Significance of the evaluation of tracheal length using a three-dimensional imaging workstation
Introduction
The trachea is the central airway of the respiratory system, and tracheal disorders can lead to respiratory failure and death. The most common conditions to require tracheal resection and reconstruction (TRR) include tracheal stenosis, traumatic injury, and tumor (1). TRR is a challenging surgery for thoracic surgeons because of the relative rarity of tracheal diseases, technical difficulties, and the specific airway management necessary during surgery. It requires close cooperation with anesthesiologists and other medical staff.
Although TRR initially allowed for resection of just 2 cm of the trachea (2,3), it is considered possible to perform TRR of approximately 6 cm with tracheal mobilization procedures (4,5). On the other hand, TRR could even allow for resection of up to half of the trachea (6). Historically, previous clinical studies reported the resected absolute length of the trachea in TRR and failed to provide information on the pre-surgical length of the trachea in each case. The original tracheal length can be crucial in deciding on the resectable and reconstructible tracheal length in TRR. However, the individual differences and characteristics of tracheal length remain unclear.
Imaging technology is advancing rapidly and has provided detailed information on human anatomy. For example, multidetector computed tomography has allowed the reconstruction of three-dimensional (3D) images using different types of software, and several studies have reported the usefulness of preoperative simulation and intraoperative guidance in thoracic surgery (7-9). In addition, 3D imaging enables more precise and objective visualization of the spatial relationship of structures than two-dimensional (2D) imaging or cadaver specimens. Furthermore, it accurately reflects the actual anatomical structures of each patient. In this study, we measured tracheal length using a 3D imaging workstation and investigated the variations in tracheal length associated with several clinical parameters that could be useful for TRR planning. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-595/rc).
Methods
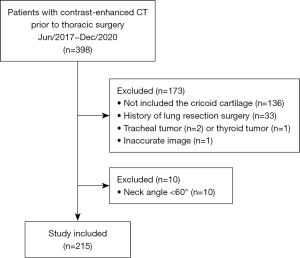
Between June 2017 and December 2020, we examined 398 patients who underwent contrast-enhanced computed tomography (CT) before thoracic surgery at Shinshu University Hospital, and 183 of them were excluded from this study. The exclusion criteria were as follows (Figure 1): images did not show the level of the cricoid cartilage, history of lung resection surgery, presence of a tracheal tumor, presence of a thyroid tumor that affected the shape of the trachea, and neck angle <60°, which appears to be the flexion position of the neck (10). This study finally enrolled the remaining 215 patients including those with primary lung cancer (n=159), metastatic lung tumor (n=28), thymic epithelial tumor (n=9), and others (n=19). Clinical data were collected from their electronic medical records. All patient data, including age, sex, height, and weight, were available, and body mass index (BMI) was calculated as weight (kg)/height (m)2. Body surface area (BSA) was calculated using the formula proposed by Fujimoto and Watanabe (11). We retrospectively investigated the association of these clinical characteristics with tracheal length. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This retrospective study was approved by the institutional review board of Shinshu University Hospital (Project ID, 4938), and we utilized an opt-out approach instead of obtaining written informed consent from each patient.
Image acquisition
During the study period, we used two types of CT scanners: Light Speed VCT Vision (GE Healthcare, USA) until December 2019, and revolution CT (GE Healthcare) from January 2020. The patients were maintained in the supine position with their arms above their heads and a towel, to add a little height, under their heads. They were asked to hold a deep breath during the scans. All contrast-enhanced 3D-CT examinations were performed using 0.63-mm-thick full-resolution scans at our institute. Collected data were transferred to a 3D imaging workstation (Ziostation2; Ziosoft, Japan).
Measurement of the neck angle and tracheal length
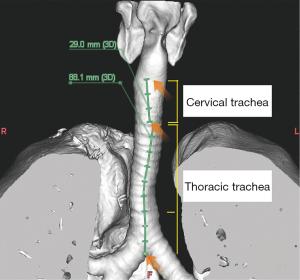
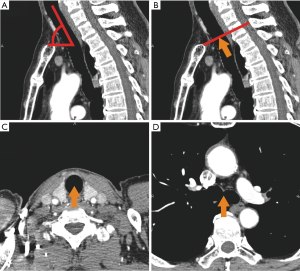
All variables were measured using a 3D imaging workstation (Figure 2). The total tracheal length was defined as the distance between the lower border of the cricoid cartilage and the carina. The neck angle was measured at an angle between an elongated horizontal line at the manubrium of the sternum and an elongated line at the center of the tracheal lumen in a sagittal view (Figure 3A). In the measurement of tracheal length, first, a point was marked at the center of the tracheal lumen on a vertical line from the jugular notch of the sternum to the cervical vertebrae, which was defined as the border between the cervical and thoracic trachea (Figure 3B). Then, in axial views, we marked two points at the center of the tracheal lumen: one at the lower border of the cricoid cartilage and the other at the carina (Figure 3C,3D). Subsequently, we traced the center of the tracheal lumen, which allowed measurements while accounting for the tracheal flexion, between these three points, and obtained the total, cervical, and thoracic tracheal lengths (Figure 4).
Statistical analysis
SPSS version 27 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. The normal distribution of the total tracheal length was analyzed using the Shapiro-Wilk test. All data are reported as mean ± standard deviation. Unpaired Student’s t-test was used to compare sex-related differences. Pearson’s correlation was used to analyze the relationship between tracheal length and physiological variables. Multiple linear regression analysis was performed to assess the independent predictors of the total tracheal length and cervical and thoracic tracheal lengths using common physiological parameters (age, sex, body height, and weight). Statistical significance was set at P<0.05.
Results
The overall distribution of the total tracheal length is depicted in Figure 5A, and it shows a normal distribution (P=0.2). The total tracheal length ranged from 8.8 to 14.4 cm (mean, 11.5±1; median, 11.5; interquartile range, 10.8–12.2 cm). In addition, 1.9% (n=4) and 8% (n=17) patients had a total tracheal length of <9 and <10 cm, which appeared to be short tracheal lengths, respectively (Figure 5).
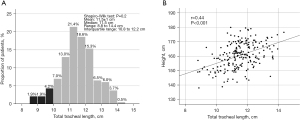
Table 1 shows the clinical characteristics of all patients; 108 men (mean age, 70±10 years) and 107 women (mean age, 67±13 years) were included. As expected, significant differences were found in height, weight, and BSA between men and women. The total trachea was significantly longer in men than in women (11.8±1.0 vs. 11.2±1.1 cm, P<0.001). The cervical trachea was significantly shorter in men than in women (2.9±1.3 vs. 3.8±1.3 cm, P<0.001), while the thoracic trachea was significantly longer in men than in women (8.9±1.1 vs. 7.4±1.1 cm, P<0.001). The ratio of the thoracic to cervical tracheal length was significantly higher in men than in women (P<0.001).
Table 1
| Variables | Total, N=215 |
Male, n=108 (50.2%) |
Female, n=107 (49.8%) |
P |
|---|---|---|---|---|
| Age, y | 68±11 | 70±10 | 67±13 | 0.047 |
| Height, cm | 161±9 | 167±6 | 154±7 | <0.001 |
| Weight, kg | 59±11 | 65±10 | 54±10 | <0.001 |
| BMI, kg/m2 | 23±3 | 23±3 | 23±3 | 0.12 |
| BSA, m2 | 1.6±0.2 | 1.7±0.1 | 1.5±0.1 | <0.001 |
| Neck angle, degree | 73±5 | 72±5 | 75±5 | <0.001 |
| Total tracheal length, cm | 11.5±1.1 | 11.8±1.0 | 11.2±1.1 | <0.001 |
| Cervical tracheal length, cm | 3.4±1.4 | 2.9±1.3 | 3.8±1.3 | <0.001 |
| Thoracic tracheal length, cm | 8.1±1.3 | 8.9±1.1 | 7.4±1.1 | <0.001 |
| Ratio of thoracic/cervical tracheal length | 3.4±3.5 | 4.4±4.0 | 2.4±2.4 | <0.001 |
Data are shown as number (%) or mean ± SD. BMI, body mass index; BSA, body surface area; SD, standard deviation.
The results of the correlation analysis between the physiological parameters and tracheal length are presented in Table 2, including the cervical and thoracic tracheal lengths. Age was significantly negatively correlated with the cervical tracheal length in both sexes (male, r=−0.37, P<0.001; female, r=−0.43, P<0.001) and positively correlated with the thoracic tracheal length (male, r=0.46, P<0.001; female, r=0.3, P<0.001). Height demonstrated a significant positive correlation with the total tracheal length in both sexes (Figure 5B; total, r=0.44, P<0.001; male, r=0.31, P<0.001; female, r=0.42, P<0.001). Height presented a significant positive correlation with the cervical tracheal length in both sexes (male, r=0.24, P=0.01; female, r=0.45, P<0.001), but no correlation with the thoracic tracheal length (male, r=−0.01, P=0.9; female, r=−0.14, P=0.2). Weight, BMI, and BSA exhibited various relationships with the tracheal length (Table 2). Although the total tracheal length had a significant positive correlation with the cervical and thoracic tracheal lengths in both sexes, the cervical tracheal length was more closely related to the total tracheal length than the thoracic tracheal length (cervical tracheal length: male, r=0.56, P<0.001; female, r=0.62, P<0.001; thoracic tracheal length: male, r=0.23, P=0.02; female, r=0.24, P=0.02). A significant negative correlation was found between the cervical and thoracic tracheal lengths in both sexes (male, r=−0.68, P<0.001; female, r=−0.61, P<0.001).
Table 2
| Variables | Total tracheal length | Cervical tracheal length | Thoracic tracheal length | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | ||||||||||||
| r | P value | r | P value | r | P value | r | P value | r | P value | r | P value | ||||||
| Age, y | 0.02 | 0.82 | −0.24 | 0.01 | −0.37 | <0.001 | −0.43 | <0.001 | 0.46 | <0.001 | 0.30 | <0.001 | |||||
| Height, cm | 0.31 | <0.001 | 0.42 | <0.001 | 0.24 | 0.01 | 0.45 | <0.001 | −0.01 | 0.9 | −0.14 | 0.2 | |||||
| Weight, kg | 0.02 | 0.8 | 0.16 | 0.1 | 0.03 | 0.8 | 0.04 | 0.7 | −0.02 | 0.8 | 0.11 | 0.3 | |||||
| BMI, kg/m2 | −0.14 | 0.15 | −0.06 | 0.5 | −0.09 | 0.4 | −0.23 | 0.02 | −0.02 | 0.8 | 0.21 | 0.03 | |||||
| BSA, m2 | 0.1 | 0.3 | 0.25 | 0.01 | 0.1 | 0.4 | 0.16 | 0.09 | −0.02 | 0.8 | 0.05 | 0.6 | |||||
| Cervical tracheal length, cm | 0.56 | <0.001 | 0.62 | <0.001 | – | – | – | – | −0.68 | <0.001 | −0.61 | <0.001 | |||||
| Thoracic tracheal length, cm | 0.23 | 0.02 | 0.24 | 0.02 | −0.68 | <0.001 | −0.61 | <0.001 | – | – | – | – | |||||
BMI, body mass index; BSA, body surface area; r, pearson correlation coefficient.
Table 3 summarizes the results of the multiple linear regression analyses of the total, cervical, and thoracic tracheal lengths using common physiological parameters (age, sex, height, and weight). Height and weight were significant independent predictors of the total tracheal length, and the contribution of height was greater than that of weight based on the standardized coefficients (height, β=0.69, P<0.001; weight, β=−018, P=0.03). In particular, height significantly contributed to the cervical tracheal length (cervical tracheal length, β=0.42, P<0.001; thoracic tracheal length, β=0.1, P=0.2). Age was an independent negative and positive contributor to cervical and thoracic tracheal lengths, respectively (cervical tracheal length, β=−0.29, P<0.001; thoracic tracheal length, β=0.37, P<0.001). Sex had the greatest contribution to the cervical and thoracic tracheal lengths (cervical tracheal length: male, β=−0.49, P<0.001; thoracic tracheal length: male, β=0.4, P<0.001). These results indicated that the male sex is a contributor to a shorter cervical trachea and longer thoracic trachea. Conversely, the female sex is a contributor to a longer cervical trachea and shorter thoracic trachea.
Table 3
| Variables | Total tracheal length (R2=0.22) | Cervical tracheal length (R2=0.32) | Thoracic tracheal length (R2=0.44) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | P value | B | SE | β | P value | B | SE | β | P value | |||
| Age, y | 0.009 | 0.007 | 0.09 | 0.2 | −0.035 | 0.008 | −0.29 | <0.001 | 0.04 | 0.007 | 0.37 | <0.001 | ||
| Sex, male | 0.3 | 0.207 | 0.14 | 0.15 | −1.36 | 0.254 | −0.49 | <0.001 | 1.06 | 0.219 | 0.4 | <0.001 | ||
| Height, cm | 0.083 | 0.014 | 0.69 | <0.001 | 0.07 | 0.017 | 0.42 | <0.001 | 0.02 | 0.015 | 0.1 | 0.2 | ||
| Weight, kg | −0.018 | 0.008 | −0.18 | 0.03 | −0.03 | 0.01 | −0.24 | 0.003 | 0.01 | 0.009 | 0.1 | 0.2 | ||
R2, coefficient of determination; B, unstandardized coefficients; SE, standard error; β, standardized coefficients.
Discussion
This study demonstrated that the mean total tracheal length was 11.5±1 cm, which is consistent with that of previous studies (4,12); however, the range varied widely from 8.8–14.4 cm. In our analysis of the relationship between tracheal length and physiological parameters, we found that physiological features differed depending on the parts of the trachea. This is the first study to focus on tracheal length using a 3D imaging workstation, encompassing normal physiological conditions in comparison with the conditions included in anatomical studies of formalin-fixed cadaver specimens. 3D imaging would be more accurate in a spatial evaluation than in multiplanar 2D imaging, since the tracheal length in this study was measured by tracing the center of the trachea without the influence of its meandering and kyphosis. Furthermore, our findings can be useful for TRR because the resectable tracheal length in TRR varies based on the tracheal length and characteristics of each patient.
As TRR is relatively rare and difficult, with complications that could lead to severe morbidities, it is a challenging procedure (13-15). In fact, one study reported that complications after TRR occurred in approximately 20% of cases, of which half were anastomotic complications (16). These anastomotic complications were associated with long-segment tracheal resection (13,16), wherein adequate tracheal release maneuvers should be considered to reduce tension along the suture line (17), including blunt dissection around the trachea, neck flexion, laryngeal release maneuver (18-20), and hilar release maneuvers (5). Therefore, preoperative estimation of an expected tracheal resection length in TRR should be considered to avoid postoperative anastomotic complications.
The techniques and knowledge of TRR have been gradually developed since the first tracheal resection, reported by Belsey in 1950 (3). Although Grillo et al. reported a mean resectable tracheal length of 6.4 cm (4), this study was performed using formalin-fixed cadaver specimens, which deviate from normal physiological conditions in unique procedures, such as the division of the left main bronchus with reimplantation into the right bronchus intermedius. Similarly, Madariaga et al. analyzed 545 patients who underwent TRR and reported that the mean resected tracheal length was 3.5 cm (range, 1–6.3 cm) with tracheal release maneuvers, and 3.0 cm (range, 0.8–6.5 cm) without tracheal release maneuvers (21). Interestingly, the patient who underwent only 1 cm of tracheal resection in the study required the tracheal release maneuver, whereas the patient with 6.5 cm of tracheal resection did not undergo the tracheal release maneuver. Although body habitus or kyphosis may be associated with tracheal mobility in tracheal reconstruction, these findings indicate that determining the total tracheal length in each case is necessary for discussing the resectable tracheal length. Conversely, it is believed that half of the trachea can be resected and reconstructed using tracheal maneuvers (6). However, we noted that 5 cm or more of tracheal resection in patients with a total tracheal length of <10 cm, which accounted for 8% of patients in this study (Figure 5A), equaled the removal of more than half of the trachea. Furthermore, the number of resected tracheal cartilage rings is another indicator in TRR (22), with the length of two rings considered to be 1 cm (23,24). Still, the number of tracheal cartilage rings also varies in individuals (mean, 19±3 cm); additionally, tracheal cartilage rings have various shapes, which are divided into 12 patterns (25). These findings indicate that the length of a tracheal cartilage ring varies depending on the total tracheal length, as well as the number and shapes of the tracheal cartilage rings. Without a proper preoperative assessment of the total tracheal length, the patient would experience critical anastomosis during TRR. As such, we should carefully determine the resectable tracheal length in each case by considering the total tracheal length, especially in patients with short tracheas.
A previous study reported that the total tracheal length was associated with the sex and height of patients (12). In this study, we found that height was the most independent contributor to the total tracheal length based on multiple linear regression. Some studies reported that all patients with postintubation tracheal rupture (PiTR) had a height of less than 165 cm, possibly indicating short stature as a predisposing factor for PiTR (26,27). Another study revealed that the endotracheal tube of patients with PiTR was positioned significantly more distantly in the already smaller trachea, which can be forced under by cuff overpressure (28). These findings may indicate that short stature increases the risk of PiTR, since patients with short statures are managed with distal positioning of the endotracheal tube due to their short tracheal length. However, although rare, there were cases wherein the trachea was extremely short relative to the patient height in this study (Figure 5B). Thus, when performing TRR and endotracheal intubation, it is important to consider the tracheal length of each patient. In addition, regarding the parts of the trachea, height only influenced the cervical tracheal length. Our study also revealed that older age significantly contributed to a shorter cervical trachea and longer thoracic trachea, which may result from a reduction in the strength of the annular ligament and fibrous tissue with aging. Furthermore, sex was the greatest independent contributor to cervical and thoracic tracheal lengths, wherein male sex was a predictor of a shorter cervical trachea and longer thoracic trachea, and female sex was a predictor of a longer cervical trachea and shorter thoracic trachea. Considering all these factors, characteristics of the trachea are shown to vary individually and biologically among patients, demonstrating the importance of measuring and identifying the tracheal features in each case.
Despite these findings, this study has certain limitations that need to be addressed. First, our data were collected from a small number of patients in a single institution, all of whom were Japanese. Second, we only conducted a case-control study of patients with non-diseased tracheas, which did not examine changes in physiological parameters over time, nor patients with a diseased trachea. Third, the influence of the neck angle, neck extension or flexion, and body habitus were not considered in this study. Fourth, our study was unable to demonstrate the superiority of 3D imaging measurement as we did not investigate the tracheal length using multiplanar 2D imaging. Similarly, we did not investigate the difference between 3D imaging and bronchoscopy measurement. Although bronchoscopy is a preoperative examination for TRR, measuring the tracheal length from the vocal cord to the carina using bronchoscopy is different from 3D imaging measurement (29). Last, the usefulness of data regarding the tracheal length in TRR remains unclear, since there are no data on the tracheal length of patients who underwent TRR. Further studies using accumulated data on the tracheal length in TRR are necessary to discuss and address this issue.
Conclusions
This study demonstrated the reference values and characteristics of tracheal length, including cervical and thoracic tracheal lengths, using a 3D imaging workstation. The total tracheal length ranged from short to long in individuals, and characteristics of tracheal length varied with height, age, sex, and part of the trachea. We should thus be aware of the tracheal length of each patient for appropriate tracheal management.
Acknowledgments
We would like to thank Otake for his support using a 3D imaging workstation and Editage (www.editage.com) for English language editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-595/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-595/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-595/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-595/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Maniwa Y. Surgical treatment of air way disease. J Thorac Dis 2016;8:E78-82. [PubMed]
- Rob CG, Bateman GH. Reconstruction of the trachea and cervical oesophagus; preliminary report. Br J Surg 1949;37:202-5, illust. [Crossref] [PubMed]
- Belsey R. Resection and reconstruction of the intrathoracic trachea. Br J Surg 1950;38:200-5. [Crossref] [PubMed]
- Grillo HC, Dignan EF, Miura T. Extensive resection and reconstruction of mediastinal trachea without prosthesis or graft: an anatomical study in man. J Thorac Cardiovasc Surg 1964;48:741-9. [Crossref] [PubMed]
- Mulliken JB, Grillo HC. The limits of tracheal resection with primary anastomosis: further anatomical studies in man. J Thorac Cardiovasc Surg 1968;55:418-21. [Crossref] [PubMed]
- Grillo HC. The history of tracheal surgery. Chest Surg Clin N Am 2003;13:175-89. [Crossref] [PubMed]
- Sekine Y, Itoh T, Toyoda T, et al. Precise Anatomical Sublobar Resection Using a 3D Medical Image Analyzer and Fluorescence-Guided Surgery With Transbronchial Instillation of Indocyanine Green. Semin Thorac Cardiovasc Surg 2019;31:595-602. [Crossref] [PubMed]
- Dong S, Yang XN, Zhong WZ, et al. Comparison of three-dimensional and two-dimensional visualization in video-assisted thoracoscopic lobectomy. Thorac Cancer 2016;7:530-4. [Crossref] [PubMed]
- Bhakhri K, Hyde ER, Mak SM, et al. Surgeon Knowledge of the Pulmonary Arterial System and Surgical Plan Confidence Is Improved by Interactive Virtual 3D-CT Models of Lung Cancer Patient Anatomies. Front Surg 2021;8:652428. [Crossref] [PubMed]
- Kim D, Jeon B, Son JS, et al. The changes of endotracheal tube cuff pressure by the position changes from supine to prone and the flexion and extension of head. Korean J Anesthesiol 2015;68:27-31. [Crossref] [PubMed]
- Fujimoto S, Watanabe T. Studies on the body surface area of Japanese. Acta Med Nagasaki 1969;14:1-13. [PubMed]
- Mi W, Zhang C, Wang H, et al. Measurement and analysis of the tracheobronchial tree in Chinese population using computed tomography. PLoS One 2015;10:e0123177. [Crossref] [PubMed]
- Auchincloss HG, Wright CD. Complications after tracheal resection and reconstruction: prevention and treatment. J Thorac Dis 2016;8:S160-7. [PubMed]
- Grillo HC, Zannini P, Michelassi F. Complications of tracheal reconstruction. Incidence, treatment, and prevention. J Thorac Cardiovasc Surg 1986;91:322-8. [Crossref] [PubMed]
- Couraud L, Bruneteau A, Martigne C, et al. Prevention and treatment of complications and sequelae of tracheal resection anastomosis. Int Surg 1982;67:235-9. [PubMed]
- Wright CD, Grillo HC, Wain JC, et al. Anastomotic complications after tracheal resection: prognostic factors and management. J Thorac Cardiovasc Surg 2004;128:731-9. [Crossref] [PubMed]
- Mohsen T, Abou Zeid A, Abdelfattah I, et al. Outcome after long-segment tracheal resection: study of 52 cases. Eur J Cardiothorac Surg 2018;53:1186-91. [Crossref] [PubMed]
- Dedo HH, Fishman NH. Laryngeal release and sleeve resection for tracheal stenosis. Ann Otol Rhinol Laryngol 1969;78:285-96. [Crossref] [PubMed]
- Montgomery WW. Suprahyoid release for tracheal anastomosis. Arch Otolaryngol 1974;99:255-60. [Crossref] [PubMed]
- Myer CM 3rd, O'Connor DM, Cotton RT. Proposed grading system for subglottic stenosis based on endotracheal tube sizes. Ann Otol Rhinol Laryngol 1994;103:319-23. [Crossref] [PubMed]
- Madariaga MLL, Soni ML, Mathisen DJ, et al. Evaluation of Release Maneuvers After Airway Reconstruction. Ann Thorac Surg 2022;113:406-12. [Crossref] [PubMed]
- Cordos I, Bolca C, Paleru C, et al. Sixty tracheal resections--single center experience. Interact Cardiovasc Thorac Surg 2009;8:62-5; discussion 65. [Crossref] [PubMed]
- Drevet G, Conti M, Deslauriers J. Surgical anatomy of the tracheobronchial tree. J Thorac Dis 2016;8:S121-9. [PubMed]
- Furlow PW, Mathisen DJ. Surgical anatomy of the trachea. Ann Cardiothorac Surg 2018;7:255-60. [Crossref] [PubMed]
- Premakumar Y, Griffin MF, Szarko M. Morphometric characterisation of human tracheas: focus on cartilaginous ring variation. BMC Res Notes 2018;11:32. [Crossref] [PubMed]
- Marty-Ané CH, Picard E, Jonquet O, et al. Membranous tracheal rupture after endotracheal intubation. Ann Thorac Surg 1995;60:1367-71. [Crossref] [PubMed]
- Massard G, Rougé C, Dabbagh A, et al. Tracheobronchial lacerations after intubation and tracheostomy. Ann Thorac Surg 1996;61:1483-7. [Crossref] [PubMed]
- Kaloud H, Smolle-Juettner FM, Prause G, et al. Iatrogenic ruptures of the tracheobronchial tree. Chest 1997;112:774-8. [Crossref] [PubMed]
- Ge X, Huang H, Bai C, et al. The lengths of trachea and main bronchus in Chinese Shanghai population. Sci Rep 2021;11:2168. [Crossref] [PubMed]