Efficiency of neural respiratory drive for the assessment of bronchodilator responsiveness in patients with chronic obstructive pulmonary disease: an exploratory study
Introduction
Worldwide, chronic obstructive pulmonary disease (COPD) is a major cause of chronic morbidity, mortality and disability, leading to heavy social and economic burdens (1). Dyspnoea is an important cause of exercise limitation and reduced quality of life for COPD patients (2). Notably, inhaled bronchodilators as the mainstay of pharmacologic treatment of COPD have been known to alleviate dyspnoea and improve exercise tolerance in these patients.
Proper evaluation of the response to bronchodilator therapy may assist in treatment decisions for COPD patients. Conventional lung function parameters, such as forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), inspiratory capacity (IC) and functional residual capacity (FRC) are generally used to evaluate the efficacy of inhaled bronchodilators. However, these indices lack sensitivity to some extent. For instance, FEV1, an important index to determine the severity of COPD, tends to underestimate the actual effect of drugs because expiratory flow limitation in COPD is not fully reversible (3-5). Furthermore, the magnitude of improvement in lung function has been within the range of measurement variability per se, which is particularly evident in patients with moderate-to-severe COPD, so it is difficult to distinguish between the curative changes and the variability. Consequently, the American Thoracic Society and the European Respiratory Society recommended a combination of pulmonary function improvement and patient-reported dyspnoea relief. Hence, patient-perceived symptomatic improvements following inhaled bronchodilators could be considered as part of clinical curative effect despite no significant changes in spirometry. Nevertheless, perception of breathlessness varies among individuals (6), and sometimes patient complaints may not align with therapeutic effects, which could lead to improper decision-making in medical treatment. Therefore, clinical studies of a novel objective indicator to help assess outcomes of bronchodilator therapy in COPD can be of interest.
Recent studies have demonstrated an increase in neural respiratory drive (NRD) in COPD patients (7-10), which is principally due to adverse pulmonary mechanics requiring an increased drive to maintain ventilation. However, the actual ventilation tends to descend. Efficiency of NRD, expressed by a ratio of ventilation to the diaphragm electromyogram (EMGdi), may reflect the unbalanced relationship between ventilation and NRD, and precisely evaluate the physiological changes in patients. Further, in COPD patients, this ratio decreased gradually during exercise and significantly improved after received tiotropium bromide 18 µg once daily for 1 month (11,12). Those authors concluded that the improved efficiency of NRD might underlie the improvement in exercise tolerance and the reduction of dyspnoea. In other words, improving the NRD efficiency may relieve clinical symptoms and make patients feel better. Thus, we hypothesized that the efficiency of NRD, defined in the present study as the ratio of minute ventilation (VE) to the root mean square (RMS) of EMGdi, or VE/RMS, might be a better tool than other lung function parameters to evaluate the treatment response in COPD.
Methods
Patient recruitment
This was a prospective, randomized, and placebo-controlled study, registered at ClinicalTrials.gov, identifier number NCT02296047. The local ethics committee approved the study and all participants provided informed consent. From November 2014 to June 2015, patients with moderate-to-severe COPD in Guangzhou Panyu Central Hospital and Zhujiang Hospital were consecutively enrolled in this study. Moderate-to-severe COPD was defined as FEV1/FVC <70% and 30% < FEV1%pred <80% after bronchodilation, according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) (1). Exclusion criteria were (I) an acute exacerbation during the previous 8 weeks; (II) history of oral corticosteroids within 4 weeks; (III) complications from other comorbidities, such as asthma, respiratory failure and neuromuscular diseases.
Study design
Administration of bronchodilators was prohibited 48 hours prior to the experiment. Shown in Figure 1, thirty-six subjects were randomized into two groups: group A (n=18) and group B (n=18). Every individual in group A inhaled 400 µg placebo, 400 µg salbutamol and 80 µg ipratropium in sequence while those in group B inhaled 400 µg placebo, 80 µg ipratropium, and 400 µg salbutamol in sequence. This grouping design was to investigate whether the sequence of medication made a difference. Lung function testing (including FEV1, FVC and IC), respiratory flow, EMGdi, and subjective dyspnoea score were measured at four time points, including baseline (identified as T0), 30 min after inhalation placebo (TP), 15 min after salbutamol or 30 min after ipratropium (T1), and after inhalation of two bronchodilators (T2). Lung function tests were performed with a spirometer (Jaeger, Germany). Flow was monitored by the differential pressure sensor (ML141, AD Instruments Corporation, Australia). During rested tidal breathing, values of VE were calculated after five consecutive respiratory cycles by integrating flow. Dyspnoea was assessed with the Borg score ranging from 0 to 10, where higher scores indicate greater intensity of breathlessness.

Medications in the study
The medications in this study included: placebo (nebulised saline solution, Glaxo Wellcome Pharmaceutical Co. Ltd., Chongqing, China), salbutamol (Ventolin, Glaxo Wellcome Products, France) and ipratropium bromide (Atrovent, Boehringer Ingelheim Pharmaceutical Co. Ltd., Germany). We chose the short-acting medications (salbutamol and ipratropium) because of the need for faster actions in our time design. In the present study, the differences between salbutamol and ipratropium were not compared. Instead, the effect of inhaled bronchodilators was compared with placebo and the effect of combined bronchodilators was compared with a single bronchodilator.
Oesophageal electrode positioning and measurement of EMGdi
As described previously (8,9,13), a five-pair oesophageal electrode catheter was used to record the EMGdi. The catheter was positioned according to the magnitude of EMGdi, and the optimal position was determined by the greatest amplitude of EMGdi in electrode pairs 1 and 5, and the lowest in electrode pair 3. The EMGdi signals were band-pass filtered between 10 Hz and 2 kHz and amplified using signal amplifier (3808; Yinghui Medical Technology Co., Ltd., Guangzhou, China). The raw signal was converted to RMS with LabChart7.5 software (Powerlab, AD Instruments Co., Australia) with the time constant of 100 ms. To avoid the influence of the electrocardiogram on EMGdi, RMS was measured from the segments between QRS complexes. The peak of RMS selected from five pairs of electrodes was measured on a breath-by-breath basis.
Data analysis
At each time point, FEV1, FVC, and IC were repeated at least three times while RMS and VE/RMS were calculated every 0.5 minutes during a 1.5-min stable eupnoea period. Consequently, FEV1, FVC, IC, RMS and VE/RMS for each subject had three values at each time point and these values were analysed. First, we calculated the variability of the five indices for each subject at each time point and the average variability for all subjects. Variability was computed in two ways: aberration rate [△% = (Max – Min)/mean × 100%] and the coefficient of variation (CV% = standard deviation/mean × 100%). Significant response to bronchodilators was judged when the variation after medication was greater than the intra-subject variability or inter-subject variability. In this study, the 95% upper limit (UL) and coefficient of repeatability (CR) (6) were, according to the variation defined as the criterion to assess the responsiveness to inhaled bronchodilators in COPD subjects, used for the above five indices and the Borg score.
Statistical analysis
Statistical calculations were carried out using Statistical Package for Social Sciences (SPSS 19.0, Chicago, IL, USA). Data were expressed as mean values ± standard deviation. Between-group differences in basic data were compared by using unpaired t-test. Analysis of variance of repeated measurement data was used to assess the quantitative differences among the different time points and least significant difference was used to detect inter-point differences. Rank correlation analysis was used to study correlations between the Borg score and other indices. A P value of <0.05 was considered statistically significant.
Results
Thirty-six patients (all males, aged 66.47±6.72 years) with FEV1 of 1.25±0.37 L (48.31%±12.15% predicted) were included in the study. Descriptive characteristics of the patients are summarized in Table 1.
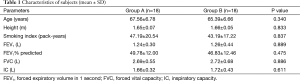
Full table
Effects of inhaled bronchodilators on the five indices and Borg score
Shown in Table 2, in comparison with placebo, inhaled bronchodilators improved FEV1, FVC, IC, and decreased RMS, thus VE/RMS increased (all P<0.05). However, in comparison with a single bronchodilator, combined bronchodilators did not show statistical improvement in the five indices (all P>0.05). Furthermore, no significant differences in the five indices were found between group A and group B (all P>0.05). When all subjects in two groups were considered, the percentage change of FEV1, FVC, IC, RMS, and VE/RMS after inhaled bronchodilators were 12.52%±6.78%, 15.02%±11.33%, 15.97%±11.36%, −27.41%±13.67%, 41.47%±31.22%, respectively. VE/RMS had the largest improvement among the five indices (Figure 2).

Full table
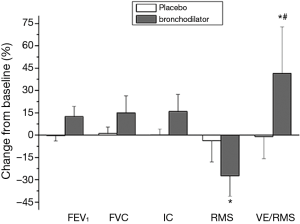
Inhaled bronchodilators resulted in a significant decrease in both Borg score and the corrected Borg scale with VE (Borg score/VE), while no differences were observed after placebo. Before and after inhaled bronchodilators, the Borg score was positively related to RMS (r=0.236, P=0.043) and negatively correlated with VE/RMS (r=−0.253, P=0.03), but not associated with FEV1, FVC, or IC (r=−0.116, P=0.326; r=−0.194, P=0.097; r=−0.205, P=0.080, respectively). The reduction of dyspnoea correlated was positively related to RMS (r=0.317, P=0.029) and negatively with the increase of VE/RMS (r=−0.507, P=0.002), but it was not associated with the changes of FEV1, FVC, or IC (r=−0.008, P=0.965; r=−0.162, P=0.360; r=−0.001, P=0.996, respectively).
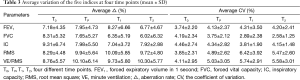
Average variability of the five indices
Shown in Table 3, the average aberration rate and CV of each index were not significantly different among four time points, indicating that individual variability was not influenced by time and medication. Then an average variability of each index at four time points was calculated as follows: the average aberration rate (%) were 7.41±5.19, 6.24±4.19, 7.65±4.48, 9.76±5.75, and 9.15±5.44 for FEV1, FVC, IC, RMS, and VE/RMS, respectively; the average CVs (%) were 3.89±2.66, 3.86±2.81, 4.35±2.87, 5.21±3.09, and 5.06±3.04 for the five indices, respectively. In other words, the average variability of RMS and VE/RMS were higher than that of FEV1, FVC, and IC (P<0.05), but there were no significant differences among FEV1, FVC, and IC and between RMS and VE/RMS (P>0.05).
Full table
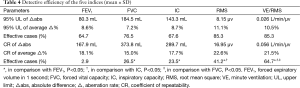
Detection efficiency of the five indices
According to intra-subject variation, the value above the UL of the 95% confidence interval of each index at T0 was defined as the criterion to judge the clinical therapeutic effect of the medication. The percentages of the values were 69.0%, 64.3%, 56.0%, 83.3%, and 79.4% for FEV1, FVC, IC, RMS, and VE/RMS, respectively. The detection efficiency of VE/RMS was higher than FVC, FEV1 and IC (P<0.05), whereas there was no significant difference between VE/RMS and RMS.
In contrast, according to inter-subject variation, the detection efficiency of the five indices was shown in Table 4. No significant difference in the percentage of values over 95% UL of average aberration rate was found between different indices. However, when the percentage of values above CR was calculated, the detection efficiency of VE/RMS was higher than FVC, FEV1 and IC (P<0.05).
Full table
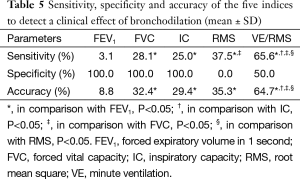
Based on the Borg score change, the value of CR over the absolute difference and average variability was defined as the criterion to judge the clinical therapeutic effect of the medication. Though the specificity of VE/RMS was lower than FEV1, FVC, and IC, VE/RMS had the highest sensitivity and accuracy among the five indices (Table 5).
Full table
Discussion
Proper assessment of bronchodilator responsiveness may assist in treatment decisions for COPD patients. Herein, we conducted an exploratory study in which we compared the detection efficiency of a novel indicator termed VE/RMS with FEV1, FVC, IC, and RMS. The principal finding is that VE/RMS may be a more sensitive and accurate indicator than traditional lung function parameters and NRD.
Traditionally, FEV1 and FVC are used to assess progression of disease and response to treatment. Although the standardization of spirometry has improved in recent years, a certain degree of variability in lung function parameters is unavoidable. The variability of FEV1 and FVC in normal subjects was reported to be less than 5%, whereas those in COPD patients were 17% and 15%, respectively. The fact that changes in lung function parameters overlap with the measurement variability makes it difficult to disambiguate whether the change is from the curative improvement of drugs or from the variation of measurements per se. Consequently, previous studies (14,15) recommended changes in FEV1 and FVC that exceed 95% confidence limits of short-term variability as a criterion to determine a statistically significant response to bronchodilators. In an evaluation of variability of spirometry in COPD, Herpel and colleagues (16) suggested that a change of 225 mL absolute difference in FEV1 and 325 mL in FVC could be used as a threshold to evaluate changes in lung function in COPD patients. Herein, we define that acute bronchodilator responsiveness occur when a value in FEV1 or FVC exceeds the limits defined by our study results. Additionally, other evaluating parameters such as IC and the forced inspiratory volume in one second (FIV1) (17) are also influenced by the degree of hyperinflation and airway obstruction, and may underestimate the effect of drugs.
Patients with COPD are characterized by dynamic hyperinflation and impaired diaphragm function, which is known to alter initial length of the diaphragm and reduce inspiratory pressure generation. Consequently, higher NRD would be expected to sustain ventilation in COPD patients than in healthy subjects, particularly during exercise. Since NRD is closely associated with disease severity and changes in the perception of dyspnea, it has served as a physiological biomarker for monitoring the changes during acute exacerbations of COPD (18). Previous studies have shown that inhaled bronchodilators can decrease central inspiratory drive and improve dyspnoea in COPD patients (19,20). As expected, the NRD of all patients in the present study decreased significantly after inhaled bronchodilators. Furthermore, our study showed a better correlation between the reduction of NRD and the alleviation of dyspnoea than that between lung function parameters and dyspnoea. After eliminating the effect of variation, RMS had higher detection efficiency than FVC, FEV1 and IC, indicating that NRD did better in detecting the response to bronchodilators.
Based on NRD, we chose VE/RMS to evaluate the efficacy of inhaled bronchodilators. As is known, the association between ventilation and NRD would be unbalanced in patients with COPD, especially during an acute exacerbation. For instance, the actual ventilation is unchanged or decreased despite the ventilation demand and NRD increase. Consequently, VE/RMS, as a composite index, may be preferable to NRD per se and reflect better the change of respiratory physiology in COPD patients. Bronchodilators can mitigate hyperinflation and gas trapping in COPD patients, leading to reduced airways resistance. This may alter the length-tension relations of the diaphragm, promote VE, attenuate EMGdi activity and therefore heighten the efficiency of NRD. Our results showed that improvement of VE/RMS was the greatest (41.47%±31.22%) among five indices, much greater than that of FVC (23%) or IC (22%) reported by O’Donnell et al. (21), suggesting this indicator had meaningful acute bronchodilator responsiveness. Furthermore, we found that the reduction of dyspnoea correlated negatively with the increase in VE/RMS. Though VE/RMS did not have a higher detection efficiency than RMS, it was more sensitive and accurate, based on the change of the Borg score. These findings confirmed the concept that the improved efficiency of NRD might underlie symptomatic improvement in COPD patients (12). Therefore, the clinical value of VE/RMS seems to be superior to both pulmonary function indices and NRD.
In the present study, EMGdi signals were recorded using a five-pair oesophageal electrode catheter, which has been acknowledged as an ideal method to quantify NRD since it is not easily disturbed by other respiratory muscles and not affected by electrode movement and lung volume change (8-13). However, oesophageal electrode placement is an invasive test and may hinder its clinical application. As such, from a clinical point of view, it is difficult to determine RMS and VE/RMS in the daily medical practice. Fortunately, due to technological advances in signal detection and processing, surface electromyography (EMG) provides a non-invasive way for rapid monitoring muscle activities, and gives results correlated with those obtained using oesophageal electrodes (22,23). Some researchers even claimed that NRD measurements could be used in COPD management as electrocardiography is used to evaluate and monitor ischemic heart disease (24). Thus, when non-invasive methods substitute for oesophageal electrodes, RMS and VE/RMS would be applicable.
We found that the sequence of medication did not significantly impact on the efficacy of inhaled bronchodilators. A combination of β-2 agonists and anti-muscarinic antagonists is recognized to be more advantageous than the individual agents in COPD patients (25,26). In this study, a combination of salbutamol and ipratropium did not show statistical improvement over either drug alone in all five indices, but showed superior efficacy in terms of absolute changes.
Our study has a few limitations. First, due to the restricted use of oesophageal electrode noted above, the number of enrolled participants was relatively small, so the results should be verified in a large clinical trial evaluating the efficacy of bronchodilators. Second, the symptoms and exercise limitation of COPD patients are exacerbated during exercise; further study is required to explore the clinical value of VE/RMS during exercise. Finally, the study design used a placebo followed by a crossover to active bronchodilator arms in a randomized order. However, providing the placebo in a non-random fashion may limit some of the conclusions drawn from the study.
In conclusion, the efficiency of NRD seems promising as a sensitive index to evaluate the response to inhaled bronchodilators. Certainly, the application of this indicator in evaluating treatment benefits warrants further investigation.
Acknowledgements
Funding: This work was supported by the Guangdong Provincial Science and Technology Project (A2013137 and 2013B022000072), the Guangzhou Municipal Science and Technology Project (201300000171 and 201507020033), and the Panyu District Science and Technology Project (2014S01049).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2013;187:347-65. [Crossref] [PubMed]
- Mahler DA, O'Donnell DE. Recent advances in dyspnea. Chest 2015;147:232-41. [Crossref] [PubMed]
- Belman MJ, Botnick WC, Shin JW. Inhaled bronchodilators reduce dynamic hyperinflation during exercise in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1996;153:967-75. [Crossref] [PubMed]
- O'Donnell DE, Lam M, Webb KA. Measurement of symptoms, lung hyperinflation, and endurance during exercise in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;158:1557-65. [Crossref] [PubMed]
- O'Donnell DE. Assessment of bronchodilator efficacy in symptomatic COPD: is spirometry useful? Chest 2000;117:42S-7S. [Crossref] [PubMed]
- Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J 2005;26:948-68. [Crossref] [PubMed]
- Parshall MB, Schwartzstein RM, Adams L, et al. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med 2012;185:435-52. [Crossref] [PubMed]
- Luo YM, Moxham J. Measurement of neural respiratory drive in patients with COPD. Respir Physiol Neurobiol 2005;146:165-74. [Crossref] [PubMed]
- Jolley CJ, Luo YM, Steier J, et al. Neural respiratory drive in healthy subjects and in COPD. Eur Respir J 2009;33:289-97. [Crossref] [PubMed]
- Jolley CJ, Luo YM, Steier J, et al. Neural respiratory drive and breathlessness in COPD. Eur Respir J 2015;45:355-64. [Crossref] [PubMed]
- Qin YY, Steier J, Jolley C, et al. Efficiency of neural drive during exercise in patients with COPD and healthy subjects. Chest 2010;138:1309-15. [Crossref] [PubMed]
- Qin YY, Li RF, Wu GF, et al. Effect of tiotropium on neural respiratory drive during exercise in severe COPD. Pulm Pharmacol Ther 2015;30:51-6. [Crossref] [PubMed]
- Luo YM, Li RF, Jolley C, et al. Neural respiratory drive in patients with COPD during exercise tests. Respiration 2011;81:294-301. [Crossref] [PubMed]
- Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med 1995;152:1107-36. [Crossref] [PubMed]
- Sourk RL, Nugent KM. Bronchodilator testing: confidence intervals derived from placebo inhalations. Am Rev Respir Dis 1983;128:153-7. [Crossref] [PubMed]
- Herpel LB, Kanner RE, Lee SM, et al. Variability of spirometry in chronic obstructive pulmonary disease: results from two clinical trials. Am J Respir Crit Care Med 2006;173:1106-13. [Crossref] [PubMed]
- Taube C, Lehnigk B, Paasch K, et al. Factor analysis of changes in dyspnea and lung function parameters after bronchodilation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2000;162:216-20. [Crossref] [PubMed]
- Murphy PB, Kumar A, Reilly C, et al. Neural respiratory drive as a physiological biomarker to monitor change during acute exacerbations of COPD. Thorax 2011;66:602-8. [Crossref] [PubMed]
- Pino-García JM, García-Río F, Gómez L, et al. Short-term effects of inhaled beta-adrenergic agonist on breathlessness and central inspiratory drive in patients with nonreversible COPD. Chest 1996;110:637-41. [Crossref] [PubMed]
- O'Donnell DE, Banzett RB, Carrieri-Kohlman V, et al. Pathophysiology of dyspnea in chronic obstructive pulmonary disease: a roundtable. Proc Am Thorac Soc 2007;4:145-68. [Crossref] [PubMed]
- O'Donnell DE, Forkert L, Webb KA. Evaluation of bronchodilator responses in patients with "irreversible" emphysema. Eur Respir J 2001;18:914-20. [Crossref] [PubMed]
- Reilly CC, Ward K, Jolley CJ, et al. Neural respiratory drive, pulmonary mechanics and breathlessness in patients with cystic fibrosis. Thorax 2011;66:240-6. [Crossref] [PubMed]
- Zhang Y. Noninvasive imaging of internal muscle activities from multi-channel surface EMG recordings. Conf Proc IEEE Eng Med Biol Soc 2013;2013:5430-2.
- Garland AJ, Doshi A, Turcanu V. Neural respiratory drive measurement for COPD assessment and monitoring. Pneumologia 2015;64:14-7. [PubMed]
- Ulrik CS. Clinical benefit of fixed-dose dual bronchodilation with glycopyrronium and indacaterol once daily in patients with chronic obstructive pulmonary disease: a systematic review. Int J Chron Obstruct Pulmon Dis 2014;9:331-8. [Crossref] [PubMed]
- Mahler DA, Kerwin E, Ayers T, et al. FLIGHT1 and FLIGHT2: Efficacy and Safety of QVA149 (Indacaterol/Glycopyrrolate) versus Its Monocomponents and Placebo in Patients with Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med 2015;192:1068-79. [Crossref] [PubMed]


