Follow-up of hypertension after aortic coarctation stent implantation based on safe and effective re-intervention: a retrospective cohort study
Introduction
Aortic coarctation (CoA) is a relatively common congenital heart disease. The incidence of CoA in live birth infants is approximately 0.04%, and it accounts for 5–8% of all cases of congenital heart disease (1,2). In 1944, the surgical correction of CoA was performed for the first time by Crafoord in Sweden (3). In the subsequent 40 years, there have been significant improvements in the surgical technology, and the cure rate of CoA has increased significantly (4). Balloon angioplasty was conducted in 1982. In the early 1990s, stent implantation was performed, which reduced the frequency of disruption of the aortic wall and significantly decreased the rate of complications (5,6).
However, despite the optimization of treatment, hypertension is still a common complication of CoA repair. Even if postoperative restenosis is relieved, patients can still develop hypertension. Depending on the age and follow-up duration, the incidence of postoperative hypertension ranges from 25% to 45% (7-11). As a result of hypertension, the long-term incidence of coronary atherosclerotic heart disease (coronary heart disease), stroke, rupture of the aorta and cerebral aneurysm, heart failure and sudden cardiac death in patients after CoA repair is high (12).
The existence of residual obstruction is a main basis for hypertension, however, many patients with hypertension have no signs of restenosis. Therefore, the possible cause of hypertension in this population remains the main issues of discussed. Abnormal aortic arch geometry, particularly a hypoplastic or gothic arch, has been reported to be associated with hypertension (9). In addition, the presence of a generalised vasculopathy, decreased aortic wall compliance, impaired baroreceptor sensitivity and altered blood flow patterns have been considered as susceptibility factors for persistent hypertension (13-15).
Currently, stent implantation is the main treatment for CoA, which can effectively reduce the aortic gradient with pleasant anatomical results. However, there remains uncertainty about the later impact of stenting on blood pressure and adverse events of cardiovascular disease. Up to now, only a limited number of studies have been conducted on the long-term follow-up after aortic stenting. In addition, very few case series that focused on aortic stents included ≥50 patients.
In this study, all patients with native CoA and recurrent CoA treated with stent implantation at the German Pediatric Heart Centre from 2004 to 2012 were followed up with until 2017 to evaluate the occurrence of hypertension and analyze the factors related to hypertension, for hypertension prevention and risk prediction. As residual stenosis and restenosis, which is a clear cause of hypertension, after CoA treatment can cause hypertension, in our study, patients with restenosis were re-subjected to the intervention to alleviate restenosis and rule out hypertension due to this cause. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1134/rc).
Methods
Study subjects
We conducted a retrospective analysis of the early- and long-term outcomes (with a follow-up period of 12 years) among all patients with stent implantation for CoA at the German Pediatric Heart Centre between January 2004 and September 2012. There were 88 consecutive patients included in this study, including patients with native CoA and recurrent CoA after surgery, simple CoA (without other cardiac malformations) and complex CoA (with other cardiac malformations).
The data about all patients who underwent transcatheter stent implantation, including demographics, systemic blood pressure (BP), diagnosis, echocardiographic examinations, interventional procedural data and angiographic images were retrospectively collected from patients’ archived records.
Because of the retrospective design, informed consent was waived. The requirement for ethical approval was waived by the ethics committee of the Asklepios Clinic Sankt Augustin, because this study used anonymised retrospective data. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Indications and exclusion criteria
The indications for stent implantation were: a transcatheter peak systolic pressure gradient of >20 mmHg and/or aortic narrowing >50% on angiography.
Patients were excluded from the study if they met any of the following exclusion criteria: (I) had a narrow segment that was too long for stent implantation; and/or (II) required a palliative stent.
Stent implantation
For all the interventions, the patients were placed under deep sedation with general anesthesia and endotracheal intubation. Vascular access was obtained from the right femoral artery, except for a few patients with complex congenital heart disease, such as hypoplastic left heart syndrome, in whom one femoral venous line was obtained. The catheter was placed on the ascending aorta and withdrawn across the narrowing segment, the pressure gradient across the coarctation was recorded, and angiography was performed. The stent dimension was selected according to the diameter of the distal transverse arch and descending aorta above the diaphragm at maximum expansion. The stents included Osypka Baby Stent, Palmaz Genesis Stent (Cordis), Numed CP Stent (both covered and not covered) and Atrium stent.
Moreover, aspirin was administered to children (2–3 mg/kg) and adults (100 mg) daily for 6 months.
Follow-up
The patients were clinically followed up at 1, 3 and 6 months after the intervention; subsequently, they were followed up every year. The follow-up examination included arm and leg BP measurements, chest radiography, standard echocardiography, and electrocardiography.
A full baseline echocardiographic examination was performed. The protocol includes parasternal long-axis, parasternal short-axis and apical 4-chamber views, acquired in the light of published guidelines.
Continuous-wave Doppler techniques were used to measure maximum peak systolic blood flow velocity at the former coarctation site or stented aorta, and peak gradients were recorded. Diastolic run-off was defined as a continuous forward flow throughout the whole diastole.
Follow-up data were obtained from the pediatric cardiac clinic or other specialized centers via fax or letter.
Patients with the following findings were scheduled for a catheter examination: (I) a brachial-ankle systolic BP (SBP) gradient >20 mmHg; (II) systemic arterial hypertension; and (III) maximum blood flow velocity at the former stent site >3 m/s or the presence of diastolic run-off in the descending aorta. Additionally, all growing children, underwent a catheter examination 3 years after the stent placement.
If invasively measured gradients were found across the stented area, balloon dilatation or stenting was performed.
BP measurements and hypertension diagnosis
Resting BP was measured in the extremities before cardiac catheterisation and after the intervention, as well as at each follow-up examination before physician review. BP was measured using an automatic oscillometric device (CARESCAPE V100 Monitor, General Electric Company) after at least 5 min of rest in the supine position. The extremities were measured to ensure the proper cuff size. The mean of at least 3 measurements of SBP, diastolic BP (DBP), pulse pressure, and brachial-ankle SBP gradient were used as the casual BP measurement. In adults, hypertension was defined as SBP ≥140 mmHg and/or DBP ≥90 mmHg, and in children, it was defined as the mean SBP and/or DBP ≥ the 95th percentile for sex, age and height on at least 3 separate occasions (16). Patients were considered normotensive if they did not use anti-hypertensive drugs or presented with no current hypertension according to the BP measurement at the last follow-up examination.
Patients with hypertension were treated with anti-hypertensive drugs. The following anti-hypertensive drugs were commonly used: β-receptor blockers, angiotensin II inhibitors [angiotensin-converting enzyme inhibitors (ACEIs)], angiotensin II receptor antagonists (ARBs), calcium channel blockers, and diuretics. The patients were treated with 1–4 anti-hypertensive drugs according to their condition.
Statistical analysis
The normally distributed continuous data are expressed as the mean ± standard deviation and the non-normally distributed data are expressed as the median (range). The differences between pre-intervention and follow-up were compared using a paired bilateral t-test or non-parametric test (Wilcoxon rank test). The risk factors for hypertension were analysed using Cox regression analysis, an estimated odds ratio, and the 95% confidence interval. A P value <0.05 was considered to indicate a statistically significant difference. All reported P values are two-sided. Statistical analysis was accessed by SPSS (version 15.0).
Results
Characteristics of the study population
The demographic data and diagnoses of the patients are summarized in Table 1.
Table 1
| Characteristics | Values (n=82) |
|---|---|
| Male sex, n (%) | 53 (64.6) |
| Age, median (range) | 123 months (40 days–44 years) |
| Weight (kg), median (range) | 36.5 (3.6–98.0) |
| Hypertension | 72 (87.8) |
| Age group, n (%) | |
| 0–5 years | 19 (23.2) |
| 6–10 years | 23 (28.0) |
| 11–15 years | 24 (29.3) |
| ≥16 years | 16 (19.5) |
| Diagnose, n (%) | |
| Simple CoA | 49 (59.8) |
| Complex CoA | 33 (40.2) |
| VSD | 5 |
| VSD + arch hypoplasia | 3 |
| AVSD | 1 (Down syndrome) |
| Arch hypoplasia | 3 |
| Left heart obstruction | 5 (1 Shone syndrome) |
| Supra-AV stenosis and LPA stenosis | 1 (Williams syndrome) |
| LPA and RPA stenosis | 1 (Williams syndrome) |
| TOF | 1 |
| TGA | 2 |
| DORV | 3 |
| SV repair (including HLHS) | 8 |
| Native CoA, n (%) | 37 (45.1) |
| Recurrent CoA, n (%) | 45 (54.9) |
CoA, coarctation; VSD, ventricular septal defect; AVSD, atrioventricular septal defect; AV, aortic valve; LPA, left pulmonary artery; RPA, right pulmonary artery; TOF, tetralogy of Fallot; TGA, transposition of the great arteries; DORV, double outlet right ventricle; SV, single ventricle; HLHS, hypoplastic left heart syndrome.
Intervention
A total of 87 stents were implanted in 82 patients. Due to a long stenosis segment or stent displacement, 5 patients were implanted with 2 stents, and all the remaining patients were implanted with 1 stent.
Based on aortography measurements before and after the intervention, the ratio of CoA diameter to diameter at the diaphragm level increased from 0.51 (0.12–0.86) to 1.00 (0.90–1.75); this value was significantly higher than that before treatment (P<0.001).
The invasive peak systolic gradient after the intervention was significantly reduced from an average of 28±12 to 7±6 mmHg after the intervention (P<0.001).
Follow-up
The average follow-up duration was 76.7 months (range, 6–151 months). One patient (1.2%) died and 5 patients were lost during the follow-up period. Ultimately, 82 patients were enrolled in this study.
Restenosis and re-intervention
During the follow-up period, catheterisation was scheduled for 65 patients; moreover, re-dilatation was required 103 times, and a second stent implantation was required 13 times. For these patients, 13 second stent implantations and 15 new stents were used. During the last follow-up, 17 (20.7%) of the 82 patients (11 men and 6 women) had not received interventional therapy, whereas 33 (40.2%), 18 (22.0%) and 14 (17.1%) had received interventional therapy 2, 3 and ≥4 times respectively (see Table 2). The most frequent indications for re-dilation were a residual gradient >10 mmHg, and/or a relative narrowing within the stent of ≥20%. As shown in Table 2, the younger the age at stent implantation, the higher the number of interventions performed.
Table 2
| Interventions | Age median (months) | Age min. (months) | Age max. (months) |
|---|---|---|---|
| Total (n=82) | 115.17 | 1.32 | 528.89 |
| 1 (n=17, 20.7%) | 187.24 | 107.54 | 425.92 |
| 2 (n=33, 40.2%) | 124.86 | 4.13 | 330.12 |
| 3 (n=18, 22.0%) | 66.05 | 1.32 | 528.89 |
| 4 or more (n=14, 17.1%) | 48.50 | 2.61 | 194.31 |
Min., minimum; max., maximum.
Complications of intervention
In total, 198 interventions included initial stent implantation, balloon dilatation and stent re-implantation. Complications occurred in 6 (3.0%) patients. Aortic aneurysms occurred in 3 patients. Among these 3 patients, the aortic aneurysms occurred during the stent implantation in 1 patient and during the balloon expansion at the follow-up examinations in 2 patients. These patients were treated with covered stent implantation. In 1 case, the stent migrated to the distal part; it was then inflated in the abdominal aorta and remained in place. Another stent was successfully implanted at the coarctation. The other 2 patients had pseudoaneurysms of the femoral artery, which were treated with surgical resection.
Hypertension
Overall, 72 (87.8%) patients were diagnosed with hypertension before treatment, and only 23 (28.0%) patients were diagnosed with hypertension at the last follow-up, which is a number significantly lower than that before the intervention (P<0.001).
Hypertension was diagnosed in 11 (of 37 patients, 29.7%) in the native CoA groups, 12 (of 45 patients, 26.7%) in the recurrent CoA groups; 15 of 49 (30.6%) in the simple CoA group, 8 of 33 (24.2%) in the complex CoA groups at the last follow-up.
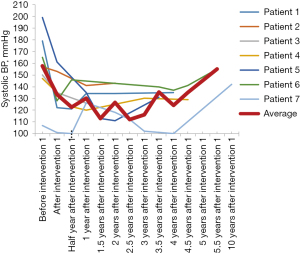
At the last follow-up, in the 0–5 years age group, 3 of 19 patients had hypertension; in the 6–10 years age group, 6 of 23 patients had hypertension; in the 11–15 years age group, 8 of 24 patients had hypertension; and in the ≥16 years age group, 6 of 16 patients had hypertension (15.8%, 26.1%, 33.3% and 37.5%, respectively). The comparison results in terms of the incidence of hypertension between the first stent implantation and the latest follow-up for the four age groups are shown in Figure 1.
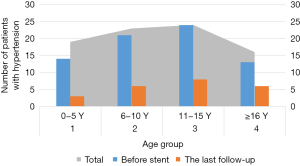
On multivariable Cox analysis, the diagnosis (simple CoA or complex CoA) and age at stenting were associated with the last follow-up hypertension (odds ratio 4.01, 95% confidence interval: 1.30–12.41, P=0.016; and odds ratio 1.81, 95% confidence interval: 1.15–2.84, P=0.01; respectively; see Table 3). The younger the age at the first stent implantation, the lower the incidence of hypertension during the follow-up (see Tables 3).
Table 3
| Variables | β | P | OR (95% CI) |
|---|---|---|---|
| Native or recurrent CoA | −0.886 | 0.085 | 0.412 (0.151, 1.129) |
| Simple or complex CoA | 1.077 | 0.044 | 2.935 (1.032, 8.347) |
| Age | 0.653 | 0.003 | 1.921 (1.241, 2.975) |
OR, odds ratio; CI, confidence interval; CoA, coarctation.
Anti-hypertensive medication
Overall, 23 patients with hypertension at the last follow-up were treated with anti-hypertensive agents as follows: 16 patients were treated with 1 agent (8: β-receptor blockers; 7: ACEIs and 1: ARBs), 4 patients were treated with 2 agents, 2 patients were treated with 3 agents, and 1 patient was treated with 4 agents. Finally, 12 patients (14.6%) were not satisfied with BP control during the follow-up period.
Standardized BP curve
To clarify the patient’s long-term changes in BP after stent implantation, standardized SBP curves were established. The standardized SBP of the children was calculated as their SBP divided by the normal SBP (in the 95th percentile for sex and age and height) multiplied by 140. The standardized SBP of adults was the actual BP of patients.
Each curve was classified according to the number of interventional treatments. As very few patients underwent >4 interventional treatments, only the curves for 1–3 interventional treatments were drawn (patients who did not attend regular follow-ups or with incomplete follow-up data were excluded).
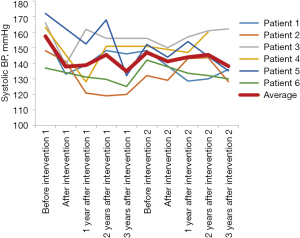
Figure 2 shows the follow-up SBP curve of patients who underwent the intervention. As shown in Figure 2, most patients had hypertension before the intervention and their BP significantly decreased after the stent implantation; moreover, most patients’ BP remained stable at the last follow-up. However, at the last follow-up, the BP of a few patients had increased.
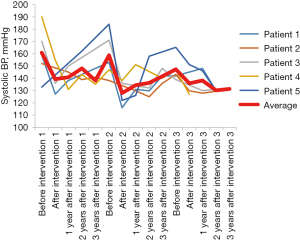
Figures 3,4 show the patients who received the intervention twice and thrice. Most patients had hypertension before treatment, and their BP decreased after treatment but increased again before the next treatment, and decreased after the intervention, which further confirmed that restenosis can cause hypertension. Subsequently, their BP decreased after treatment. Therefore, regular follow-ups and timely examinations are required in such patients to detect restenosis and conduct the treatment.
Discussion
Stents have been widely used in the treatment of native CoA and recurrent CoA after surgery. Stent implantation is minimally invasive and has a high success rate and low complication rate. This can be used instead of surgery among patients with appropriate anatomical conditions.
Recent studies found that hypertension is still extremely common in patients even after the complete elimination of the obstruction (17-19). Further, despite early catheter and surgical interventions, life expectancy continues to decline. Among patients who underwent CoA correction, hypertension was proven to be related to the occurrence of left ventricular hypertrophy. It is also an important risk factor for coronary events, stroke, rupture of aortic and cerebral aneurysms, heart failure, and sudden cardiac death (12).
Some studies have found that the incomplete relief of stenosis can lead to hypertension (20,21); thus, it is recommended that clinical and imaging evaluations of CoA should be conducted in a timely manner. Any obstruction that meets the intervention criteria should be resolved immediately. However, in clinical settings, it was found that a considerable number of patients with hypertension after coarctation repair had no residual obstruction (22). This highlights the complexity of the pathophysiology of paradoxical hypertension, which is related to various mechanisms, including abnormal aortic arch geometry (9,23,24), aortic arch dysplasia (10,25,26), changes in arterial function (27-29), overactivation of the renin-angiotensin system (30) and attenuation of the baroreflex (31,32).
Our study comprised patients who underwent stent implantation for CoA at the German Pediatric Heart Centre. The patients were regularly followed up after their stent implantations. During the follow-up examinations, the BP of 4 limbs was measured. Patients with restenosis were treated in time to relieve the stenosis and the residual obstructing factor was removed. At the last follow-up, 23 patients had hypertension.
To determine the incidence of hypertension after stent implantation, we analyzed age at the initial stent implantation, native or recurrent CoA after surgery, and simple or complex CoA. In between-group comparison, we found that the incidence of hypertension did not differ significantly between the native and recurrent CoA during the follow-up period. However, the incidence of hypertension in complex CoA was lower than that in simple CoA; this finding is consistent with the finding reported in Giordano’s study (33). In Giordano’s study, the subjects were patients who had undergone surgery, and we obtained the same results in patients with stent implantation. This suggests that the difference in the incidence of hypertension between the simple and complex CoA groups is not related to the type of surgical approach alone. Furthermore, we hypothesize that the lower rate of late hypertension in patients with complex CoA could be due to reduced stimulation of the baroreceptor reflex in the pre-stenotic area due to decreased systemic blood flow and pressure before the intervention, which is not true for patients with simple CoA, as previously shown (34,35).
We also found that the incidence of hypertension increased with age at the initial stent implantation. The Cox regression analysis revealed that age was the main factor affecting paradoxical hypertension after the intervention. Thus, consistent with the findings of other studies (13,18,36), we suggest that coarctation should be treated as soon as possible.
The administration of medication to patients with hypertension after coarctation repair can not only control BP but can also improve arterial stiffness, endothelial function, and ventricular stiffness. Commonly used anti-hypertensive drugs include β-receptor blockers, calcium channel blockers, thiazide diuretics and ACEIs. When a single-agent treatment is ineffective, 2 or more agents should be combined. In the present study, 23 patients used anti-hypertensive medications; of these, 11 patients were able to maintain normal BP after medication administration.
We drew the standardized curve of SBP. The BP of most patients who underwent the intervention once decreased after stent implantation, whereas the BP of patients who underwent the intervention twice or thrice decreased after the first intervention but increased after restenosis. After the next intervention, the BP decreased again with the disappearance of restenosis. This strongly supports the necessity of long-term follow-up, BP monitoring and timely detection of restenosis and treatment. However, after a period of being normotensive, a few patients’ BP increased again, but without restenosis. This further emphasizes the significance of long-term follow-up examinations. Hypertension needs to be detected at an appropriate time, and restenosis should be ruled out and anti-hypertensive medications should be started as soon as possible.
Stent implantation for CoA was first applied to adolescents and adults. As the metal stent is hard and cannot grow with the body, the sheath required for stent implantation in children is thicker for the femoral artery. Only permanent stents should be used in implantations for infants and young children. Recent stent designs allow for stents to gradually expand to an adult size in stages, and the maximum sized stent does not need to be implanted at the time of implantation (37,38). In our study, the stents used for the infants were the Osypka Baby Stent and Palmaz Genesis Stent (Cordis), including PG1910 and PG2910, and the stents used for the children and adults were the Palmaz 308, Numed CP, and Atrium. As children grow and develop, stent restenosis is common, and the stent may need to be re-expanded or a new stent may be needed. Our study found that the younger the age at stenting, the more re-interventions are required.
Among the 198 interventions, 6 patients developed complications (3.0%). Studies have proven that multiple balloon dilatation and stent implantation are safe and effective.
In our study, patients with hypertension complicated with restenosis underwent balloon dilatation or another stent placement to reduce the gradient. The remaining patients with hypertension were treated with anti-hypertensive drugs. Finally, 12 patients were dissatisfied with BP control (14.6%). We also found that the treatment of coarctation is a continuous process. Long-term regular follow-up examinations after treatment and BP monitoring and timely treatment are essential.
Limitations and additional statement
Regarding the treatment of CoA, surgery for infants and stent implantation for adults and adolescents are generally recommended. In our study, the age of patients at stent implantation was below the recommended standard. This was largely because the patients were not able to undergo surgery owing to cardiac insufficiency, serious complications or residual coarctation early after surgery and consent of the surgeons was obtained.
Conclusions
Hypertension in patients with CoA stent implantation involves a complex pathophysiological process. Early treatment of CoA could reduce the incidence of hypertension. Moreover, timely expansion of restenosis is necessary to control hypertension. CoA needs a long-term treatment process, which not only requires surgical or interventional treatment to relieve anatomical malformations but also the medication management of BP, thereby requiring lifelong follow-up examinations.
Acknowledgments
Funding: This study was funded by Tianjin Key Medical Discipline (Specialty) Construction.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1134/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1134/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1134/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Because of the retrospective design, informed consent was waived. The requirement for ethical approval was waived by the ethics committee of the Asklepios Clinic Sankt Augustin, because this study used anonymised retrospective data. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890-900. [Crossref] [PubMed]
- Baumgartner H, Bonhoeffer P, De Groot NM, et al. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J 2010;31:2915-57. [Crossref] [PubMed]
- Crafoord C, Nylin G. Congenital coarctation of the aorta and its surgical treatment. J Thorac Surg 1945;14:347-61. [Crossref]
- Victor S. Patch aortoplasty for coarctation of aorta: technical considerations. Ann Thorac Surg 1995;59:1276-8. [Crossref] [PubMed]
- Batlivala SP, Goldstein BH. Current Transcatheter Approaches for the Treatment of Aortic Coarctation in Children and Adults. Interv Cardiol Clin 2019;8:47-58. [Crossref] [PubMed]
- Magee AG, Brzezinska-Rajszys G, Qureshi SA, et al. Stent implantation for aortic coarctation and recoarctation. Heart 1999;82:600-6. [Crossref] [PubMed]
- Smith Maia MM, Cortês TM, Parga JR, et al. Evolutional aspects of children and adolescents with surgically corrected aortic coarctation: clinical, echocardiographic, and magnetic resonance image analysis of 113 patients. J Thorac Cardiovasc Surg 2004;127:712-20. [Crossref] [PubMed]
- Stewart AB, Ahmed R, Travill CM, et al. Coarctation of the aorta life and health 20-44 years after surgical repair. Br Heart J 1993;69:65-70. [Crossref] [PubMed]
- Ou P, Bonnet D, Auriacombe L, et al. Late systemic hypertension and aortic arch geometry after successful repair of coarctation of the aorta. Eur Heart J 2004;25:1853-9. [Crossref] [PubMed]
- Quennelle S, Powell AJ, Geva T, et al. Persistent Aortic Arch Hypoplasia After Coarctation Treatment Is Associated With Late Systemic Hypertension. J Am Heart Assoc 2015;4:001978. [Crossref] [PubMed]
- Sendzikaite S, Sudikiene R, Tarutis V, et al. Prevalence of arterial hypertension, hemodynamic phenotypes, and left ventricular hypertrophy in children after coarctation repair: a multicenter cross-sectional study. Pediatr Nephrol 2020;35:2147-55. [Crossref] [PubMed]
- Bondy CA. Aortic coarctation and coronary artery disease: the XY factor. Circulation 2012;126:5-7. [Crossref] [PubMed]
- Hager A, Kanz S, Kaemmerer H, et al. Coarctation Long-term Assessment (COALA): significance of arterial hypertension in a cohort of 404 patients up to 27 years after surgical repair of isolated coarctation of the aorta, even in the absence of restenosis and prosthetic material. J Thorac Cardiovasc Surg 2007;134:738-45. [Crossref] [PubMed]
- Morgan GJ, Lee KJ, Chaturvedi R, et al. Systemic blood pressure after stent management for arch coarctation implications for clinical care. JACC Cardiovasc Interv 2013;6:192-201. [Crossref] [PubMed]
- Meijs TA, Warmerdam EG, Slieker MG, et al. Medium-term systemic blood pressure after stenting of aortic coarctation: a systematic review and meta-analysis. Heart 2019;105:1464-70. [Crossref] [PubMed]
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004;114:555-76. [Crossref] [PubMed]
- Canniffe C, Ou P, Walsh K, et al. Hypertension after repair of aortic coarctation--a systematic review. Int J Cardiol 2013;167:2456-61. [Crossref] [PubMed]
- Bocelli A, Favilli S, Pollini I, et al. Prevalence and long-term predictors of left ventricular hypertrophy, late hypertension, and hypertensive response to exercise after successful aortic coarctation repair. Pediatr Cardiol 2013;34:620-9. [Crossref] [PubMed]
- Choudhary P, Canniffe C, Jackson DJ, et al. Late outcomes in adults with coarctation of the aorta. Heart 2015;101:1190-5. [Crossref] [PubMed]
- Rinnström D, Dellborg M, Thilén U, et al. Poor blood pressure control in adults with repaired coarctation of the aorta and hypertension: a register-based study of associated factors. Cardiol Young 2017;27:1708-15. [Crossref] [PubMed]
- Lee MGY, Allen SL, Koleff J, et al. Impact of arch reobstruction and early hypertension on late hypertension after coarctation repair. Eur J Cardiothorac Surg 2018;53:531-7. [Crossref] [PubMed]
- Lee MG, Allen SL, Kawasaki R, et al. High Prevalence of Hypertension and End-Organ Damage Late After Coarctation Repair in Normal Arches. Ann Thorac Surg 2015;100:647-53. [Crossref] [PubMed]
- Ou P, Mousseaux E, Celermajer DS, et al. Aortic arch shape deformation after coarctation surgery: effect on blood pressure response. J Thorac Cardiovasc Surg 2006;132:1105-11. [Crossref] [PubMed]
- De Caro E, Trocchio G, Smeraldi A, et al. Aortic arch geometry and exercise-induced hypertension in aortic coarctation. Am J Cardiol 2007;99:1284-7. [Crossref] [PubMed]
- Giardini A, Piva T, Picchio FM, et al. Impact of transverse aortic arch hypoplasia after surgical repair of aortic coarctation: an exercise echo and magnetic resonance imaging study. Int J Cardiol 2007;119:21-7. [Crossref] [PubMed]
- Ntsinjana HN, Biglino G, Capelli C, et al. Aortic arch shape is not associated with hypertensive response to exercise in patients with repaired congenital heart diseases. J Cardiovasc Magn Reson 2013;15:101. [Crossref] [PubMed]
- de Divitiis M, Pilla C, Kattenhorn M, et al. Ambulatory blood pressure, left ventricular mass, and conduit artery function late after successful repair of coarctation of the aorta. J Am Coll Cardiol 2003;41:2259-65. [Crossref] [PubMed]
- Brili S, Tousoulis D, Antoniades C, et al. Evidence of vascular dysfunction in young patients with successfully repaired coarctation of aorta. Atherosclerosis 2005;182:97-103. [Crossref] [PubMed]
- Menon A, Eddinger TJ, Wang H, et al. Altered hemodynamics, endothelial function, and protein expression occur with aortic coarctation and persist after repair. Am J Physiol Heart Circ Physiol 2012;303:H1304-18. [Crossref] [PubMed]
- Parker FB Jr, Streeten DH, Farrell B, et al. Preoperative and postoperative renin levels in coarctation of the aorta. Circulation 1982;66:513-4. [Crossref] [PubMed]
- Igler FO, Boerboom LE, Werner PH, et al. Coarctation of the aorta and baroreceptor resetting. A study of carotid baroreceptor stimulus-response characteristics before and after surgical repair in the dog. Circ Res 1981;48:365-71. [Crossref] [PubMed]
- Johnson D, Perrault H, Vobecky SJ, et al. Resetting of the cardiopulmonary baroreflex 10 years after surgical repair of coarctation of the aorta. Heart 2001;85:318-25. [Crossref] [PubMed]
- Giordano U, Chinali M, Franceschini A, et al. Impact of complex congenital heart disease on the prevalence of arterial hypertension after aortic coarctation repair. Eur J Cardiothorac Surg 2019;55:559-63. [Crossref] [PubMed]
- Beekman RH, Katz BP, Moorehead-Steffens C, et al. Altered baroreceptor function in children with systolic hypertension after coarctation repair. Am J Cardiol 1983;52:112-7. [Crossref] [PubMed]
- Kenny D, Polson JW, Martin RP, et al. Relationship of aortic pulse wave velocity and baroreceptor reflex sensitivity to blood pressure control in patients with repaired coarctation of the aorta. Am Heart J 2011;162:398-404. [Crossref] [PubMed]
- Meadows J, Minahan M, McElhinney DB, et al. Intermediate Outcomes in the Prospective, Multicenter Coarctation of the Aorta Stent Trial (COAST). Circulation 2015;131:1656-64. [Crossref] [PubMed]
- Boe BA, Armstrong AK, Janse SA, et al. Percutaneous Implantation of Adult Sized Stents for Coarctation of the Aorta in Children ≤20 kg: A 12-Year Experience. Circ Cardiovasc Interv 2021;14:e009399. [Crossref] [PubMed]
- Bambul Heck P, Fayed M, Hager A, et al. Sequential dilation strategy in stent therapy of the aortic coarctation: A single centre experience. Int J Cardiol 2021;331:82-7. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)