
Becoming proactive, not reactive: the cardiothoracic surgery job market in the coronavirus disease 2019 (COVID-19), era
Background
The impact of coronavirus disease 2019 (COVID-19) on cardiovascular healthcare delivery extends beyond direct COVID-19 morbidity and mortality (1,2). In the cardiothoracic surgery (CTS) clinical setting, COVID-19 pandemic has contributed to blood bank shortages, reduction in primary prevention screening and counselling for cardiovascular risk factors (i.e., dyslipidemia, diabetes, hypertension, smoking) and thoracic malignancies resulting in advanced disease at time of presentation, surgical backlog of non-emergency cases (e.g., transplant and congenital heart disease), and reallocation of specialized cardiovascular resources including extracorporeal membrane oxygenation and cardiovascular intensive care expertise (1). The COVID-19 pandemic has also affected the CTS research landscape, with considerable reductions in women authorship (3,4), and surgical training, with fewer hands-on training opportunities for students, residents, and fellows (5). One area that remains to be elucidated is the impact of COVID-19 on hiring trends in cardiovascular/cardiothoracic surgery.
Luc et al. (6) explore this topic through a temporal review of the Cardiothoracic Surgery Network (CTSNet) job market database. They found an overall decline in CTS job opportunities during January to May 2020, compared to the same months during pre-pandemic 2019. The reduction of job postings was greatest for cardiovascular/cardiothoracic combined subspecialty, followed by congenital and adult cardiac surgery. Conversely, general thoracic surgery saw a proportional increase in job postings. During the early months of the pandemic, there was also an increase in views per CTS job posting, but a corresponding reduction in monthly curriculum vitae (CV) views, which the authors interpreted as a mismatch between job market supply and demand.
We would like to congratulate Dr. Luc and colleagues for this first-of-its-kind CTS job market analysis using a well-established and societally-supported database to evaluate the impact of COVID-19 on employment. This analysis provides trends in the engagement of both job seekers and recruiters, as well as data by region and CTS subspecialties. From the findings, the article postulates the downstream effects of diminishing CTS job opportunities for upcoming surgical graduates and highlights potential strategies to overcome these challenges during their transition to faculty in the pandemic and post-pandemic era. Innovative analyses such as these are important to plan ahead and meet the needs of our patients and our community: trainees require future job security after training, divisions and departments want a well-staffed team that covers the necessary clinical services and maintains a conducive workplace culture, and institutions want to meet their volumetric demands to best care for their patients as well as empower innovation and research to advance the field.
The effects of the COVID-19 pandemic on the cardiothoracic surgery job market?
Although this job market analysis is unprecedented and highly topical, there are shortcomings associated with study designs of this type. Firstly, the validity of CTSNet data is unclear as it is not subjected to verification or data cleaning. Secondly, CTSNet is heavily North America-centric despite having global participating and member organizations. This is reflected in the geographic distribution of postings, for which granularity in regional variation is only reported for the United States. Indeed, CTSNet is not commonly used by job seekers or recruiters in Canada, and even less so beyond North America. Thirdly, there is a strong bias towards American academic positions in the database, whereas CTSNet lacks external validity as the job market extends beyond virtual platforms. Employment opportunities in CTS are often navigated through less transparent means. Jobs are commonly secured through pre-existing social networks, word-of-mouth, internal postings, and other informal processes (7). Certain jobs on CTSNet may have already been filled at time of listing or drafted with an applicant in mind; however, public listings are required as part of logistical formality. Fourthly, caution should be taken when interpreting job supply and demand based on website viewership. Job seekers may use more than one profile or account, or are not encountering the positions they desire, while the decreased CV views can be explained by sickness leave among recruiters or a shift in the organization’s priorities during the pandemic. As these metrics are not validated, it is unclear what conclusions may be drawn from mere views.
Lastly, with any temporal-based study, there is concern for seasonality of the data. For example, there is expected month-to-month variation, as well as seasonality to the start dates of employment contracts, which can introduce random and systematic error, respectively. Since March 2020 was when COVID-19 was declared a pandemic by the World Health Organization, the decline in job postings seen in January and February 2020 may be considered noise rather than evidence of a drop in non-thoracic job opportunities. This is also not accounting for the turnaround time between declaration of the pandemic and the implementation of changes in human resource management at the hospital level. Assuming March 2020 to be the true start of the pandemic (and changes in longer-term institutional practices and thinking), there are only three months of data that would allow for valid comparison to pre-pandemic 2019. This short timeframe is inadequate to draw robust conclusions about the impact of COVID-19 on job trends. Altogether, the study would thus benefit from further justification for the decision to study January to May as the months of interest, as well as further study with more recent data that have become available since the start of the pandemic.
Mechanisms of job market variability
The COVID-19 pandemic had a two-fold impact on the surgical workforce. Early in the pandemic, there were considerably reduced surgical volumes across the globe as scheduled cases were cancelled to mobilize hospital resources and beds to respond to COVID-19 (8). This resulted in acute workforce needs in terms of non-surgical management, often responded to by surgical personnel (1). Similarly, the increased cardiovascular and lung pathology due to COVID-19, as well as growing waiting lists for other cardiothoracic pathologies, led to subacute and chronic needs for cardiothoracic specialists (9). This may explain why thoracic surgery job posts on CTSNet almost doubled in the authors’ analysis. Nevertheless, the uncertainty of the pandemic also troubled programs’ ability to plan for the future. During the earlier waves, transcatheter and minimally-invasive procedures were more commonly prioritized in order to minimize hospital length of stay and infection risks for patients and health workers (10), both during and after a procedure, whereas future volumetric needs were difficult to predict.
In addition to healthcare crises, the job market varies considerably by both external and specialty-specific factors. Externally, macroeconomic factors can result in hospital-level and governmental changes in hospital budgets, whether due to economic crises, conflict-induced inflation, loss of private funding and philanthropy, or underfunding of health systems. Specialty-specific, it has been widely reported that the CTS workforce is ageing at a rate that is disproportionate to the number of trainees recruited into the specialty, whereby deficits have been projected across North America in the near future (11,12). This may be exacerbated by an ageing patient population, which becomes increasingly vulnerable to CTS pathology, as well as the need to clear the remaining backlog accrued through the pandemic. Furthermore, the transcatheter and minimally invasive surgery era has resulted in a growth of structural heart training opportunities in residency, fellowship, and beyond for (future) cardiac surgeons (13,14), which may influence the number of jobs presented on CTSNet (e.g., more posts on other, more interventional platforms), as well as the diversity of job descriptions. In addition, hospitals have different needs (e.g., changing patient population, departure or retirement of a given subspecialist) which may influence trainees’ fellowship choices to obtain a particular job and present informal ways of recruiting surgeons. Lastly, and most importantly, representation and institutional culture greatly influence job market variability. CTS is known to be underrepresented in terms of sex, gender, race, ethnicity, and Indigeneity relative to the patients and populations we serve (15-17). Thus, job opportunities can vary considerably based on unconscious biases and systemic racism (i.e., fewer opportunities) or active diverse recruiting (i.e., more opportunities). Similarly, the reputed institutional culture can serve as a considerable push or pull factor. For example, a program may be known for its supportive leadership and multidisciplinary collaboration, or associated with multiple reports of bullying and harassment (18).
Way forward: fool-proofing the future cardiothoracic surgery job market
Several actions have already been taken to support current and future CTS job applicants to seek and prepare for jobs (Figure 1). During the pandemic, programs were forced to move towards virtual interviews and networking opportunities (5,19), which were commonly held in-person at conferences or workshops before the pandemic. Many programs have maintained these structures later in the pandemic to reduce barriers for individuals when applying for jobs, such as the ability to take time off and have funds to travel to conferences (5). In addition, the CTS professional network is vast, comprising both of historical formal or informal partnerships between institutions, as well as internal mentorship, sponsorship, and alumni structures of one’s primary (residency) or secondary (fellowship) training program, which often further serve as drivers for job opportunities (7). Indeed, the impact of cardiothoracic surgery on patients and families is immense and surgical team “fit” is important that more informal recruitment, such as recommendations from trusted colleagues and partner institutions, is incredibly common in our specialty. Thus, institutions, through their experience and networks, should proactively support their trainees in such a way, rather than leaving pivotal career transitions in the hands of their graduating trainees or departing surgeons.
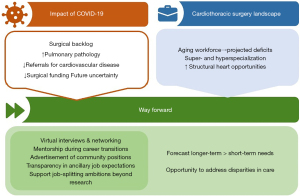
Moving forward, further work is needed to truly foolproof the CTS job market and make it more resilient towards healthcare crises, as well as to ensure greater inclusion within our specialty. First, future needs should be more accurately forecasted rather than only responded to acutely when gaps become apparent. This includes an evaluation of growing subacute and chronic disease burdens, the ageing workforce, and changing skillsets in today’s procedural landscape. This will require hospitals to better engage workforce representatives, which have a different perspective compared to departmental leadership and hospital administrators, and patients, to ensure their care needs are met. In turn, societies must serve their membership and take a leading role in studying trends in the CTS workforce. They ought to engage in advocacy surrounding existing disparities and mismatch in the specialty, which extends far beyond the pandemic. Lastly, programs should consider greater flexibility in individuals’ non-primary commitments (i.e., job splitting). Luc et al. (6) found that 60% of job posts pertained to academic positions of which 40-50% carry research expectations. Programs may consider facilitating surgeons to engage in activities other than research should they prefer this, whether clinical (e.g., intensive care, global surgery) or non-clinical (e.g., administration, education, entrepreneurship). This ensures that surgeons feel empowered rather than burdened and may facilitate recruitment, retainment, and job satisfaction with downstream effects on clinical care, trainee education, and workplace culture.
Conclusions
The pandemic is not over, but cardiovascular and cardiothoracic surgical volumes have almost returned to pre-pandemic volumes. Nevertheless, opposing challenges exist and persist in the cardiothoracic surgical workforce: our specialty is faced with too many graduates (e.g., in Canada and after congenital heart surgery fellowship) relative to the job opportunities that are available or created, women and minoritized individuals remain considerably underrepresented, and the workforce is ageing with projected shortages in actively working surgeons. While the pandemic’s impact on our specialty is slowly fading, it is paramount for our specialties to be proactive rather than reactive for our patients because our specialty depends on it.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Thoracic Disease. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1412/coif). DV is supported by the Canadian Institutes of Health Research (CIHR) Vanier Canada Graduate Scholarship, outside this manuscript. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Vervoort D, Luc JGY, Percy E, et al. Assessing the Collateral Damage of the Novel Coronavirus: A Call to Action for the Post-COVID-19 Era. Ann Thorac Surg 2020;110:757-60. [Crossref] [PubMed]
- Percy E, Luc JGY, Vervoort D, et al. Post-Discharge Cardiac Care in the Era of Coronavirus 2019: How Should We Prepare? Can J Cardiol 2020;36:956-60. [Crossref] [PubMed]
- Ma X, Vervoort D, Babar MS, et al. Vascular Surgery Research in the Coronavirus Disease 2019 Pandemic: A Sex-Based Bibliometric Analysis. Am Surg 2022; Epub ahead of print. [Crossref]
- Elfaki LA, Luc JGY, Antonoff MB, et al. Sex differences in authorship in cardiothoracic surgery during the early coronavirus disease 2019 pandemic. JTCVS Open 2022;11:265-71. [Crossref] [PubMed]
- Vervoort D, Dearani JA, Starnes VA, et al. Brave New World: Virtual conferencing and surgical education in the Coronavirus Disease 2019 era. J Thorac Cardiovasc Surg 2021;161:748-52. [Crossref] [PubMed]
- Luc JGY, Pizano A, Udwadia F, et al. Early effect of the COVID-19 pandemic on the North American cardiothoracic surgery job market. J Thorac Dis 2022;14:3304-13. [Crossref] [PubMed]
- Sterbling HM, Molena D, Rao SR, et al. Initial report on young cardiothoracic surgeons' first job: From searching to securing and the gaps in between. J Thorac Cardiovasc Surg 2019;158:632-641.e3. [Crossref] [PubMed]
- Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg 2020;107:1440-9. [Crossref] [PubMed]
- Tam DY, Qiu F, Manoragavan R, et al. The Impact of the COVID-19 Pandemic on Cardiac Procedure Wait List Mortality in Ontario, Canada. Can J Cardiol 2021;37:1547-54. [Crossref] [PubMed]
- Vervoort D, Nguyen TC. Commentary: Coronary artery bypass grafting in patients with coronavirus disease 2019 (COVID-19): Darkness cannot drive out darkness. J Thorac Cardiovasc Surg 2020;160:e197-8. [Crossref] [PubMed]
- Ouzounian M, Hassan A, Teng CJ, et al. The cardiac surgery workforce: a survey of recent graduates of Canadian training programs. Ann Thorac Surg 2010;90:460-6. [Crossref] [PubMed]
- Vanderby SA, Carter MW, Latham T, et al. Modeling the cardiac surgery workforce in Canada. Ann Thorac Surg 2010;90:467-73. [Crossref] [PubMed]
- Tam DY, Makhdoum A, Ouzounian M, et al. The state of transcatheter aortic valve implantation training in Canadian cardiac surgery residency programs. Can J Surg 2018;61:418-23. [Crossref] [PubMed]
- Muller Moran HR, Maurice-Ventouris M, Alharbi M, et al. Pan-Canadian initiative on Fundamental Competencies for Transcatheter Cardiac Surgery: A modified Delphi consensus study. J Thorac Cardiovasc Surg 2021; Epub ahead of print. [Crossref]
- Gao SW, Forcillo J, Watkins AC, et al. 60 Years After the First Woman Cardiac Surgeon: We Still Need More Women in Cardiac Surgery. CJC Open 2021;3:S89-94. [Crossref] [PubMed]
- Yanagawa B, Servito M, Osler FG, et al. Declaration of Values, Vision and Approaches from the Canadian Society for Cardiac Surgery Taskforce on Equity, Diversity, and Integration. Can J Cardiol 2022;38:828-31. [Crossref] [PubMed]
- Vervoort D, Kimmaliardjuk DM, Ross HJ, et al. Access to Cardiovascular Care for Indigenous Peoples in Canada: A Rapid Review. CJC Open 2022;4:782-91. [Crossref] [PubMed]
- Gianakos AL, Freischlag JA, Mercurio AM, et al. Bullying, Discrimination, Harassment, Sexual Harassment, and the Fear of Retaliation During Surgical Residency Training: A Systematic Review. World J Surg 2022;46:1587-99. [Crossref] [PubMed]
- Rabenstein AP. An Applicant's Perspective on Virtual Interviews-Do's and Don'ts. Ann Thorac Surg 2022;114:356. [Crossref] [PubMed]


