The usefulness of Wi-Fi based digital chest drainage system in the post-operative care of pneumothorax
Introduction
After thoracic surgery, chest tubes are essential for drainage of air and fluid from the pleural cavity. Recently digital drainage systems have been developed and these systems facilitate the patients to ambulate without attached to wall suction and also make it easy for physicians to decide when to remove tubes objectively (1). Digital monitoring systems reduced hospital stay and medical expenses (2,3). But with these advantages over traditional drainage systems, physicians still visit the patients to confirm the state of chest drainage systems. With combination of wireless internet device, monitoring of digital data and controlling suction power are possible in real time without seeing the patients (4). The aim of this study is to apply the Wi-Fi (Wireless-Fidelity) based drainage system to patients in the course of postoperative care after thoracic surgery and to compare the efficacy of this digital drainage system.
Materials and methods
Patients and data collection
Patients eligible for this pilot study were those who underwent wedge resection of lung by video assisted thoracoscopic surgery (VATS) for spontaneous pneumothorax from January, 2012 to September, 2013 in Eulji University Hospital, Daejeon, Korea. Inclusion criteria were primary spontaneous pneumothorax with recurrence or prolonged air leak more than five days. We excluded secondary pneumothorax due to emphysema, tuberculosis and other causes such as trauma or inherited disease in this study. We inserted 12 Fr. trocar tube first in patients with pneumothorax larger than 30%. We did not perform chemical or mechanical pleurodesis before and during the operation. A single 28 Fr. chest tube was placed inside the thoracic cavity at the end of the procedure. After surgery, the patients were randomized 1:1 to apply two different types of chest drainage systems. Group I (study) consisted of digital chest drainage system (iPRUM, IVAI, Seoul. Korea) while in group II (control), conventional underwater-seal chest bottle system was used. It was approved by the institutional review board (IRB) of the Eulji University Hospital (2011-MDR-003). All patients had provided written informed consent before surgery when they matched to inclusion criteria. In all cases, we applied −20 cmH2O suction power until removal of the tubes. Chest tubes were removed when there was no air leak with less than 20 cm fluctuation of bottle line in traditional system without suction. In digital drainage system, when there was no leakage more than six hours at the monitor, then we removed. Questionnaire was given to study group to check usefulness of the device.
Technology
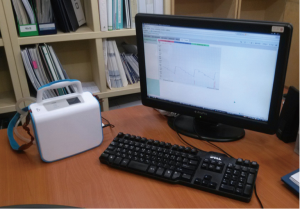
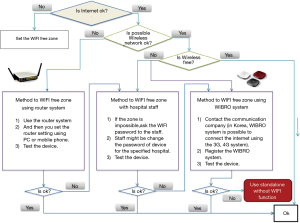
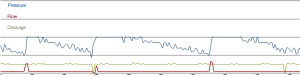
In the Wi-Fi (Wireless-Fidelity) based drainage system (iPRUM, IVAI, Seoul. Korea), suction pressure is controlled from 0 to −30 cmH2O using by the installed vacuum pump (Thomas diaphragm pump). Minimum and maximum value of suction pressure can be changed per 1 cmH2O unit controlled by the smart phone, the personal computer or remote controller (Figure 1). The measured data of the pressure value (mmH2O), air leakage volume and drainage volume (mL) were saved in real time by the pressure sensor (Digi-key, MPXV6115VC6U), the flow sensor (Siago, FSG4003-5LPM) and infrared sensor (Sharp, GP2Y0A41SK0F, reliability range 90%) and the data is transferred through internet server system to the physicians in real time and the physician can monitor all patients’ data and decide when to remove at the same time (Figure 2). In Figure 2, the blue, red, green line is respectively represented the pressure (mmHg), air-leakage flow (lpm) and the drainage volume (mL) in the instantaneous and history time monitor data. The medical staff can check patient’s instant and storage information and control the drainage system from the controller system. If Wi-Fi system is impossible, the patient’s data can be obtained by using the alternate method. Figure 3 demonstrates how to connect the internet system without WiFi system.
Statistical analysis
Data were analyzed using IBM SPSS Statistics20 for windows (IBM Software Group, Wacker Dr., Chicago, IL, USA). Numerical variables between the two groups of patients were compared with the student t-test (for normal distribution) and Mann-Whitney U-test (for other than normal distribution). Categorical data were analyzed by chi-square independence test. Two-sided P≤0.050 was considered statistically significant.
Results
Demography
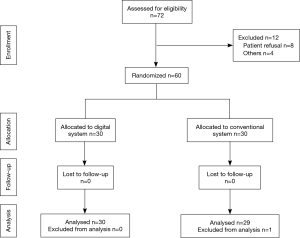
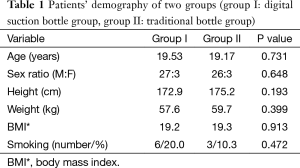
Seventy two patients were suitable for inclusion criteria during the period. Eight patients refused to be enrolled in the study and clinicians failed to enroll in another four patients. Of 72 patients, 60 patients were enrolled and 30 patients in each group (Figure 4). There were no significant differences in baseline characteristics between two groups such as age, height, weight, BMI (body mass index) and smoking history (Table 1). One patient was excluded from analysis because of postoperative pleurodesis due to prolonged air leak in group II (control group).
Full table
Pain and postoperative management
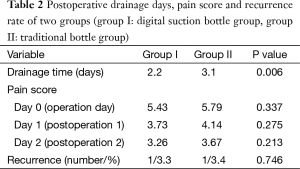
Pain was measured with visual analogue scale (VAS) scoring system. We used intravenous pain medication on the day of operation and oral medication was allowed from the following day. No patients received epidural analgesia. There was no significant difference between two groups in pain. Duration of tube was 2.2 days in group I and 3.1 in group II. Tube duration days were significantly shorter in group I than in group II (P=0.006). There were no complications before discharge and after one month follow-up. Two patients were found minimal pneumothorax during six months follow-up (one patient in each group), however, the amount of pneumothorax were minimal and they were resolved spontaneously during follow-up (Table 2).
Full table
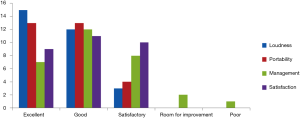
Questionnaire survey
Survey was done in group I (study group). All patients in group I had experienced traditional drainage system before surgery so it was possible for them to compare between two systems. Contents of the survey were composed of four questions; loudness of digital system compared to traditional system during daily activity and sleep, portability of the digital system compared to traditional system during exercise, easiness to control of digital system compared to traditional system, and the overall satisfaction compared to traditional system. Categories were graded by such as; excellent, good, satisfactory, room for improvement and poor. They felt that using digital system was more than satisfactory in loudness and portability but two patients answered that there was room for improvement in the device and one patient answered that using the new device was difficult to be managed (Figure 5).
Discussion
Chest tubes are inserted to drain the pleural cavity of air and fluid in various situations. Underwater-seal traditional system has been used in worldwide. It is composed of underwater-seal container, connector line to chest tube and allows one way movement of air and liquid from the pleural cavity. Care should be taken to fill the chamber to the marked water level and to connect the line to underwater-seal column. It is difficult to transport a patient with traditional chest tube because container bottle should be remained upright all the time. Sometimes fatal errors are committed by nurses or junior clinicians during these procedures. To deal with traditional bottle system, much time and effort should be given to educate and train nurses (5,6). Underwater-seal system also restricts patients to ambulate or to do daily activity. For clinicians, to remove the chest tube, there is no objective data so it is difficult to decide when to remove. So this system cannot fit the evidence based approach of managing patients with chest tubes.
Vital signs such as heart rate, respiration rate and arterial pressure, body temperature, oxygen saturation, and electrocardiogram can be monitored in the intensive care unit or bedside currently in real time. Recently it is more familiar for physicians using digitalized data to decide the patient’s condition than using analogue or subjective data. In the chest drainage system, such a change has begun. Data of the first digital detection device on air-leaks were published in 2006 (7). It was bed-side air-flow metry and should be connected to chest tube to measure air-leaks for about 10–15 minutes. In this study, they could detect minor air-leaks in cases presumed to have none by visual assessment. They also emphasized the possibility of evidence-based algorithm for the evaluation and treatment of air-leaks. Air-flowmety within chest drainage system was invented and it could display the measurement of air-leaks and pleural pressures over time (8). Clinicians could utilize objective data of air-leaks and intrapleural pressures in determining the time of removal with these systems. But on the point of patients, there was no improvement in daily activities with these systems because patients still stayed in bed to connect negative pressure suction pump. Ambulation is an important part of physiotherapy as a post-operative care in thoracic surgery patients.
Not only digitalized sensor detecting air leaks, but also suction pump being built in the bottle system was invented after those progressions (9). A single chamber device without liquid column allowed the patients to move freely or use conveniences because no suction line is needed in this system. There is a debate on suction in postoperative care of thoracic surgery patients (10,11), but still negative suction plays important role in the chest bottle management in reducing pleural cavity and expanding lung. This system also will reduce infection risk particularly if patients disconnect themselves to mobilize leaving the suction tube on the floor and reattach to the drain (9). This system shortened the duration of drainage, the length of hospital stay and eventually saved overall hospitalization cost in patients with pneumothorax (3). Recently in large multicenter international clinical trial, this system showed shorter air leak duration and higher satisfaction scores compared with patient with traditional devices (12).
Even if air-flow metry and suction pump are in drainage bottle system, patients still stay at hospital because physicians cannot monitor and control drainage system in real time. Another model of remote control of suction power and monitoring of air leak enabled the physicians to change suction power at the desired level without visiting a patient (4). Before this report, the patients with prolonged air leak have been discharged with various Heimlich valve type devices in many reports (13-15), but physicians could not know the changes of pleural cavity before their visiting and evaluation of bottle system.
In our study, we used Wi-Fi based drainage bottle system (iPRUM, IVAI, Seoul, Korea). Wi-Fi is a local area wireless technology that allows an electronic device to exchange data or connect to the internet. But free Wi-Fi was not always available, we used WiBro 4G egg (Olleh, KT, Korea) modem to connect Wi-Fi system. It was stuck to the bottle system, so controlling the system and collecting data were always possible. Multiple factors such as appearance of effusion drainage, characteristics of air leakage, and general condition also will affect postoperative duration of chest bottle, hospital stay and cost. To reduce such postoperative parameters, we chose the patients of primary pneumothorax because air leakage is the only factor when to remove chest tube. In our study, we found an advantage in hospital stay in digital drainage system comparing traditional system. In survey of the questionnaire, using digital drainage system made patients more comfortable than traditional system in loudness, portability and daily management of the tube. Only one patient said that managing device gave him some trouble but most of patients gave positive response in the field of managing tube. It means that young patients were easily adjusted to the new system because recently electronic equipment spread widely, so they are familiar with digitalized gadget. In this pilot study, we wanted to check the stability of our system, so we used this system only in the hospital without discharge. There were no significant technical problems during our study.
Recently advanced telecommunication devices have been applied in health care so rapidly and especially in respiratory field, home pulmonary function monitoring have shown a meaningful and cost-effective outcomes (16,17). In thoracic surgical area, internet-based digital drainage system will make rapid discharge and benefit in reducing cost possible. There are some risks in management of emergency situation like disconnection or malfunction of the device, so intermediate step maybe needed before home discharge. An affiliated health care system (i.e., hospices, dedicated guest houses) may provide the necessary networking and basic expertise (i.e., nonspecialized medical personnel) for clinical supervision in the event of emergency (4). There is still some limitation to apply this system, but internet based digital drainage system could be good method in thoracic telemedicine area in the near future.
Conclusions
Digital system was beneficial on reducing the length of tube drainage by real time monitoring. It also had advantage in portability, loudness and gave more satisfaction than conventional system when reviewing results of the questionnaire. Moreover internet based digital drainage system will be a good option in thoracic telemedicine area in the near future.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Cerfolio RJ, Varela G, Brunelli A. Digital and smart chest drainage systems to monitor air leaks: the birth of a new era? Thorac Surg Clin 2010;20:413-20. [Crossref] [PubMed]
- Brunelli A, Salati M, Refai M, et al. Evaluation of a new chest tube removal protocol using digital air leak monitoring after lobectomy: a prospective randomised trial. Eur J Cardiothorac Surg 2010;37:56-60. [Crossref] [PubMed]
- Jablonski S, Brocki M, Wawrzycki M, et al. Efficacy assessment of the drainage with permanent airflow measurement in the treatment of pneumothorax with air leak. Thorac Cardiovasc Surg 2014;62:509-15. [PubMed]
- Rocco G. Remote-controlled, wireless chest drainage system: an experimental clinical setting. Ann Thorac Surg 2013;95:319-22. [Crossref] [PubMed]
- Lehwaldt D, Timmins F. Nurses' knowledge of chest drain care: an exploratory descriptive survey. Nurs Crit Care 2005;10:192-200. [Crossref] [PubMed]
- Charnock Y, Evans D. Nursing management of chest drains: a systematic review. Aust Crit Care 2001;14:156-60. [Crossref] [PubMed]
- Anegg U, Lindenmann J, Matzi V, et al. AIRFIX: the first digital postoperative chest tube airflowmetry--a novel method to quantify air leakage after lung resection. Eur J Cardiothorac Surg 2006;29:867-72. [Crossref] [PubMed]
- Dernevik L, Belboul A, Rådberg G. Initial experience with the world's first digital drainage system. The benefits of recording air leaks with graphic representation. Eur J Cardiothorac Surg 2007;31:209-13. [Crossref] [PubMed]
- Rathinam S, Bradley A, Cantlin T, et al. Thopaz Portable Suction Systems in Thoracic Surgery: an end user assessment and feedback in a tertiary unit. J Cardiothorac Surg 2011;6:59. [Crossref] [PubMed]
- Sanni A, Critchley A, Dunning J. Should chest drains be put on suction or not following pulmonary lobectomy? Interact Cardiovasc Thorac Surg 2006;5:275-8. [Crossref] [PubMed]
- Deng B, Tan QY, Zhao YP, et al. Suction or non-suction to the underwater seal drains following pulmonary operation: meta-analysis of randomised controlled trials. Eur J Cardiothorac Surg 2010;38:210-5. [Crossref] [PubMed]
- Pompili C, Detterbeck F, Papagiannopoulos K, et al. Multicenter international randomized comparison of objective and subjective outcomes between electronic and traditional chest drainage systems. Ann Thorac Surg 2014;98:490-6; discussion 496-7. [Crossref] [PubMed]
- McKenna RJ Jr, Fischel RJ, Brenner M, et al. Use of the Heimlich valve to shorten hospital stay after lung reduction surgery for emphysema. Ann Thorac Surg 1996;61:1115-7. [Crossref] [PubMed]
- Lodi R, Stefani A. A new portable chest drainage device. Ann Thorac Surg 2000;69:998-1001. [Crossref] [PubMed]
- Jenkins WS, Hall DP, Dhaliwal K, et al. The use of a portable digital thoracic suction Thopaz drainage system for the management of a persistent spontaneous secondary pneumothorax in a patient with underlying interstitial lung disease. BMJ Case Rep 2012;2012.
- Izbicki G, Abboud S. Telespirometry for home monitoring of pulmonary function. J R Soc Med 1999;92:154-5. [PubMed]
- Cooper CB. Respiratory applications of telemedicine. Thorax 2009;64:189-91. [Crossref] [PubMed]