
The clinical journey of patients with a severe exacerbation of chronic obstructive pulmonary disease (COPD): from the ambulance to the emergency department to the hospital ward
Introduction
Exacerbations of chronic obstructive pulmonary disease (COPD) are acute complications which cause significant morbidity and mortality for patients and often require emergency management in the ambulance, emergency department (ED) and hospital setting. The literature of COPD exacerbations is expanding rapidly and there are comprehensive national and international clinical guidelines including the COPD-X Plan and the GOLD Report (1,2). Whilst this literature is extensive, there are only a handful of studies and reviews which have linked aspects of the emergency healthcare pathway for exacerbations (3-8).
The pre-hospital and emergency management of COPD exacerbations involves a body of literature that is rapidly expanding. To date, there are only a small number of 0studies which examine the entire emergency healthcare pathway for these patients, from the ambulance to the ED to the hospital ward. The aims of this study were to address this gap in knowledge and provide important information about the epidemiology of COPD patients accessing this emergency healthcare pathway, as well as predictive factors for healthcare outcomes. This research has focused on the problems of overwhelming medical burden, difficulties in rapid and correct identification, irregular treatment measures, and poor prognosis in COPD patients. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-328/rc).
Methods
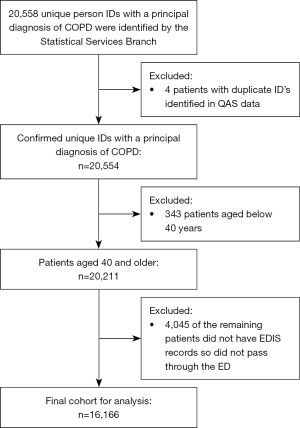
This is a retrospective observational study of patients aged 40 and above who presented to an ED in Queensland and received either an ED or hospital principal diagnosis of COPD in 2015 and 2016 (ICD-10-AM code of J44.0, J44.1, J44.8, or J44.9). Administrative patient record data were separately extracted from the Queensland Ambulance Service (QAS), Emergency Department Information System (EDIS), Queensland Hospital Admitted Patient Data Collection (QHAPDC) and Death Registry and linked to provide a comprehensive picture of the emergency pathway for patients experiencing an exacerbation of COPD (See Figure 1). The linkage was performed by the Statistical Services Branch of Queensland Health, who created unique patient identifiers (ID) to facilitate the de-identification of the data. There were three primary outcomes for the study: admission (greater than one admission or episode of ongoing vs one admission or less); hospital length of stay (LOS) (weighted average or lower than weighted average LOS vs. greater than weighted average LOS); and mortality (yes/no). The secondary endpoints were re-presentation to an ED within 48 hours and 30 days.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committees of The Prince Charles Hospital (No. HREC/17/QPCH/221) and The University of Queensland (No. 2017002067) and individual consent for this retrospective analysis was waived.
Statistical analyses
Statistical analyses were completed using SPSS (version 26, IBM, New York, USA). Univariate descriptive analyses were completed to identify trends and data discrepancies. The data for each patient were considered across the entire two-year study period and analyses of demographic characteristics were completed at a per-patient level to identify epidemiological and demographic factors and trends. The data were then analysed at a per-visit level to measure factors related to individual healthcare episodes.
Three separate multivariate logistic regression models were constructed for the three primary outcomes (admission or ongoing care, average admission LOS and mortality). For each outcome, a series of univariate regression analyses were first conducted to identify variables of interest. The multivariate regression model was then created containing all variables that were significantly associated with the outcome in the univariate analyses [i.e., 95% confidence interval (CI) not including 1.0, P<0.05]. Any variables that were not significant in the first multivariate model were then removed from the model one at a time, and the impact on the remaining variables examined. If no changes were observed to the odds ratios beyond 10% of any of the other variables, the variable was permanently removed from the model, otherwise, it was retained. Interactions were also assessed for each of the three multivariate models.
Results
Demographics
In total, 16,166 individual patients aged forty years or older presented to a Queensland ED and received either an ED or hospital principal diagnosis of COPD between 1 January 2015 and 31 December 2016. These patients had a combined total of 29,332 emergency healthcare episodes for COPD. Gender distribution was similar, with 8,209 (51%) male and 7,955 (49%) female. Patient age was received from the data custodians in five-year age groups due to de-identification requirements, and the median age fell within 70 to 74 years age group. Table 1 shows the characteristics of the patients in this study.
Table 1
| Characteristics | N=16,166 [%] |
|---|---|
| Sex | |
| Male | 8,209 [51] |
| Female | 7,955 [49] |
| Indeterminant | 2 [0] |
| Age (≥40), years | |
| 40–59 | 2,855 [18] |
| 60–69 | 4,097 [25] |
| 70–79 | 5,243 [32] |
| 80+ | 3,971 [25] |
| Aboriginal or Torres Strait Islander status | |
| Aboriginal but not Torres Strait Islander | 904 [5.6] |
| Torres Strait Islander but not Aboriginal | 93 [0.6] |
| Both Aboriginal and Torres Strait Islander | 47 [0.3] |
| Not Aboriginal or Torres Strait Islander | 15,111 [93.5] |
| Current marital status | |
| Married or de facto relationship | 7,493 [46] |
| Divorced or separated | 3,162 [20] |
| Widowed | 2,991 [19] |
| Never married | 1,765 [11] |
| Unknown | 624 [4] |
| Region of birth | |
| Australia | 12,201 [76] |
| United Kingdom | 1,675 [10] |
| New Zealand | 789 [5] |
| Other | 1,501 [9] |
| First language | |
| English | 15,094 [93] |
| Other | 263 [2] |
| Unknown | 809 [5] |
| Home state | |
| Queensland | 15,752 [97] |
| New South Wales | 160 [1] |
| Victoria | 94 [1] |
| Other | 160[1] |
| Smoking status | |
| Current smoker | 5,835 [36] |
| Former smoker | 5,767 [36] |
| Smoking status not recorded | 4,564 [28] |
| Comorbidities | |
| 0–1 comorbidity | 1,633 [10] |
| 2–4 comorbidities | 4,140 [26] |
| 5–9 comorbidities | 5,052 [31] |
| ≥10 comorbidities | 4,300 [27] |
| Unknown | 1,041 [6] |
| Top comorbidities | |
| Hypertension | 5,377 [4] |
| Asthma | 3,847 [3] |
| Type 2 diabetes mellitus | 3,282 [3] |
| Heart failure | 2,645 [3] |
| Pneumonia | 2,259 [2] |
| Ischaemic heart disease | 2,248 [2] |
| Hypercholesterolaemia | 2,157 [2] |
These patients had a significant comorbidity burden with the most common comorbidities found to be hypertension, asthma, type 2 diabetes mellitus and heart failure. Furthermore, 11,602 (72%) patients reported a smoking history, with 5,835 (36%) reporting they were current smokers.
Predictive factors for the primary outcomes
The primary outcomes of this study were admission, hospital LOS and mortality for patients who presented to the ED with exacerbations of COPD. The multivariate regression analysis identified various pre-hospital, ED and admission predictive factors associated with the three primary outcomes.
Firstly, a number of variables were associated with more than one admission during the two year study period, after adjusting for known confounders (Table 2). Patients with more than one ambulance transportation during the study period were 22 times more likely to have more than one admission (95% CI: 17.9–28.5). Other significant predictors included having more than 10 comorbidities [odds ratio (OR) 4.3, 95% CI: 3.1–5.8], and being a current or past smoker (OR 2.3, 95% CI: 1.9–2.7). Patients who were administered oxygen therapy (OR 1.3, 95% CI: 1.1–1.5), ipratropium bromide (OR 1.4, 95% CI: 1.2–1.7) or adrenaline (OR 2.3, 95% CI: 1.2–4.3) in the prehospital setting, were more likely to be admitted to hospital more than once during the 2-year study period. Finally, patients with a discrepancy between the ED and hospital principal diagnosis were 2.3 times more likely to have greater than one admission (OR 2.3, 95% CI: 2.0–2.6). Other significant variables for more than one admission included having greater than two healthcare episodes triaged as resuscitation or emergency and having an ED LOS of 4 to 8 hours.
Table 2
| Variables | OR (95% CI) | ||
|---|---|---|---|
| Model 1: greater than one admission or episode of ongoing care | Model 2: LOS >3.6 days |
Model 3: mortality |
|
| Gender | |||
| Male | Reference | Reference | |
| Female | 1.2 (1.1–1.3) | 0.7 (0.6–0.8) | |
| Age, years | |||
| 40–59 | Reference | Reference | |
| 60–69 | 1.3 (1.2–1.5) | 1.8 (1.5–2.2) | |
| 70–79 | 1.5 (1.3–1.7) | 2.2 (1.9–2.7) | |
| 80+ | 1.6 (1.4–1.8) | 3.7 (3.0–4.5) | |
| Indigenous status | |||
| Not Aboriginal or Torres Strait Islander | Reference | ||
| Aboriginal or Torres Strait Islander | 0.8 (0.7–0.9) | ||
| Relationship status | |||
| Married/DeFacto | Reference | Reference | |
| Widowed | 1.0 (0.9–1.1) | 1.2 (1.0–1.3) | |
| Never married | 1.1 (1.0–1.3) | 1.1 (0.9–1.3) | |
| Divorced/separated | 1.1 (1.0–2.3) | 1.1 (1.0–1.3) | |
| Department of Veteran’s Affairs | |||
| No | Reference | Reference | |
| Yes | 0.6 (0.5–0.8) | 1.5 (1.2–1.8) | |
| Smoking status | |||
| No smoking recorded | Reference | Reference | |
| Smoking history | 2.3 (1.9–2.7) | 0.7 (0.6–0.8) | |
| Current smoker | 2.3 (1.9–2.7) | 0.7 (0.6–0.8) | |
| Comorbidities | |||
| 0–1 | Reference | Reference | Reference |
| 2–4 | 1.6 (1.2–2.1) | 2.5 (2.1–3.1) | 1.5 (1.2–1.9) |
| 5–9 | 2.5 (1.2–2.0) | 6.5 (5.3–7.8) | 2.8 (2.3–3.6) |
| 10+ | 4.3 (3.1–5.8) | 22.1 (18.1–27.2) | 5.3 (4.2–6.8) |
| Ambulance use | |||
| No ambulance trips | Reference | Reference | |
| 1 ambulance trip | 0.6 (0.5–0.7) | 0.4 (0.3–0.5) | |
| >1 ambulance trips | 22.6 (17.9–28.5) | 0.2 (0.2–0.3) | |
| QAS dispatch criticality | |||
| No dispatch code 1 | Reference | ||
| 1 or more dispatch code 1 | 0.9 (0.8–1.0) | ||
| Retrieval | |||
| No aircraft retrievals | Reference | ||
| At least one aircraft retrieval | 2.5 (1.6–4.0) | ||
| QAS final assessment COPD | |||
| No | Reference | Reference | |
| Yes | 1.2 (1.1–1.3) | 1.6 (1.4–1.8) | |
| Pre-hospital oxygen | |||
| No | Reference | Reference | Reference |
| Yes | 1.3 (1.1–1.5) | 1.5 (1.3–1.6) | 1.6 (1.5–1.8) |
| Pre-hospital salbutamol | |||
| No | Reference | ||
| Yes | 0.7 (0.6–0.8) | ||
| Pre-hospital ipratropium bromide | |||
| No | Reference | Reference | |
| Yes | 1.4 (1.2–1.7) | 1.2 (1.1–1.3) | |
| Pre-hospital adrenaline | |||
| No | Reference | ||
| Yes | 2.3 (1.2–4.3) | ||
| ED LOS, hours | |||
| <4 | Reference | Reference | |
| 4–8 | 1.5 (1.3–1.7) | 1.2 (1.1–1.3) | |
| >8 | 1.2 (1.0–1.4) | 1.1 (1.0–1.2) | |
| Health care episodes | |||
| 1 | Reference | Reference | |
| 2 | 1.0 (0.9–1.1) | 0.9 (0.8–1.1) | |
| >2 | 1.3 (0.9–2.0) | 1.5 (1.0–2.3) | |
| Health care episode type | |||
| No complex episodes | Reference | ||
| At least one complex episode | 1.7 (1.3–2.1) | ||
| ED triage | |||
| 1–2 Episodes triaged as ‘Resus’ or ‘Emergency’ | Reference | Reference | |
| >2 Episodes of ‘Resus’ or ‘Emergency’ | 0.5 (0.4–0.8) | 0.5 (0.3–0.8) | |
| Discrepancy between ED and hospital principal diagnosis | |||
| No discrepancy | Reference | Reference | Reference |
| Discrepancy | 2.3 (2.0–2.6) | 1.2 (1.1–1.3) | 1.1 (1.0–1.3) |
QAS, Queensland Ambulance Service; COPD, chronic obstructive pulmonary disease; ED, emergency department; LOS, length of stay; OR, odds ratio.
The final multivariate model for the second outcome of above weighted average LOS (average LOS >3.6 days) demonstrated some notable associations with predictive factors (Table 2). Firstly, there was a strong association with patients who had greater than 10 comorbidities and a longer average LOS (OR 22, 95% CI: 18.0–27.2). Additionally, patients who required aircraft transfer, who had complex healthcare episodes or who had oxygen therapy in the ambulance had an increased odds of longer admissions (OR 2.5, 95% CI: 1.6–4.0; OR 1.7, 95% CI: 1.3–2.1, OR 1.4, 95% CI: 1.3–1.6, respectively). Other significant variables for above average LOS were female sex, increasing age, being divorced or separated, having a paramedic final assessment of COPD, and ipratropium administration in the ambulance. Being Aboriginal or Torres Strait Islander, having Department of Veterans’ Affairs funding, increasing ambulance trips and greater than two episodes triaged as resuscitation or emergency had reduced associations with increased average LOS.
Finally, there were a number of variables with notable associations for the outcome of mortality (see Table 2). Firstly, patients who had greater than 10 comorbidities were 5 times more likely to die in the two-year period (95% CI: 4.2–6.8). Additionally, patients aged 80 or older or patients with Department of Veterans’ Affairs funding had increased odds ratio for mortality of 3.7 (95% CI: 3.0–4.5) and 1.5 (95% CI: 1.2–1.8) respectively. Oxygen therapy in the ambulance had an odds ratio of 1.6 (95% CI: 1.5–1.8) and patients who paramedics determined had COPD as their final assessment also had an odds ratio of 1.6 (95% CI: 1.4–1.8) for increased mortality. Female sex, smoking, having at least one dispatch criticality of 1, having greater than two ED episodes triaged as resus or emergency, and salbutamol delivery in the ambulance were all variables associated with reduced associations with mortality.
Interactions were tested for clinically significant pairs of variables for each of the multivariate models. Firstly, the interaction term between age and number of comorbidities was significant for the outcome of mortality. Secondly, the interaction terms for number of comorbidities versus number of ambulance trips were significant for both the outcomes of greater than one admission and increased average LOS. These findings suggest possible effect modification for the predictive factors on these outcomes.
Other pertinent results
Prehospital results
The majority of ED presentations (20,307/29,332, 69%) required ambulance transport and these involved 11,588 patients. Of the patients with ambulance presentations, (31% 9,594/11,588) required more than one presentation in the two-year period and 769 (7%) required three or greater trips in that time. Ambulance patients also had a high comorbidity burden (Table 3). These ambulance presentations were primarily given a dispatch criticality of Code 1 (16,509, 89%), indicating that the case was of high acuity and allowing paramedics to travel with lights and sirens as required.
Table 3
| Number of comorbidities | Frequency | Percent % |
|---|---|---|
| ≥10 comorbidities | 4,106 | 35 |
| 5–9 comorbidities | 4,342 | 37 |
| 2–4 comorbidities | 2,605 | 23 |
| 0–1 comorbidity | 531 | 5 |
| Total | 11,584 | 100 |
| Missing | 4 | <1 |
| Total | 11,588 | 100 |
QAS, Queensland Ambulance Service.
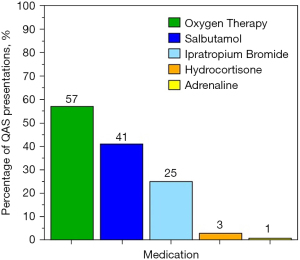
Medications were delivered in the majority of ambulance presentations (14,966, 74%) and oxygen therapy was given in more than half (11,537, 57%). Patients received salbutamol and ipratropium bromide in 8,424 (41%) and 5,018 (25%) of presentations, respectively (Figure 2).
The most common final assessments assigned by paramedics for ambulance presentations were shortness of breath (6,196, 31%), chest infections (3,970, 20%), COPD (2,998, 15%), asthma (1,310, 7%) and pain (952, 5%), with the remaining (4,881, 22%) presentations involving other miscellaneous conditions.
A number of clinical parameters were captured in the ambulance data including medications delivered in the ambulance (Figure 2) and patient observations (Table 4). It was found that these patients had generally deranged observations with tachypnoea, tachycardia, hypertension and hypoxia. 19,207 presentations (97%) involved patients with a Glasgow Coma Scale (GCS) of 15 with the remaining 767 (3%) having some extent of altered level of consciousness.
Table 4
| Clinical parameters | Mean | Median | Standard deviation | Minimum | Maximum |
|---|---|---|---|---|---|
| Initial respiratory rate | 27 | 25 | 8 | 0 | 80 |
| Initial SpO2 reading | 90% | 92% | 8% | 24% | 100% |
| Final SpO2 reading | 96% | 96% | 3% | 41% | 100% |
| Change in SpO2 across presentation | +5% | +3% | 7% | −55% | +73% |
| Initial heart rate | 99 | 99 | 20 | 0 | 212 |
| Initial systolic blood pressure | 145 | 142 | 27 | 30 | 260 |
SpO2, blood oxygen saturations.
In over half of the pre-hospital presentations (9,690/17,127, 57%) where patients had a final oxygen saturation of greater than 92%, supplemental oxygen was administered in the ambulance. Of note, for patients who were administered salbutamol in the ambulance, the median final oxygen saturation was 97% with an average change in saturation of +5% during the presentation. For patients who received both bronchodilators, the median final oxygen saturation was 97% with an average change of +8%.
ED results
In the ED, 19,890 (68%) patients had a principal diagnosis of COPD, with the top five alternative diagnoses being pneumonia, acute lower respiratory infection, asthma, heart failure or dyspnoea unspecified. The EDs with the most frequent presentations for COPD were Logan Hospital, the Gold Coast University Hospital, The Prince Charles Hospital, Ipswich Hospital and Caboolture Hospital, all classified as serving a major city population.
The ED median LOS was 4 hours 7 minutes with an interquartile range of 3 hours 41 minutes. The majority of COPD presentations were triaged as ‘Emergency’ (9,806, 33%) or ‘Urgent’ (15,987, 54%), with 956 (3%) triaged for ‘Resuscitation’ and the remaining 2,591 (10%) triaged as ‘Semi-Urgent’ or ‘Non-Urgent’.
Of the ED presentations, 25,136 (86%) received ongoing care including hospital, short stay or ED admission or inter-hospital transfer and 3,953 (14%) were discharged (Table 5). Patients brought in by ambulance were more frequently admitted (90% admission rate), compared with 75% admission rate for patients who were not brought in by ambulance.
Table 5
| Episode end status | Frequency | Percent |
|---|---|---|
| Admitted | 19,497 | 66.5 |
| Admitted to a short stay unit | 4,293 | 14.6 |
| Discharged (ED service event completed) | 3,953 | 13.5 |
| Transferred to another hospital | 759 | 2.6 |
| Admitted to observation ward | 421 | 1.4 |
| Left at own risk after treatment commenced | 161 | 0.5 |
| Other—admitted but no QHAPDC record | 106 | 0.4 |
| Admitted to the emergency department/service | 58 | 0.2 |
| Did not wait | 30 | 0.1 |
| Died in the emergency department | 52 | 0.2 |
| Returned to hospital in the home | 1 | 0.0 |
| Admitted to hospital in the home service | 1 | 0.0 |
| Total | 29,332 | 100.0 |
ED, emergency department; QHAPDC, Queensland Hospital Admitted Patient Data Collection.
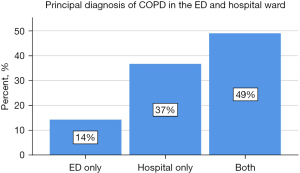
Admission factors
Most presentations had a hospital admission principal diagnosis of COPD (21,486, 85%), with the remaining admissions having a principal diagnosis of COPD in the ED only (Figure 3).
For patients who were admitted or received ongoing care, the median LOS was 1.9 days and an interquartile range of 3.9 days. The weighted average LOS for individual patients was 3.6 days with a standard deviation of 4 days. A number of presentations (0.5%) involved complex and severe disease requiring intensive care unit (ICU) admission, with these patients having a median ICU stay of 2.5 days with an interquartile range of 4 days, and 202 presentations involved ventilator support. On discharge, patients primarily returned to their home or usual residence.
Representations
Time to representation following ED or hospital discharge was a median of 38 days, with an interquartile range of 110 days. Of discharged patients, 720 (5%) had at least one representation for COPD within 48 hours of discharge and 2,517 (16%) patients had at least one representation for COPD within 30 days. Of the ambulance cases, 628 (3%) resulted in representation for COPD within 48 hours of discharge after either an ED stay or an admission. For presentations discharged from the ED, 389 (10%) had a representation within 48 hours and 1,025 (30%) had representation for COPD within 30 days. These figures were greater than presentations discharged from hospital, with 557 (2%) resulting in representation for COPD within 48 hours and 4,196 (17%) resulting in representation for COPD within 30 days.
Death registry data
Of this COPD cohort, 2,938 (18%) patients died during the two-year period. Of these patients who died, 45% had COPD listed as a primary cause of death and 25% as a secondary cause of death. Respiratory failure was listed on 1% of death certificates and the remainder had other causes listed. The median age of death fell within the age group 75 to 79 years old. Hospitals were the most commonly recorded place of death (1,840/2,938, 63%) compared with other places of death.
Discussion
The results of this study have demonstrated that exacerbations of COPD place substantial demand on ambulance services, EDs and hospitals in Queensland. The primary outcomes of hospital admission, hospital LOS and mortality were found to be considerable and significant. Furthermore, patients experiencing exacerbations in Queensland tend to be older and have a significant comorbidity burden. These patients most frequently present to the ED by ambulance and the majority receive oxygen or other treatment in the ambulance. On arrival to Queensland EDs, COPD patients have high acuity and are frequently triaged for rapid review. Following ED management, patients experiencing an exacerbation of COPD have high admission rates, and even higher rates for those brought in by ambulance. Once discharged, COPD patients have high rates of representation within 48 hours or 30 days, particularly those patients discharged from the ED. Generally, predictive factors for poorer healthcare outcomes, including more admissions, increased lengths of stay and mortality, were found to be larger comorbidity burden, requiring frequent ambulance presentations and having at least one episode requiring oxygen delivery in the ambulance.
Patient characteristics
The demographic characteristics of these patients with COPD, including age, sex, indigenous status, country of birth, first language and marital status all align with the findings of similar studies in Australia (5,9,10).
The majority of patients had a significant comorbidity burden, especially patients accessing ambulance services, with the multivariate analyses indicating that increased number of comorbidities was associated with greater odds of having more than one admission in the 2-year period, longer than average LOS, and all-cause mortality. These findings indicate a significant opportunity for clinicians in the pre-hospital and emergency domain to identify patients with COPD with multiple comorbidities as high risk for negative outcomes. In the ED, it is recommended that patients with multimorbidity have early assessment by relevant specialties to determine the pathway and specialty team for admission.
Current smoking and smoking history each had a two-fold increase in risk of admissions in the multivariate analysis. Of note, 36% of this COPD cohort who present for emergency treatment identified as current smokers, a prevalence that is three times that of the general population (12%) (11). This represents a significant opportunity for ambulance and ED clinicians to intervene with smoking cessation counselling in the emergency setting.
Prehospital factors
The majority of patients with exacerbations of COPD in Queensland are transported to the ED by ambulance, with most requiring frequent trips across the two-year period. A small proportion of these patients required significant use of ambulance services with greater than ten trips in that period. For patients with COPD, having an increased number of ambulance presentations was strongly associated with having more than one admission and greater than average LOS, likely demonstrating clinical severity of these presentations.
Many COPD patients (57%) who present to the ED by ambulance in Queensland received oxygen in the ambulance, and overall, 48% of patients transported by ambulance had a final oxygen saturation greater than the 92%. For many of these patients, if they were breathing room air or were not carbon-dioxide retainers, higher saturations would be appropriate, however it is likely that a proportion of these were at risk of hypercapnic respiratory failure. This likely reflects the known diagnostic difficulties in the pre-hospital setting and it is recommended that more research into this area be conducted to further clarify oxygen use in the pre-hospital settings, as well as to identify ways to assist paramedics with differentiating COPD patients. One such method is for ED and hospital clinicians to consistently provide COPD action plans to patients which identify those at risk from high flow oxygen delivery and to educate patients to flag their COPD action plan with paramedics when they require ambulance transport.
In the pre-hospital setting, salbutamol was administered in 41% of presentations, ipratropium bromide in 25% indicating a significant proportion of patients are given bronchodilators prior to ED arrival. Further research is required into the delivery of medications in the pre-hospital setting and how these affect outcomes for patients with COPD.
ED factors
Patients with COPD presenting to the ED had a high acuity as indicated by the assigned triage categories, with over one-third triaged as ‘Resuscitation’ or ‘Emergency’ and over half triaged as ‘Urgent’. Queensland state data indicates that for patients triaged as ‘Resuscitation’ in Queensland, COPD was the second most common diagnosis following myocardial infarction as the most common (12).
In this study, 68% of patients had an ED principal diagnosis of COPD with the other 32% receiving a hospital diagnosis of COPD once admitted. Often the discrepancy between ED and hospital involved ED diagnoses such as respiratory failure, with a hospital diagnosis of COPD, therefore not representing a misdiagnosis, but the appropriate differentiation of a patient given further investigation and treatment on the ward. Of note however, a discrepancy between ED and hospital principal diagnoses was associated with two-fold increase in odds of greater than one admission, likely representing complicated COPD presentations and multifactorial presentations with multisystem disease. These findings demonstrate that patients who present to the ED with an exacerbation of COPD are high acuity and often present in a complex manner with comorbid conditions. More studies are required to explore the presentation and severity of COPD in the ED as well as diagnostic and early management factors.
Admission factors
Following emergency management, admission rates for patients with COPD were high, with 86% receiving ongoing care in hospital, and 14% being discharged. Patients brought in by ambulance had even higher admission rates of 90% compared with 75% for patients who arrived at the ED via other means. These rates of hospitalisation are much higher than the overall admission rate of 35% for all patients presenting to an ED in Queensland in 2016–2017 (13). These figures indicate the significant clinical burden of patients with COPD exacerbations requiring hospital admission for ongoing acute management following their ED presentation.
The study revealed a number of important findings regarding patterns of admission for COPD exacerbations. Firstly, the hospitals with the most admissions were also the hospitals with the most ED presentations for COPD. These were inner city hospitals likely reflecting population density in these areas. For patients who were admitted or received ongoing care, the median LOS was 1.9 days (interquartile range of 3.9 days), which was generally shorter than a LOS of more than 4 days identified in other studies of COPD patients (5,14-16). A small number of presentations (0.5%) involved ICU admission, with these patients having a median ICU stay of 2.5 days (17). These figures highlight the severe and critical nature of many COPD exacerbations and more research is required into the predictive factors and outcomes for patients requiring critical care in ICU.
Representations
Patients in this study were more likely to represent to an ED for their COPD within 48 hours or 30 days of discharge if they were discharged from an ED compared with discharge following hospital admission. This finding likely indicates that patients experiencing a COPD exacerbation have complex disease and often require more definitive care than emergency management. Furthermore, these representation findings may also indicate that there is a lack of community healthcare supports for these patients, many of whom do not need full hospital admission, but who may require some form of ongoing healthcare or support. It is recommended that further research be conducted in this area to identify causes of representation as well as to investigate possible solutions to representation rates. Possible solutions may lie in programs such as hospital in the home (HITH), which provide ongoing community-based care for patients who do not necessarily require hospital admission.
Death registry factors
The 2,938 deaths in the cohort represented 3.5% of the 58,034 deaths in Queensland in 2015 and 2016 (12). These findings indicate that for most patients, COPD contributes substantially to their mortality and places increased requirement on hospital services for care of patients with advanced lung disease, including end-of-life care. More research is required into factors leading to COPD mortality, and also improvements to practice for clinicians and hospital systems to best support patients with end-stage COPD.
Limitations
The use of administrative data was central to this study design, which was selected to address questions at the state-wide level about patients presenting for emergency management of their COPD. Access to this data allowed for analysis of a significant number of unique parameters including demographic, clinical and admission factors in the ambulance, ED and hospital domain. Despite the advantages of using administrative data in this way, there are a number of limitations to the findings and conclusions of this type of study. Firstly, a major limitation involves the collection of the data, which is most often entered directly into online systems by clinicians, at the time of presentation, as is the case for the ambulance and ED records, or retrospectively collected by health coding teams from patient medical records. This meant that the researchers involved in this study did not have any influence over the parameters that were collected or the accuracy of the coding or data collection. Additionally, the variables are fixed and researchers are restricted to the variables available without influence over study parameters. One example in this case was the age of patients being in age groups rather than actual age or date of birth, due to additional privacy requirements for the state-government data. Finally, another limitation was that no lung function data was available or other data such as medications delivered in the ED. To counter these limitations, further prospective studies involving tailored data collection tools are required to examine predictive factors for hospital admission in patients with exacerbations of COPD, in a more sophisticated and robust manner.
Conclusions
In conclusion, exacerbations of COPD require significant emergency pre-hospital response in Queensland. There were a number of predictive factors identified that were associated with adverse health outcomes for these patients that may assist clinicians and policymakers working in these domains. Patients with COPD are older, have extensive comorbid burden of disease, access emergency services frequently, often present with high acuity and require extensive healthcare management. These patients most often use ambulance services to get to the ED and receive important healthcare interventions from paramedics including early assessment, oxygen therapy and appropriate medications. Of patients presenting by ambulance, 90% are admitted for ongoing treatment. There were a number of factors associated with poorer health outcomes such as increased admissions, increased lengths of stay and mortality. These factors primarily were higher numbers of comorbidities, frequent ambulance presentations and need for prehospital administration of oxygen therapy. Larger prospective studies are required to further examine predictive factors for hospital admission after ED presentation and identify reversible factors early in the clinical pathway to minimise adverse outcomes for patients with COPD presenting to EDs.
Acknowledgments
This study was completed as a Masters of Philosophy research project by Dr. Emily Sneath through the University of Queensland. The results of this study and those presented in this paper also form part of the thesis completed for the Masters degree. We sincerely thank the data-custodians of the Statistical Services Branch of Queensland Health for the provision of data, and the Queensland Ambulance Service research department including Ms Jamie Quinn for early support in this project.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-328/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-328/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-328/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-328/coif). IAY serves as an unpaid editorial board member of Journal of Thoracic Disease. KMF serves as an unpaid Associate Editor-in-Chief of Journal of Thoracic Disease from February 2021 to January 2023. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committees of The Prince Charles Hospital (No. HREC/17/QPCH/221) and The University of Queensland (No. 2017002067) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yang IA, George J, McDonald CF, McDonald V, O’Brien M, Smith B, Zwar N, Dabscheck E. The COPD-X Plan: Australian and New Zealand Guidelines for the management of Chronic Obstructive Pulmonary Disease 2021. Version 2.63, February 2021.
- Global initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2020 Report) 2020. Available online: https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf
- Considine J, Botti M, Thomas S. Emergency department management of exacerbation of chronic obstructive pulmonary disease: audit of compliance with evidence-based guidelines. Intern Med J 2011;41:48-54. [Crossref] [PubMed]
- Tang CY, Taylor NF, McDonald CF, et al. Level of adherence to the GOLD strategy document for management of patients admitted to hospital with an acute exacerbation of COPD. Respirology 2014;19:1191-7. [Crossref] [PubMed]
- Gerber A, Moynihan C, Klim S, et al. Compliance with a COPD bundle of care in an Australian emergency department: A cohort study. Clin Respir J 2018;12:706-11. [Crossref] [PubMed]
- Williams TA, Finn J, Fatovich D, et al. Paramedic Differentiation of Asthma and COPD in the Prehospital Setting Is Difficult. Prehosp Emerg Care 2015;19:535-43. [Crossref] [PubMed]
- Kuwornu JP, Lix LM, Quail JM, et al. Identifying Distinct Healthcare Pathways During Episodes of Chronic Obstructive Pulmonary Disease Exacerbations. Medicine (Baltimore) 2016;95:e2888. [Crossref] [PubMed]
- Sneath E, Bunting D, Hazell W, et al. Pre-hospital and emergency department pathways of care for exacerbations of chronic obstructive pulmonary disease (COPD). J Thorac Dis 2019;11:S2221-9. [Crossref] [PubMed]
- Khialani B, Sivakumaran P, Keijzers G, et al. Emergency department management of acute exacerbations of chronic obstructive pulmonary disease and factors associated with hospitalization. J Res Med Sci 2014;19:297-303.
- Kelly AM, Holdgate A, Keijzers G, et al. Epidemiology, prehospital care and outcomes of patients arriving by ambulance with dyspnoea: an observational study. Scand J Trauma Resusc Emerg Med 2016;24:113. [Crossref] [PubMed]
- Australian Institute of Health and Welfare. Chronic Obstructive Pulmonary Disease (COPD), associated comorbidities and risk factors. Canberra: AIHW, 2020.
- Queensland Health. The Health of Queenslanders 2016. Report of the Chief Health Officer Queensland. Brisbane: Queensland State Government, 2016.
- Australian Institute of Health and Welfare. Emergency department care 2016-2017: Australian hospital statistics. Canberra: AIHW, 2017.
- Chow JW, Khullar K, Katechia K, et al. Controlled oxygen therapy at emergency department presentation increases the likelihood of achieving target oxygen saturations in patients with exacerbations of chronic obstructive pulmonary disease. Emerg Med Australas 2016;28:44-7. [Crossref] [PubMed]
- Kelly AM, Holdgate A, Keijzers G, et al. Epidemiology, treatment, disposition and outcome of patients with acute exacerbation of COPD presenting to emergency departments in Australia and South East Asia: An AANZDEM study. Respirology 2018;23:681-6. [Crossref] [PubMed]
- Tsai CL, Clark S, Cydulka RK, et al. Factors associated with hospital admission among emergency department patients with chronic obstructive pulmonary disease exacerbation. Acad Emerg Med 2007;14:6-14. [Crossref] [PubMed]
- Australian Institute of Health and Welfare. Asthma in Australia - with a focus chapter on chronic obstructive pulmonary disease, 2011. Canberra: AIHW, 2011.


