–1.07), and PaCO2 (OR=1.01, 95% CI, 1.00–1.03) were respectively considered as an independent risk factor of patients with moderate-to-severe PH (OR>1).
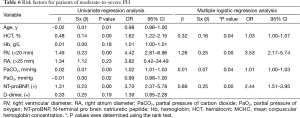
Full table
Discussion
This is a systematic retrospective observational study which highlights the clinical features and risk factors of PH related to common chronic pulmonary diseases [Group 3 and Group 4 of PH in World Health Organization (WHO) classification] in Chinese population patients. Previously, Barberà et al. demonstrated that the most effective treatment for PH associated with chronic hypoxic respiratory disease was long-term oxygen therapy (14). Alternative effective therapy is currently unavailable. Therefore, early recognition and intervention is important for the prognosis of those patients. At present, right heart catheterization is the gold standard for diagnosis of PH. However, due to its invasive nature and high cost, the clinical application of RHC is limited in China. In 2009, the ACCF/AHA 2009 Expert Consensus Document on Pulmonary Hypertension recommended echocardiography as the most appropriate screening examination for PH diagnosis (11).
The first research article on PH patients in China was published in 2007 by Jing et al. (7). which reviewed 72 hospitalized patients with idiopathic pulmonary arterial hypertension and familial pulmonary arterial hypertension with a mean PASP of 98 mmHg. The Switzerland registration reported by Fischler et al. (9) included 17 patients with hypoxic disease associated-PH with a mean mPAP of 47 mmHg. In our study, the mean age was 71±12 years, the male/female ratio was 3.8:1 and the mean PASP was 54.2±16.5 mmHg. The results of our study suggest that male patients symptomatic with chronic respiratory disease-associated PH more than female patients.
A potential explanation for this phenomenon is that there are more male than female smokers in China. Santos et al. (4) showed that smoking could cause lung vascular injury and remodeling. The vascular remodeling plays a key role during the PH pathogenesis. In this study, the proportion of patients with smoking history was up to 71.0%. There was a significant difference among the proportions of patients with smoking history and was highest in the mild group. The major reason for this difference may be that the male/female ratio was higher in the mild group (4.7:1) than that in the moderate group (3.0:1) and the severe group (3.4:1). Smoking has previously been proven as a risk factor for hypertension. In our study, the majority of patients with a smoking history were found in the mild group (76.5%). Therefore, it’s not surprising that the mild group contained significantly more patients with hypertension history than the other two groups (P<0.05) (Table 1).
The median duration from the onset of symptoms to diagnosis was 120.0 (72.0–240.0) months. This finding was different than the registry studies on idiopathic and familial PAH patients reported by Rich et al. (5) (24.4±58.8 months), Humbert et al. (15) (27 months) and Jing et al. (7) (26.4±27.6 months). The duration had significant differences among the three groups (P<0.05), suggesting that the patients with PH usually suffer from a long period (median 10 years) of chronic respiratory diseases and the severity of PH is relevant to the duration of the underlying disease. Weitzenblum et al. (16) found that mPAP increased by an average of 1.47 mmHg each year in a small follow-up study of COPD patients.
Dyspnea is the most common presenting symptom of PH patients. As the disease progresses, the pulmonary arterial pressure increases and overwhelms the compensatory mechanism. Chaouat et al. (17) reported that COPD was usually associated with mild PH and it was clinically difficult to distinguish PH from other airway diseases. Before the obvious symptoms of pulmonary heart disease occur, including lower extremity edema and abdominal distension, it is difficult to identify PH in patients with no specific symptoms. Dyspnea was the most common symptom in our study (93.51%), similar to the American registry reported by Rich et al. (5) and D’alonzo et al. (6) Other similar symptoms included lower extremity edema, chest pain and palpitations. In our study, chronic respiratory disease-associated PH also presented with cough, sputum and hemoptysis, which were different presentations than other studies. Once hemoptysis occurred, PH was thought to be more serious (P<0.05). Therefore, patients presenting dyspnea and hemoptysis with a long history of chronic respiratory disease, usually 10 years or more, should be evaluated for PH.
In this study, the severity of respiratory disease-related PH was greatly dependent on the type of the underlying disease. COPD was the most common underlying disease with comorbid, generally mild-to-moderate, PH (78.35%). Chaouat et al. (17) reported that the prevalence of COPD-related severe PH was only 1.1%. But PH often occurs as a complication in patients with advanced COPD and leads to limitation of lung function, and the severity of PH is not proportional to that of the patient’s condition. CTEPH is classified as WHO Group 4 PH (12), which presents with severe PH in our study, although the prevalence was relatively low (9.6%). Interestingly, we found that pulmonary bullae (44.16%) and pulmonary tuberculosis (38.82%) were the second and third common underlying PH-related pulmonary diseases. We speculate that the destruction of the pulmonary vascular bed, as well as lung and airway irreversible injury, may play an important role in the development of this kind of PH.
Interestingly, in this study, elevated HCT presented as a risk factor in these patients. This finding is probably attributed to the secondary polycythemia caused by long-term hypoxia. Brown et al. (18) pointed out that HCT was an independent and complex risk factor for cardiovascular disease. The risk of major coronary events was significantly increased at an HCT level exceeding 46.0% compared to those with HCT less than 46.0%, even after adjustments for other risk factors (19). Some research implicated increased HCT as a risk factor for coronary events (19-21), while some other investigations did not (22-24). We indicate that in this study there might also be a threshold effect in the relationship between HCT and PH. However, studies concerning this point are so far limited and need more evidence to explain and support the relationship between HCT and PH.
NT-proBNP is a biochemical marker of myocardial cell damage and ventricular dysfunction released from the ventricle. NT-proBNP is an N-fragment of splinted BNP (brain natriuretic peptide). Both of BNP and NT-proBNP have similar physiological function that may cause vasodilatation and natriuresis. In patients with PH, the abnormal structure and function of the right heart can lead to increased NT-proBNP and BNP. Therefore the severity, effectiveness, survival and prognosis of the disease are reflected through these two biochemical markers, which are closely related to the change of hemodynamics that are important indexes for the monitor of right heart failure. Bozkanat et al. (25) found that BNP and pulmonary arterial pressure fit in a linear correlation with correlation coefficient 0.68. In patients with CTEPH, the correlation coefficient between BNP and PVR was 0.63 (26). In this study, NT-proBNP had significant differences among the three groups (P<0.01). We inferred that NT-proBNP could predict the severity of PH, decreased or persistently low levels of BNP and NT-proBNP might indicate effective control of PH hemodynamic changes in this population of PH patients.
As this was a retrospective study, the possibility of selection bias could not be avoided. However, lack of RHC data is also a limitation of our research. In addition, this was a single center clinical study. If multicenter clinical studies would be conducted nationwide on this basis, the research results from the Chinese population could be more accurate, practical and significant. We assert that these discoveries will contribute to a better understanding of the relationship between PH and chronic respiratory diseases, which in turn will benefit optimization of new treatment strategies, providing new clinical research directions and more mechanisms for future studies. These benefits would be valuable and meaningful to the prognosis of patients with PH related to chronic respiratory disease.
Acknowledgements
Funding: This work was supported by National Natural Science Foundation of China (81173112, 81470246, 81170052, 81220108, 81520108001), Guangzhou Department of Education Yangcheng Scholarship (12A001S), Guangzhou Department of Natural Science (2014Y2-00167) and Guangdong Province Universities and Colleges Pearl River Scholar Funded Scheme (2014, W Lu), China.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Farber HW, Loscalzo J. Pulmonary arterial hypertension. N Engl J Med 2004;351:1655-65. [Crossref] [PubMed]
- Galiè N, Torbicki A, Barst R, et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. Eur Heart J 2004;25:2243-78. [Crossref] [PubMed]
- Montani D, Günther S, Dorfmüller P, et al. Pulmonary arterial hypertension. Orphanet J Rare Dis 2013;8:97. [Crossref] [PubMed]
- Santos S, Peinado VI, Ramírez J, et al. Characterization of pulmonary vascular remodelling in smokers and patients with mild COPD. Eur Respir J 2002;19:632-8. [Crossref] [PubMed]
- Rich S, Dantzker DR, Ayres SM, et al. Primary pulmonary hypertension. A national prospective study. Ann Intern Med 1987;107:216-23. [Crossref] [PubMed]
- D'Alonzo GE, Barst RJ, Ayres SM, et al. Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med 1991;115:343-9. [Crossref] [PubMed]
- Jing ZC, Xu XQ, Han ZY, et al. Registry and survival study in chinese patients with idiopathic and familial pulmonary arterial hypertension. Chest 2007;132:373-9. [Crossref] [PubMed]
- Chaouat A, Naeije R, Weitzenblum E. Pulmonary hypertension in COPD. Eur Respir J 2008;32:1371-85. [Crossref] [PubMed]
- Fischler M, Speich R, Dorschner L, et al. Pulmonary hypertension in Switzerland: treatment and clinical course. Swiss Med Wkly 2008;138:371-8. [PubMed]
- Tueller C, Stricker H, Soccal P, et al. Epidemiology of pulmonary hypertension: new data from the Swiss registry. Swiss Med Wkly 2008;138:379-84. [PubMed]
- McLaughlin VV, Archer SL, Badesch DB, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association developed in collaboration with the American College of Chest Physicians; American Thoracic Society, Inc.; and the Pulmonary Hypertension Association. J Am Coll Cardiol 2009;53:1573-619. [Crossref] [PubMed]
- Galiè N, Hoeper MM, Humbert M, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J 2009;30:2493-537. [Crossref] [PubMed]
- Sciomer S, Badagliacca R, Fedele F. Pulmonary hypertension: echocardiographic assessment. Ital Heart J 2005;6:840-5. [PubMed]
- Barberà JA. Heart pathology of extracardiac origin. IV. Pulmonary hypertension in chronic respiratory diseases. Rev Esp Cardiol 1998;51:56-68. [PubMed]
- Humbert M, Sitbon O, Chaouat A, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med 2006;173:1023-30. [Crossref] [PubMed]
- Weitzenblum E, Sautegeau A, Ehrhart M, et al. Long-term oxygen therapy can reverse the progression of pulmonary hypertension in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 1985;131:493-8. [PubMed]
- Chaouat A, Bugnet AS, Kadaoui N, et al. Severe pulmonary hypertension and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2005;172:189-94. [Crossref] [PubMed]
- Brown DW, Giles WH, Croft JB. Hematocrit and the risk of coronary heart disease mortality. Am Heart J 2001;142:657-63. [Crossref] [PubMed]
- Wannamethee G, Shaper AG, Whincup PH. Ischaemic heart disease: association with haematocrit in the British Regional Heart Study. J Epidemiol Community Health 1994;48:112-8. [Crossref] [PubMed]
- Gagnon DR, Zhang TJ, Brand FN, et al. Hematocrit and the risk of cardiovascular disease--the Framingham study: a 34-year follow-up. Am Heart J 1994;127:674-82. [Crossref] [PubMed]
- Knottnerus JA, Swaen GM, Slangen JJ, et al. Haematologic parameters as risk factors for cardiac infarction, in an occupational health care setting. J Clin Epidemiol 1988;41:67-74. [Crossref] [PubMed]
- Carter C, McGee D, Reed D, et al. Hematocrit and the risk of coronary heart disease: the Honolulu Heart Program. Am Heart J 1983;105:674-9. [Crossref] [PubMed]
- Yano K, Reed DM, McGee DL. Ten-year incidence of coronary heart disease in the Honolulu Heart Program. Relationship to biologic and lifestyle characteristics. Am J Epidemiol 1984;119:653-66. [PubMed]
- Szatrowski TP, Peterson AV Jr, Shimizu Y, et al. Serum cholesterol, other risk factors, and cardiovascular disease in a Japanese cohort. J Chronic Dis 1984;37:569-84. [Crossref] [PubMed]
- Bozkanat E, Tozkoparan E, Baysan O, et al. The significance of elevated brain natriuretic peptide levels in chronic obstructive pulmonary disease. J Int Med Res 2005;33:537-44. [Crossref] [PubMed]
- Nagaya N, Ando M, Oya H, et al. Plasma brain natriuretic peptide as a noninvasive marker for efficacy of pulmonary thromboendarterectomy. Ann Thorac Surg 2002;74:180-4. [Crossref] [PubMed]


