
Video-based curriculum improves resident participation during robot-assisted surgery
Introduction
Surgical education has evolved significantly over time. The modern surgical educational system in the United States began with the Halstead model. The model is based on the philosophy that surgery is founded on scientific knowledge and overarching principle of apprenticeship with the progressive transfer of patient care responsibilities and graded autonomy in the operating room (OR) (1). This model has evolved with the development of standards and milestones within the training paradigm enforced by the Accreditation Council for Graduate Medical Education (ACGME) (2). The ACGME has developed core competencies for all surgical training programs and work hour restrictions for the residents in learning these tasks (3). The restriction on time for the residents makes each operative experience a crucial aspect of the development of a surgeon. However, there are challenges in adequately preparing for cases, with most surgical rotations lasting a month at a time with various techniques performed by different surgeons. Some of these challenges may be overcome using video in surgical education.
Video-based learning has made significant strides, from trainees recording their videos for personal feedback training to overhead operating room camera recordings of thoracoscopic and laparoscopic case videos. Learners of all levels, from medical students to attendings, have used the advancement in video-based technology to further their skills and shorten the learning curve (4). There have been specialty collaborations to create large educational video databases (5). Since there is a significant variation in video databases or video sources, it is essential to standardize the use and learning aspects of video-based learning. For example, a study showed that the most valued video characteristics varied by user and expertise level, but resident users most valued the presence of video narration and didactic illustrations (6). Video-based education addresses several challenges within surgical training, including increased knowledge retention within a continuously expanding field of information and a time-constrictive environment.
Within the last decade, one of the most influential changes in surgical technique and technology has been the advent of robotic surgical systems. In a cohort study of 169,404 patients across 73 hospitals, it was found that the use of robotic surgery in general surgery procedures increased from 1.8% in 2012 to 15.1% in 2018. Notably, this was accompanied by a decrease in the use of laparoscopy. As this occurs, it becomes important to integrate robotic education into the curricula for surgeon resident training. In the Society of American Gastrointestinal and Endoscopic Surgeons annual meeting in 2017, a consensus was made on four themes that embraced the challenges of resident robotic training (7). The first theme addressed the need to distinguish the acquisition of content required for mastery of surgical technique from attaining mastery of the robotic platform. The second theme focused on the timing of exposure to the robot technology and the integration of surgical steps from basic to complex. The third theme highlighted the overlapping features between robotic, laparoscopic, and open surgery, which is associated with how a robotic curriculum is integrated, in parallel vs. sequentially. Finally, the fourth theme spotlights the unique aspect of the dual console in robot technology, serving as an important teaching tool.
We hypothesized that residents would be better prepared for surgery by having access to videos of standard procedures performed by an attending surgeon from the current rotation. We implemented our program and tested our theory by administering a survey of the residents. In addition, with the advent of video-based learning and dual console robot technology, we hypothesized that residents with access to a similar case video before the operation would increase their participation in the case. We tested this hypothesis by assessing the time the resident was participating in the operation on the second console before and after implementing the video-based curriculum. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-603/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Houston Methodist Research Institute Research Board approved the study (No. PRO00030171), and informed consent from the residents was waived since the questionnaire was administered anonymously and the data was collected without identifying individual residents. The survey instructions contained the following: “The answers are completely anonymous and confidential. These data are exclusively for us to continue improving the educational experience on the rotation. In the future, these anonymized data may be used for educational research purposes.”
We developed a novel video-based education curriculum to improve surgical training in the thoracic surgery service. We obtained informed consent from each patient to obtain permission to record the operation for teaching purposes. We recorded the procedure using the integrated video system in the operating room (Karl-Storz, Tuttlingen, Germany) and uploaded it to a secure hospital server. We removed patient identification information and edited the video on desktop software (Camtasia, TechSmith, Okemos, Michigan, USA). The video was edited to play at four times the speed of the live operation and included narration highlighting the operation’s important aspects. This was performed by the one surgeon with input from his partners. Each surgeon in the group performs the indicated surgery in largely the same manner, making the steps of the video applicable for residents performing the surgery with any of the attending surgeons.
We placed the video on an online server, Vimeo (Vimeo, LLC, New York, NY, USA), allowing the learner to watch HD videos on numerous platforms. The learner was also able to slow down the video on numerous platforms. An e-mail link was sent Friday afternoon before the week with similar cases that were going to be performed the following week. The attending surgeon explained the availability of the video during the orientation at the beginning of the month, and again at the beginning of the case to gauge the engagement and preparation of the resident for case. Using the Vimeo software, we analyzed the total number of videos and the total number of hours the residents spent watching. We analyzed the number, and the average amount of time the residents spent per month viewing these videos during the 13 months since the program’s implementation.
We performed a retrospective survey study to determine the impact of this curriculum on resident education. After 12 months, we sent a survey to residents who rotated on the service. Twenty-four residents rotated on the service during those 12 months. We asked about their use of the video and its impact on their education. The survey was anonymous. We gave residents one month to complete the survey with three e-mails asking them to complete it. The goal was to improve resident participation in the survey to minimize bias. Survey questions were as follows:
- Demographics: What is your current post graduated year (PGY) level?
- Use of the video: How often did you watch the video before surgery? (always, often, sometimes, rarely)
- Impact of the video:
- Did the videos help you prepare for the surgery? (yes, no)
- Did the videos help you improve your understanding of surgical anatomy? (yes, no)
- Did the videos help you improve your understanding of the cognitive aspects of the operation? (yes, no)
- Did the videos help you improve your understanding of the technical aspects of the operations? (yes, no)
- Did the videos help you better prepare for the operation compared to reading a book? (yes, no)
- Evaluation of the content:
- Was the video of the entire operation helpful in preparing for the operation? (yes, no)
- Was the narration helpful in preparing for the operation? (yes, no)
- Would a shorter video with major parts of the operation be helpful? (yes, no)
- Access to the video:
- Did the weekly e-mail with a link to the content encourage you to watch the video? (yes, no)
- Did the attending asking you if you watched the video encourage you to watch it prior to the operation? (yes, no)
- Suggestions:
- What would you change to improve the video-based learning curriculum?
We calculated the percentage for the answers. We obtained information about the demographics of the residents. We categorized the answers based on the different aspects of the video.
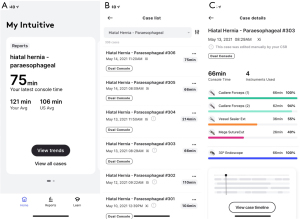
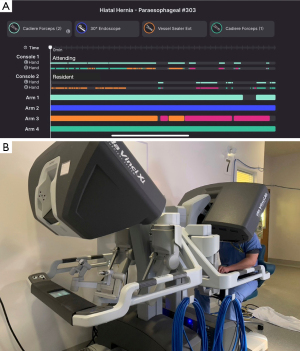
Next, we hypothesized that the video-based curriculum would increase the resident’s participation in the operating room. We used the My Intuitive app (Intuitive Surgical, Sunnyvale, CA, USA, Figure 1), which provides information on the amount of time a person in each surgical console is controlling the robot. We assessed the time the resident had control of the robot for their first robot-assisted hiatal hernia repair of the rotation with a dual console, 13 months before and after implementing the curriculum. We measured the amount of time the attending and resident had control of the robot (Figure 2). We divided it by the total time that the robot was being used in the case to derive the % of the time that the attending and the resident were each using the robot. We obtained the average % of the time before and after the video-based curriculum that the resident was using the robot. We performed a t-test to determine if the groups had a significant difference. P<0.05 was considered a significant value.
Results
There were 43 different surgical videos created for this curriculum that included esophagectomy, hiatal hernia repair, diaphragm plication, lobectomy, segmentectomy, pneumonectomy, supercharged jejunal reconstruction, Nissen fundoplication, Toupet fundoplication, magnetic sphincter augmentation, Heller myotomy, thymectomy, posterior mediastinal mass resection, mediastinal lymph node and lung nodule localization. Each video took about 2–3 hours to create, from editing the video to placing it on the web-based server. Every Friday, the attending reviewed all upcoming cases for the following week, created a curated list of videos for the resident, and sent it to the residents to review before the operation. Typically, three residents were on the service during the month-long rotation (intern, junior resident, and chief resident). The chief resident sent the weekly schedule to residents, so each learner understood which case they were assigned to cover during the week. On average, 37 videos were viewed during the month, with residents spending 16 hours per month viewing the videos. Among the 20 out of 24 residents who completed the survey, 30% were interns, 35% were junior residents (PGY2 15% and PGY3 20%), and 35% were chief residents (PGY4 20% and PGY5 15%). 90% of the residents either watched the videos always (40%) or often (50%) before the operation.
The first set of questions asked about the usefulness of the video content. All the residents stated that the video helped them prepare for the surgery (100%). The majority of the residents felt that the video helped them improve their understanding of the surgical anatomy (95%) and the cognitive aspect of the surgery (95%), while all of them felt that the video improved their understanding of the technical aspect of the operation (100%). Compared to reading a book, all the residents felt that the video was better at preparing them for surgery (100%). The second set of questions asked about the format of the content. Most residents felt that the video of the entire operation was helpful (85%) with narration (100%). However, the residents also felt that having a shorter video with major parts of the operation would also be helpful (100%). The last set of questions asked about the use of the content. Most of the residents felt that weekly e-mail with the link to the video was helpful (95%), as was the attending encouraging the residents to watch the video (80%). There were 14 comments from the residents (Appendix 1), and most of them point to having a shorter video with a description of the anatomy with key steps that would be helpful for resident education.
The most common operation and video watched was a robot-assisted hiatal hernia repair with fundoplication. We analyzed the resident console time of the month’s first robot-assisted hiatal hernia repair. All residents who performed the first robot-assisted hiatal hernia repair were chief residents. During the 13 months before implementing the video-based curriculum, the residents spent 11% of the time controlling the robot during the case. After the implementation of the program, the resident spent significantly more time controlling the robot (48%, P<0.0001, Figure 3).

Discussion
Surgical education is a career-long process. It requires the adaptability to assimilate an increasingly greater breadth of information to be mastered in a limited time. Surgical training is particularly subject to this challenge as learners are expected to achieve competency in performing surgeries using different technologies—most recently, the robotic platform. While surgical coaching has been explored as a learning tool (8), it requires time and planning from trainees and instructors to discuss and analyze videos for learning. On the other hand, the use of educational videos factors out the need for trainees and instructors to find a common time. The trainee can use the videos at their liberty and prepare for the operating room as it fits in their schedule. Not only is it critical for the trainee to organize their own time, but video learning has also benefited trainees more than manuscript learning in studies (9). Trainees now tend to prefer the mobility and time flexibility that video learning has, which has translated into an improvement in learning curves (4).
In our study, a video-based surgical education curriculum has been helpful for residents as they prepare to participate in cases. Access to videos of similar operations before the case allows the resident to better prepare for the case than reading a textbook. It allows them to have a better understanding of the surgical anatomy, as well as the cognitive and technical aspects of the operation. This finding is echoed in studies examining the use of educational videos (10). Fan et al. found that online-video-based teaching tools increase the knowledge base of medical students, residents, and practicing physicians (11). Moreover, Celentano et al. found that surgery residents routinely watch videos before a case, reviewing critical anatomy using YouTube and Websurg.com (12). Studies have shown that the most watched videos on YouTube often do not provide the best surgical technique (13,14). A unique aspect of our study is that the videos provided to the residents are developed by the surgeons who are providing the training. The surgeon allows control of the quality of content that the resident sees during the operation.
Specifically, 95% of the trainees specified that the videos provided helped their understanding of the operation’s surgical anatomy and cognitive aspects. This is a key finding, given that so much time and effort is spent teaching these two points in the operating room. Understanding surgical anatomy outside the operating room has long represented a challenge to resident learners because in vivo representation differs from still drawings and text. It has always been vital to learn anatomy through cadaveric dissections and labs (15). Technological advancements have allowed for a progression of simulation applications that merge print material and 3D representation. Still, the most useful resident learning tool may be the ability to see anatomy as it is presented during the operation, shortening the learning curve. These surgical educational videos are helpful with anatomy, but they also help contextualize the surgical steps described in books. It solidifies the learning process as the learner can visualize and piece together the different parts of the surgery as it unfolds within the educational video. Surgical videos provide the “see one” aspect of Halsted’s learning model before arriving in the operating room.
Creating an operative video requires a significant amount of time to make and distribute, however, there is minimal capital expense involved. We created and distributed the content using commercially available software and web-based programs, similar to what other groups have done to make videos for clinical teaching (16). One advantage we had was an operating room designed with the capability to record both minimally invasive and open procedures securely stored on a centralized server. The largest amount of time was spent adding the narration to the video. Once the video was created, it was placed on a web-based platform for distribution so that residents could easily access it through any internet-capable device. Most practicing surgeons may not have the time to be able to make this type of time investment. One option that we have explored is to have senior residents or research fellows create these videos using the infrastructure already in place for editing and publishing the video. This may also provide valuable teaching and learning opportunities for the residents and fellows who create the videos and help increase the content volume for educational purposes.
In discussing what content to include in the videos, we opted to provide the entire video of the operation at four times the regular speed for the viewer to have access to the entire operation instead of parts of the operation. This allows a learner to understand how a case progressed from one part to another. We also added narration of the video to provide insight into the operation. Most of the residents felt this was a helpful feature for viewing the operation. However, some of the comments requested having videos that were shorter with highlights of the anatomy and key steps. The difference in opinion may be due to the difference in the level of training for the residents. Learners at the novice level who have not seen or performed a particular operation may need anatomic information as well as a narration of the parts of the operation. In contrast, residents at the advanced beginner or competent level who are familiar with the operation are more focused on the techniques of tissue handling and progression of the operation. Thus, it may be optimal to create two different types of videos to address the needs of two different groups of learners. One type of video would be an abridged, narrated video that provides information about the parts of the operation and anatomy. Another type of video would be the entire operation.
The key finding in our study is the statistically significant increase in resident console time after the implementation of the surgical education videos from 11% to 48% of the operating time. The difference was seen in the fact that the resident no longer needed to spend valuable operating room time “seeing one”. The trainee had seen the operation by a known attending surgeon from the surgical group via a prescribed surgical video. Therefore, on the day of the surgery, the operating surgeon felt confident that the trainee had prepared with high-quality material. There is a standardization of quality, and there is less concern with variability. The trainee also has greater confidence that the surgical steps that they have reviewed will be in line with the steps performed by the attending surgeon. Therefore, the trainee and instructor are confident in their willingness and ability to participate in the operation.
Our study is unique in that we can objectively quantify the trainee’s participation during an operation. Up to this point, participation has been gauged by subjective questionnaires from the learner or instructor asking about autonomy and parts of the surgery performed by the trainee. While this can still be useful, there is a lot of variability in definitions of autonomy, and therefore there is a gap in objective data. With the My Intuitive App, there is greater transparency and quantifiable data regarding trainee participation. While at this point, we are not using the data to identify what parts of the operation are being performed, we can identify the amount of time spent participating relative to the total length of the case. The data, therefore, becomes objective and actionable.
The robotic dual console has myriad useful tools (17,18). The dual console allows the trainee to have the same visibility as the attending surgeon and removes the perception of distance from the surgical field. The trainer can perform integrated teaching with surgical coaching, touch screen drawing, and virtual pointer capabilities to give real-time advice and guidance. It also facilitates transferring control of arms and instruments without significantly changing operative times or patient outcomes (19). Finally, there is an emergency stop button for the trainer to use.
The limitation of the study is that this is a single institution retrospective experience of using a video-based curriculum, and that some of the data are based on the opinions of the learners who went through the curriculum without a control group. In addition, the number of subjects is relatively small with only 24 residents in the study. Thus, there may be significant bias introduced in this study. The survey was administered at one time point; thus, there may have been a difference in opinion between a learner who had the rotation within the month of the survey compared to the learner who had the rotation 12 months before the survey. Moreover, some learners did not answer the survey. However, 80% replied to the survey, with most of the learners providing similar views of the value of the video-based curriculum. In addition, we did not randomize residents to determine who had access to a video-based curriculum vs. no video-based curriculum to determine the impact of the curriculum because we felt that this would be an important adjunct to resident education. A randomized controlled trial would have provided stronger evidence for this curriculum. However, both learner’s perspective and objective data from the resident console time support the benefit of the curriculum.
Overall, a video-based curriculum that provides similar narrated videos for learners before operations provides a tool that prepares them for the technical and cognitive aspects of surgery. In addition, we found that video-based learning increases resident robot console time. We believe this is a valuable finding in an era when trainees increasingly use the internet to prepare for the operating room. We hope this encourages programs to analyze the quality and platforms from which trainees obtain training material and recognize that providing a video-based platform can improve trainee operating room participation and enhance learning.
Acknowledgments
Funding: This work was supported by the American College of Surgeons-Accredited Education Institutes Fellowship Program (Houston Methodist Institute for Technology, Innovation, and Education-MITIE) and Houston Methodist Academic Institute Clinical Scholar Awards-Clinician Educator Award.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-603/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-603/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-603/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-603/coif). MPK serves as an unpaid editorial board member of Journal of Thoracic Disease from September 2022 to August 2024. EYC serves as an unpaid editorial board member of Journal of Thoracic Disease from February 2022 to January 2024. MPK has consulted for AstraZeneca, Olympus, Medtronic, and Intuitive Surgical. EYC has consulted for Olympus and Intuitive Surgical. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Houston Methodist Research Institute Research Board approved the study (No. PRO00030171), and informed consent from the residents was waived since the questionnaire was administered anonymously and the data was collected without identifying individual residents.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Grillo HC. To impart this art: the development of graduate surgical education in the United States. Surgery 1999;125:1-14.
- Swanson AG. The genesis of the Coordinating Council on Medical Education and the Liaison Committee on Graduate Medical Education. Bull N Y Acad Med 1974;50:1216-21.
- Education ACfGM. Common Program Requirements 2013. Available online: http://www.acgme.org/acgmeweb/Portals/0/dh_dutyhoursCommonPR07012007.pdf
- Ahmet A, Gamze K, Rustem M, et al. Is Video-Based Education an Effective Method in Surgical Education? A Systematic Review. J Surg Educ 2018;75:1150-8. [Crossref] [PubMed]
- Brown CS, Cunningham CD 3rd, Lee WT, et al. Development of a Surgical Video Atlas for Resident Education: 3-Year Experience. OTO Open 2020;4:2473974X20939067.
- Mota P, Carvalho N, Carvalho-Dias E, et al. Video-Based Surgical Learning: Improving Trainee Education and Preparation for Surgery. J Surg Educ 2018;75:828-35. [Crossref] [PubMed]
- Green CA, Mahuron KM, Harris HW, et al. Integrating Robotic Technology Into Resident Training: Challenges and Recommendations From the Front Lines. Acad Med 2019;94:1532-8. [Crossref] [PubMed]
- Greenberg CC, Dombrowski J, Dimick JB. Video-Based Surgical Coaching: An Emerging Approach to Performance Improvement. JAMA Surg 2016;151:282-3. [Crossref] [PubMed]
- Reck-Burneo CA, Dingemans AJM, Lane VA, et al. The Impact of Manuscript Learning vs. Video Learning on a Surgeon’s Confidence in Performing a Difficult Procedure. Front Surg 2018;5:67. [Crossref] [PubMed]
- Green JL, Suresh V, Bittar P, et al. The Utilization of Video Technology in Surgical Education: A Systematic Review. J Surg Res 2019;235:171-80. [Crossref] [PubMed]
- Fan T, Workman AD, Koch G, et al. Educational utility of an online video-based teaching tool for sinus and skull base surgery. Laryngoscope Investig Otolaryngol 2021;6:195-9. [Crossref] [PubMed]
- Celentano V, Smart N, Cahill RA, et al. Use of laparoscopic videos amongst surgical trainees in the United Kingdom. Surgeon 2019;17:334-9. [Crossref] [PubMed]
- Rodriguez HA, Young MT, Jackson HT, et al. Viewer discretion advised: is YouTube a friend or foe in surgical education? Surg Endosc 2018;32:1724-8. [Crossref] [PubMed]
- de’Angelis N, Gavriilidis P, Martínez-Pérez A, et al. Educational value of surgical videos on YouTube: quality assessment of laparoscopic appendectomy videos by senior surgeons vs. novice trainees. World J Emerg Surg 2019;14:22. [Crossref] [PubMed]
- Smith CF, Martinez-Álvarez C, McHanwell S. The context of learning anatomy: does it make a difference? J Anat 2014;224:270-8. [Crossref] [PubMed]
- Krumm IR, Miles MC, Clay A, et al. Making Effective Educational Videos for Clinical Teaching. Chest 2022;161:764-72. [Crossref] [PubMed]
- Morgan MS, Shakir NA, Garcia-Gil M, et al. Single- versus dual-console robot-assisted radical prostatectomy: impact on intraoperative and postoperative outcomes in a teaching institution. World J Urol 2015;33:781-6. [Crossref] [PubMed]
- Mikhail E, Salemi JL, Hart S, et al. Comparing Single and Dual Console Systems in the Robotic Surgical Training of Graduating OB/GYN Residents in the United States. Minim Invasive Surg 2016;2016:5190152. [Crossref] [PubMed]
- Smith AL, Scott EM, Krivak TC, et al. Dual-console robotic surgery: a new teaching paradigm. J Robot Surg 2013;7:113-8. [Crossref] [PubMed]


