A dense fissure is not a contra-indication for uniportal thoracoscopic lobectomy
Introduction
Rocco et al. [2004] were the first to report uniportal thoracoscopic pulmonary wedge resection, followed by Gonzalez [2011], who reported the first case of uniportal, thoracoscopic, major pulmonary resection (1,2). A uniportal thoracoscopic approach is usually considered less invasive than a multiportal approach because only one port is required. Several authors have successfully used a uniportal thoracoscopic approach in major pulmonary resection (3-5). Dai et al., in a prospective study, found that a uniportal thoracoscopic approach in lung cancer lobectomy was associated with fewer patient-reported severe symptoms and better functional status in the early postoperative period than a multiportal approach (3). Bourdages-Pageau et al. reported that a uniportal thoracoscopic approach was safe and feasible, and yielded short-term outcomes similar to those of a multiportal approach for early stage, non-small-cell lung cancer patients, although the former approach tended to be chosen by only highly experienced surgeons (4). We also noted better perioperative outcomes of patients undergoing thoracoscopic, anatomical pulmonary resection when the uniportal rather than the multiportal approach was employed (5). The uniportal approach was the only factor significantly associated with less postoperative pain. However, a uniportal approach is more difficult than a multiportal approach; several surgical instruments are simultaneously inserted via a small skin incision and may interfere with each other during surgery, rendering manipulations difficult.
A prolonged air leak (PAL) after lobectomy is frequent in patients with dense fissures. In addition, the pulmonary artery tends to be incidentally injured in such patients; catastrophic bleeding may develop if the pulmonary artery is dissected and exposed at the fissure. Thus, a dense fissure is considered to render thoracoscopic lobectomy difficult. We therefore retrospectively investigated whether uniportal thoracoscopic lobectomy was appropriate for patients with dense fissures; we compared the perioperative outcomes of patients with and without such fissures. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1073/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of Japanese Red Cross Maebashi Hospital (Approval No. 2022–04). The need for individual patient consent was waived given the retrospective nature of the work. We introduced uniportal, major, thoracoscopic pulmonary resections in February 2019, initially for only cT1N0 cases to ensure safety and to allow the surgical team to become familiar with this less-invasive procedure. During this period, we continued to use a multiportal approach toward all other major pulmonary resections. In December 2019, after our team had performed 30 uniportal approaches, we adopted this approach for all primary lung cancer patients. All such surgeries were performed by HI or NM, both of whom have performed over 500 thoracoscopic, major pulmonary resections via a multiportal approach.
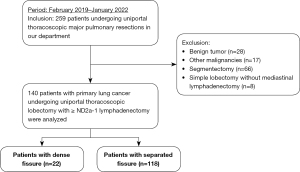
Between February 2019 and January 2022, 259 patients underwent major, uniportal thoracoscopic pulmonary resections. Uniportal thoracoscopic lobectomy with ≥ ND2a-1 lymphadenectomy was performed for 140 patients with lung cancer; all were enrolled in the present study (Figure 1). Patients requiring bronchoplasty or angioplasty, or with tumors >7 cm in diameter, were not eligible for thoracoscopic surgery. The patients were classified into those with dense (n=22) and separated (n=118) fissures. We compared the patient characteristics and perioperative results of the two groups. The clinical data analyzed included age, sex, American Society of Anesthesiologists (ASA) score; the smoking index (pack × year); the forced expiratory volume in 1 s (FEV1.0); the %FEV1.0; tumor location, histology, and pathological stage; the surgical technique (the fissureless or conventional technique) (6-8); the operative time; intraoperative blood loss; duration of postoperative drainage; postoperative PAL status (continuous air leakage for ≥5 days postoperatively); postoperative hospitalization time; the number of dissected lymph nodes; rate of conversion to thoracotomy; rate of re-admission within 30 days after operation; morbidity (Clavien-Dindo grade ≥III); and 30- and 90-day postoperative mortality. Factors predictive of PAL were sought via univariate and multivariate analyses.
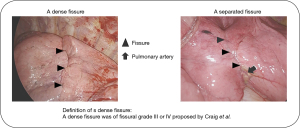
Definition of a dense fissure
A dense fissure was of fissural grade III or IV (Craig, 1997) or a fissure that was inflamed to an extent rendering it difficult to expose the pulmonary artery using counter-traction (9). Figure 2 shows the intraoperative image of the patients with dense and separated fissures.
Uniportal thoracoscopic procedure
Uniportal, major, thoracoscopic pulmonary resection was performed with the patient under general anesthesia on one-lung ventilation in the lateral decubitus position. We placed a monitor above the head. A 3.5–4 cm incision was created in the fourth or fifth intercostal space from the anterior axillary line and covered with an XXS Alexis wound retractor (Applied Medical, Rancho Santa Margarita, CA, USA). We inserted a 5 or 10 mm 30° thoracoscope and other surgical instruments. The large vessels and bronchi were divided with a stapler. Small-caliber vessels were divided with an energy device after proximal ligation. Specimens were placed in an endovascular bag and retrieved through the incision after completion of pulmonary resection. The incision was lengthened if required. We did not use a rib-spreader. For all the patients undergoing lobectomy to treat primary lung cancer, ≥ ND2a-1 systemic lymphadenectomy was performed. When an air leak was found on a sealing test performed at the end of surgery, we applied a polyglycolic acid felt (a Neoveil sheet; Igaki Medical Planning Co., Ltd., Kyoto, Japan) and fibrin glue (Beriplast P; CSL Behring, King of Prussia, PA, USA) with or without 3-0 absorbable monofilament sutures. Finally, a 19 Fr Blake chest drain (Ethicon, Paramus, NJ, USA) or a 24 Fr double-lumen chest tube (ArgyleTM Trocar Catheter; Cardinal Health K.K., Tokyo, Japan) was positioned in the thorax.
The fissureless technique of the uniportal thoracoscopic approach
Right upper lobectomy (Video 1 shows the details)
The first branch of the pulmonary artery was initially divided at the hilum with caudal retraction of the upper lobe. Then the upper bronchus was divided with en-bloc harvesting of the lymph nodes of the second carina (LN#11s). Next, the ascending pulmonary artery was divided to the posterior segment of the upper lobe. Finally, the upper lobe pulmonary vein was divided. After these preparations, the dense fissure was divided using staplers from anterior to posterior.
Right middle lobectomy
We encountered no patients with a dense fissure who underwent right middle lobectomy.
Right or left lower lobectomy
Initially, the inferior pulmonary vein was divided after dissection of the pulmonary ligament, with retraction of the lower lobe toward the head. Then the lower bronchus was carefully encircled and divided. We used a suction-guided technique to avoid injury to the pulmonary artery behind the bronchus that might have been caused by mis-insertion of a forceps or stapler (10,11). Next, the branches of the lower lobe pulmonary arteries were divided. On the monitor, the branches were flipped. Therefore, we were careful to divide the correct branches. Finally, the dense fissure was divided using staplers from anterior to posterior.
Left upper lobectomy (Video 1 shows the details)
With the upper lobe retracted caudally, the superior pulmonary vein and upper lobe pulmonary arteries were divided in an order that depended on the locations of the branches. Then the upper lobe bronchus was divided using a stapler; we were careful to not injure the pulmonary artery behind the bronchus. Next, the lingual, segmental pulmonary arteries were exposed and divided. Finally, the dense fissure was divided from anterior to posterior.
Postoperative management
The chest tube was removed when air leakage ceased, regardless of the fluid volume on postoperative day 1 or later. If air leakage persisted for more than 3 days, we performed pleurodesis if the patient’s respiratory status was permitted. The PAL continued for more than a weak postoperatively, we planned to perform reoperation to cease it although it depended on the patient condition and degree of the air-leakage.
Statistical analysis
We used the Fisher exact test to compare categorical variables and the t-test and Mann-Whitney U-test to compare continuous variables. A P value <0.05 was considered statistically significant. Multivariate analyses of categorical variables were performed using logistic regression. We propensity score-matched the patients of the two groups including fissureless and conventional techniques. Propensity scores were calculated using a logistic regression model including the following variables: age, sex, ASA score, smoking index, FEV1.0, %FEV1.0, and tumor location, histology, and pathological stage. All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan) with a graphical user interface for R (R Foundation for Statistical Computing, Vienna, Austria).
Results
Table 1 compares the characteristics and perioperative outcomes of patients with dense and separated fissures. The fissureless technique was employed for all patients with dense fissures (P<0.0001). Although such fissures were significantly associated with right upper lobectomy, all other patient characteristics and perioperative results were identical between the two groups. Moreover, no significant pulmonary artery injuries occurred in the fissureless group. Table 2 shows the results of subgroup analyses of right upper lobectomy patients. A dense fissure was significantly associated with a more advanced pathological stage; we found no other significant between-group differences in patient characteristics or perioperative results. Table 3 lists the details of the seven patients with PAL. Six with separated fissures underwent the conventional technique; only one patient with a dense fissure received the fissureless technique. Pleural adhesions were found around the entire thorax of one patient and part of the thoraces of two patients. All patients underwent pleurodesis; air leakage ceased in four. The remaining three underwent surgical interventions. Intraoperatively, the leakage points were on the staple line in one and in the regions of the dissected pleural adhesions in two. Table 4 lists the factors predictive of PAL in univariate and multivariate analyses. Right upper lobectomy [odds ratio (OR): 0.047, 95% confidence interval (CI): 0.0044–0.49, P=0.011] or smoking index (OR: 1.03, 95% CI: 1–1.07, P=0.048) was the factor predictive of PAL in multivariate analysis. A dense fissure was not such a factor.
Table 1
| Variables | Pts. with dense fissures (n=22, %) | Pts. with separated fissures (n=118, %) | P value |
|---|---|---|---|
| Age (years) | 69±12 | 72±10 | 0.18 |
| Sex | 0.64 | ||
| Female | 11 (50.0) | 50 (42.4) | |
| Male | 11 (50.0) | 68 (57.6) | |
| ASA score, median [IQR] | 2 [1–3] | 2 [1–3] | 0.65 |
| Smoking index (pack × year) | 22±25 | 25±128 | 0.66 |
| FEV1.0 (mL) | 2,361±913 | 2,204±571 | 0.29 |
| %FEV1.0 (%) | 97±19 | 95±18 | 0.56 |
| Tumor location | 0.00073 | ||
| RUL | 16 (72.7) | 29 (24.6) | |
| RML | 0 (0) | 10 (8.5) | |
| RLL | 2 (9.1) | 41 (34.7) | |
| LUL | 2 (9.1) | 16 (13.6) | |
| LLL | 2 (9.1) | 22 (18.6) | |
| Histology | 0.87 | ||
| Adenocarcinoma | 17 (77.3) | 83 (70.3) | |
| Squamous cell carcinoma | 4 (18.2) | 23 (19.5) | |
| Others | 1 (4.5) | 12 (10.2) | |
| p-Stage | 0.39 | ||
| 0 | 1 (4.5) | 1 (0.8) | |
| I | 13 (59.1) | 87 (73.7) | |
| II | 1 (4.5) | 14 (11.9) | |
| II | 6 (27.3) | 14 (11.9) | |
| IV | 1 (4.5) | 2 (1.7) | |
| Surgical steps | <0.0001 | ||
| Fissureless technique | 22 (100.0) | 10 (8.5) | |
| Conventional technique | 0 (0) | 108 (91.5) | |
| Operative time (min) | 164±39 | 149±41 | 0.14 |
| Blood loss (g) | 51±60 | 44±82 | 0.71 |
| Significant vessel injury | 1 (4.5) | 5 (4.2) | 1 |
| Conversion to thoracotomy | 0 (0) | 7 (5.9) | 0.6 |
| Duration of postoperative drainage (days) | 1.5±1.1 | 1.7±1.6 | 0.66 |
| PAL | 1 (4.5) | 6 (5.1) | 1 |
| Postoperative hospitalization time (days) | 3.2±1.6 | 5.8±18 | 0.51 |
| Number of harvested lymph nodes | 11.1±5.5 | 9.4±6.2 | 0.35 |
| Morbidity (C-D classification grade ≥3) | 1 (4.5) | 20 (16.9) | 0.2 |
| Re-admission within 30 days of operation | 1 (4.5) | 9 (7.6) | 1 |
| 30-day postoperative mortality | 0 (0) | 0 (0) | – |
| 90-day postoperative mortality | 0 (0) | 0 (0) | – |
Data are expressed as mean ± SD, n (%), or median [IQR]. Pts., patients; ASA, American Society of Anesthesiologists; IQR, interquartile range; FEV, forced expiratory volume; RUL, right upper lobe; RML, right middle lobe; RLL, right lower lobe; LUL, left upper lobe; LLL, left lower lobe; p-Stage, pathological-stage; PAL, prolonged air leakage; C-D classification, Clavien-Dindo classification.
Table 2
| Variables | Pts. with dense fissures (n=16, %) | Pts. with separated fissures (n=29, %) | P value |
|---|---|---|---|
| Age (years) | 68±12 | 70±12 | 0.46 |
| Sex | 0.76 | ||
| Female | 7 (43.8) | 15 (51.5) | |
| Male | 9 (56.2) | 14 (48.3) | |
| ASA score, median [IQR] | 2 [1–3] | 2 [1–3] | 0.89 |
| Smoking index (pack × year) | 21±24 | 27±34 | 0.52 |
| FEV1.0 (mL) | 2,484±1,007 | 2,115±513 | 0.11 |
| %FEV1.0 (%) | 95±19 | 93±18 | 0.65 |
| Histology | 1 | ||
| Adenocarcinoma | 12 (75.0) | 21 (72.4) | |
| Squamous cell carcinoma | 3 (18.8) | 7 (24.1) | |
| Others | 1 (6.2) | 1 (3.4) | |
| p-Stage | 0.043 | ||
| 0 | 1 (6.2) | 0 (0) | |
| I | 9 (56.2) | 27 (93.1) | |
| II | 1 (6.2) | 1 (3.4) | |
| II | 4 (25.0) | 1 (3.4) | |
| IV | 1 (6.2) | 0 (0) | |
| Surgery | <0.0001 | ||
| Fissureless technique | 16 (100.0) | 10 (34.5) | |
| Conventional technique | 0 (0) | 19 (65.5) | |
| Operative time (min) | 159±40 | 148±39 | 0.35 |
| Blood loss (g) | 42±59 | 37±111 | 0.88 |
| Significant vessel injury | 1 (6.2) | 0 (0) | 0.36 |
| Conversion to thoracotomy | 0 (0) | 1 (3.4) | 1 |
| Duration of postoperative drainage (days) | 1.7±1.3 | 2.1±2.4 | 0.49 |
| PAL | 1 (6.2) | 4 (13.8) | 0.64 |
| Postoperative hospitalization time (days) | 3.4±1.8 | 5.7±12 | 0.45 |
| The number of harvested lymph nodes | 16.8±6.2 | 15.9±7.5 | 0.7 |
| Morbidity (C-D classification grade ≥3) | 1 (6.2) | 5 (17.2) | 0.4 |
| Readmission within 30 days of operation | 1 (6.2) | 2 (6.9) | 1 |
| 30-day postoperative mortality | 0 (0) | 0 (0) | – |
| 90-day postoperative mortality | 0 (0) | 0 (0) | – |
Data are expressed as mean ± SD, n (%), or median [IQR]. Pts., patients; ASA, American Society of Anesthesiologists; IQR, interquartile range; FEV, forced expiratory volume; p-Stage, pathological-stage; PAL, prolonged air leakage; C-D classification, Clavien-Dindo classification.
Table 3
| Case number | Treated lobe | Fissure | Surgical type | Pleural adhesion | Postoperative pleurodesis | Re-operation | Leakage point | Duration of postoperative drainage (days) |
|---|---|---|---|---|---|---|---|---|
| 1 | RUL | Separated | Conventional | Observed around entire thorax | + | − | Unknown | 7 |
| 2 | RUL | Separated | Conventional | None | + | − | Unknown | 5 |
| 3 | RUL | Dense | Fissureless | None | + | − | Unknown | 6 |
| 4 | RUL | Separated | Conventional | Observed around part of thorax | + | + | Dissected area of pleural adhesion | 10 |
| 5 | RLL | Separated | Conventional | None | + | − | Unknown | 6 |
| 6 | LLL | Separated | Conventional | None | + | + | Staple-line | 9 |
| 7 | RUL | Separated | Conventional | Observed around part of thorax | + | + | Dissected area of pleural adhesion | 8 |
RUL, right upper lobe; RLL, right lower lobe; LLL, left lower lobe.
Table 4
| Factors | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | P value | Odds ratio | 95% CI | P value | ||
| Age (continuous) | 1.02 | 0.94–1.1 | 0.71 | 0.97 | 0.82–1.14 | 0.68 | |
| Sex: male (vs. female) | 2 | 0.37–10.6 | 0.59 | 13.3 | 0.1–1,700 | 0.3 | |
| ASA score: 3 (vs. 1–2) | 2.6 | 0.28–24.3 | 0.4 | 0.17 | 0.00021–129 | 0.6 | |
| Smoking index (continuous) | 1.02 | 0.999–1.04 | 0.057 | 1.03 | 1–1.07 | 0.048 | |
| FEV1.0 (continuous) | 1 | 0.999–1.04 | 0.96 | 1 | 0.99–1 | 0.24 | |
| %FEV1.0 (continuous) | 0.99 | 0.95–1.04 | 0.7 | 1.1 | 0.98–1.25 | 0.11 | |
| Tumor location: other lobes (vs. RUL) | 0.17 | 0.032–0.92 | 0.04 | 0.047 | 0.0044–0.49 | 0.011 | |
| Fissure: dense (vs. separated) | 0.89 | 0.1–7.7 | 0.92 | 1.46×107 | 0–Inf | 0.99 | |
| Histology: other histologies (vs. adenocarcinoma) | 1 | 0.19–5.4 | 1 | 0.08 | 0.0024–2.65 | 0.16 | |
| p-Stage: II–IV (vs. 0–I) | 0.43 | 0.05–3.7 | 0.45 | 0.39 | 0.027–5.4 | 0.48 | |
| Surgical steps: conventional (vs. fissureless) | 1.82 | 0.21–15.7 | 0.59 | 4.19×107 | 0–Inf | 0.99 | |
| Operative time (continuous) | 1.01 | 0.99–1.03 | 0.23 | 1.01 | 0.96–1.05 | 0.8 | |
| Blood loss (continuous) | 1.01 | 1–1.01 | 0.038 | 1.01 | 0.99–1.02 | 0.28 | |
CI, confidence interval; ASA, American Society of Anesthesiologists; FEV, forced expiratory volume; RUL, right upper lobe; p-Stage, pathological-stage.
Discussion
Many reports have emphasized the merits of the uniportal approach which is of course less invasive than the multiportal approach. Perioperative results have also been reported to be superior to those of the multiportal approach (3-5). However, patient backgrounds and the technical difficulties encountered have differed among previous studies. It was not clear whether all patients would benefit from a uniportal approach; again, instrument manipulation is difficult. Thus, here, we focused on patients with dense fissures, treatment of whom is accepted to be difficult. However, the perioperative outcomes of patients with dense and separated fissures were identical. A dense fissure is not a contraindication for uniportal thoracoscopic lobectomy. To the best of our knowledge, this is the first study to describe the feasibility of uniportal thoracoscopic lobectomy for such patients.
A dense fissure is most common between the right upper and middle lobes and dissection is occasionally associated with PAL or accidental injury of the pulmonary artery. In this study, 72.7% of dense fissures were in patients requiring right upper lobectomy. We thus performed subgroup analyses of these patients; earlier reports focused on the perioperative outcomes of such patients (12,13). The perioperative outcomes of patients with dense and separated fissures were very similar. In these analyses, the fissureless technique was selected for the 34.5% of patients with separated fissures. We place our single port on the anterior axillary line, which is appropriate when using the fissureless technique; instrument angulation is limited and the unidirectional dissection of the fissureless technique easy to perform (14,15). We frequently choose the fissureless technique even for patients with separated fissures. Right upper lobectomy is the easiest and most common form of fissureless lobectomy via uniport. On the contrary, fissureless lower lobectomies must be carefully performed because injury to the pulmonary artery behind the lower lobe bronchus can cause catastrophic bleeding when the lower bronchus is encircled or divided by a stapler (6-8). We consider that a uniportal, thoracoscopic anterior approach ensures safe dissection of the lower bronchus, because a good anterior operative view of the lower lobe pulmonary artery and bronchus is available. We usually employ suction-guided stapling to avoid injury to the lower lobe pulmonary artery that might be caused by mis-insertion of a stapler (10,11). We encountered no instances of significant, intraoperative vessel injury using the fissureless technique; this technique is safe.
Postoperative PAL can trigger pneumonia or atelectasis caused by pain and slow patient mobilization. Attaar et al. reported that PAL was associated with pulmonary complications, re-admission, and delayed hospital discharge (16). Konstantinidis et al. reported that 18 of 59 patients requiring re-admission within 90 days of discharge exhibited prolonged chest drainage (17). Although a dense fissure is usually considered a prime cause of postoperative PAL, our multivariate analysis revealed otherwise. A dense fissure was not associated with PAL in patients undergoing uniportal thoracoscopic lobectomies via the fissureless technique.
In multivariate analysis, the smoking index and right upper lobectomy were predictive of PAL. Moreover, five of the seven cases with PAL underwent right upper lobectomy (Table 3). Similarly, Seder et al. described right upper lobectomy was an independent contribution factor to PAL in the study using The Society of Thoracic Surgeons General Thoracic Surgery Database (STS GTSD) although the study included the patients receiving thoracotomy or multiportal thoracoscopic approach (18). Although the reason for this association is unclear, pleural adhesions around the entire or partial thoraces were observed in three of the five cases. Inappropriate dissection of the pleural adhesion or suboptimal treatment of the dissected area may have triggered PAL. In fact, this was intraoperatively apparent in two of the three cases who required surgery to stop PAL. Surgeons who dissect pleural adhesions or who suture leakage points via a uniportal approach must improve their skills.
Our work had several limitations. The study was retrospective in nature, of small sample size, and performed at a single institution. The separated fissure patients included those with pleural adhesions or underlying pulmonary disease who were technically difficult to treat; this may have affected the perioperative outcomes. In addition, application of a polyglycolic acid felt with fibrin glue or postoperative pleurodesis might affect the occurrence rate of PAL. Moreover, the surgical procedure ratios (the fissureless: conventional technique ratios) differed significantly between patients with dense and separated fissures.
Conclusions
Uniportal, thoracoscopic pulmonary lobectomy is feasible even for patients with dense fissures; the fissureless technique affords perioperative outcomes equivalent to those of patients with separated fissures. Moreover, all fissureless surgeries can be safely performed without injury to the pulmonary artery. A dense fissure is not a contraindication for uniportal, thoracoscopic pulmonary lobectomy using a fissureless technique.
Acknowledgments
The authors thanks all of the surgeons and coworkers who contributed to this study, as well as the editors and reviewers for their assistance with the manuscript.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1073/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1073/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1073/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1073/coif). HI served as unpaid editorial board member of Journal of Thoracic Disease from August 2022 to July 2024. The other authors have no conflict of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of Japanese Red Cross Maebashi Hospital (Approval No. 2022–04) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Dai W, Dai Z, Wei X, et al. Early Patient-Reported Outcomes After Uniportal vs Multiportal Thoracoscopic Lobectomy. Ann Thorac Surg 2022;114:1229-37. [Crossref] [PubMed]
- Bourdages-Pageau E, Vieira A, Lacasse Y, et al. Outcomes of Uniportal vs Multiportal Video-Assisted Thoracoscopic Lobectomy. Semin Thorac Cardiovasc Surg 2020;32:145-51. [Crossref] [PubMed]
- Matsuura N, Igai H, Ohsawa F, et al. Uniport vs. multiport video-assisted thoracoscopic surgery for anatomical lung resection-which is less invasive? J Thorac Dis 2021;13:244-51. [Crossref] [PubMed]
- Nomori H, Ohtsuka T, Horio H, et al. Thoracoscopic lobectomy for lung cancer with a largely fused fissure. Chest 2003;123:619-22. [Crossref] [PubMed]
- Stamenovic D, Bostanci K, Messerschmidt A, et al. Fissureless fissure-last video-assisted thoracoscopic lobectomy for all lung lobes: a better alternative to decrease the incidence of prolonged air leak? Eur J Cardiothorac Surg 2016;50:118-23. [Crossref] [PubMed]
- Igai H, Kamiyoshihara M, Yoshikawa R, et al. The efficacy of thoracoscopic fissureless lobectomy in patients with dense fissures. J Thorac Dis 2016;8:3691-6. [Crossref] [PubMed]
- Craig SR, Walker WS. A proposed anatomical classification of the pulmonary fissures. J R Coll Surg Edinb 1997;42:233-4.
- Igai H, Kamiyoshihara M. Uniportal thoracoscopic fissureless right lower lobectomy using the suction device trick. Multimed Man Cardiothorac Surg 2019; [Crossref]
- Igai H, Furusawa S, Ohsawa F, et al. Application of "suction-guided stapling" during uniportal thoracoscopic major lung resection. Gen Thorac Cardiovasc Surg 2022;70:204-5. [Crossref] [PubMed]
- Refai M, Brunelli A, Salati M, et al. Efficacy of anterior fissureless technique for right upper lobectomies: a case-matched analysis. Eur J Cardiothorac Surg 2011;39:1043-6. [Crossref] [PubMed]
- Ng T, Ryder BA, Machan JT, et al. Decreasing the incidence of prolonged air leak after right upper lobectomy with the anterior fissureless technique. J Thorac Cardiovasc Surg 2010;139:1007-11. [Crossref] [PubMed]
- Igai H, Matsuura N, Kamiyoshihara M. Uniportal thoracoscopic upper division segmentectomy of left upper lobe using a unidirectional anterior approach. Multimed Man Cardiothorac Surg 2020; [Crossref]
- Igai H, Matsuura N, Kamiyoshihara M. Uniportal thoracoscopic right anterior basal (S8) segmentectomy using unidirectional dissection. Multimed Man Cardiothorac Surg 2021; [Crossref]
- Attaar A, Luketich JD, Schuchert MJ, et al. Prolonged Air Leak After Pulmonary Resection Increases Risk of Noncardiac Complications, Readmission, and Delayed Hospital Discharge: A Propensity Score-adjusted Analysis. Ann Surg 2021;273:163-72. [Crossref] [PubMed]
- Konstantinidis K, Woodcock-Shaw J, Dinesh P, et al. Incidence and risk factors for 90-day hospital readmission following video-assisted thoracoscopic anatomical lung resection†. Eur J Cardiothorac Surg 2019;55:666-72. [Crossref] [PubMed]
- Seder CW, Basu S, Ramsay T, et al. A Prolonged Air Leak Score for Lung Cancer Resection: An Analysis of The Society of Thoracic Surgeons General Thoracic Surgery Database. Ann Thorac Surg 2019;108:1478-83. [Crossref] [PubMed]