Systematic review and meta-analysis of the risk factors for postoperative delirium in patients with acute type A aortic dissection
Highlight box
Key findings
• In this study, the meta-analysis showed that postoperative hypoxemia, ventilator-assisted use time, renal insufficiency, ICU stay time, and APACHE II score were high-risk factors for postoperative delirium in patients with acute type A aortic dissection.
What is known and what is new?
• Previous studies on the risk factors of postoperative delirium have not reached a completely consistent conclusion, and there is a lack of evidence-based medical research.
• Our study aimed to explore the risk factors of postoperative delirium in patients with acute type A aortic dissection by systematic evaluation and meta-analysis.
What is the implication, and what should change now?
• This study analyzed the risk factors of postoperative delirium in patients with acute type A aortic dissection by meta-analysis, which require further clinical attention.
Introduction
Aortic dissection is characterized by an acute onset and rapid progression with a high mortality rate, while acute type A aortic dissection progresses even faster and has a poor prognosis (1-3). Surgery is the most effective treatment in clinical practice. Although the surgical procedure for aortic dissection has been considerably enhanced in recent years, there are still many potential complications, such as delirium (4-6). Postoperative delirium is a severe brain disorder characterized by inattention, disturbed thinking, and altered levels of consciousness (7,8). This is a complication that occurs frequently after cardiac surgery, especially after aortic dissection surgery, with an incidence rate of 32.5–52.0% (9) and a 3-month mortality rate of as high as 90% (10).
Studies have shown that postoperative delirium (POD) leads to prolonged mechanical ventilation, prolonged duration of intensive care unit (ICU) stay, an increased daily risk of long-term hospitalization by 20%, persistent delirium, hypoxemia, and so on (2,5,11-13). It has also been reported that postoperative mobility of patients with acute type A aortic is decreased and their quality of life declines (3,14-16). However, there are many risk factors for postoperative delirium and the conclusion is often affected by the sample size, so there is no completely consistent conclusion in the reported literature at present, even there are some contradictory situations. For example, two studies reported that Acute Physiology, Age, Chronic Health Evaluation (APACHE) II score was not an independent risk factor for postoperative delirium (8,11), but other studies confirmed that APACHE II score was a high-risk factor for postoperative delirium (3,13-15). This controversial conclusion has caused some confusion for the judgment of high-risk factors of postoperative delirium. Although there are some models for predicting delirium risk, the proportion of aortic dissection in these models is not high, so they are not applicable to predict the risk of delirium after acute type A aortic dissection. Considering the negative effect of delirium on patients, correct conclusion of risk factor analysis is of great significance for disease prevention and mortality reduction (17). Meta-analysis, as a kind of evidence-based medicine, can expand the sample size and improve the test efficiency by combining the previous articles to make the conclusion more accurate. Therefore, in this study, we aimed to explore the risk factors of acute type A aortic dissection by systematic review and meta-analysis. A combined effect size analysis was also performed to determine the risk factors for postoperative delirium in patients with acute type A aortic dissection. We present the following article in accordance with the MOOSE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-10/rc).
Methods
Search strategy
Chinese literature was retrieved from the China National Knowledge Infrastructure (CNKI), cqvip.com (VIP), and WanFang databases, and English literature was retrieved from the PubMed, Willey Library, Embase, and Web of Science databases. The Chinese and English keyword search terms included ‘acute type A’, ‘aortic dissection’, ‘AAD’, ‘POD’, ‘postoperative’, ‘delirium’, ‘risk factors’, and so on. The retrieval time was updated to November 1, 2022.
Inclusion criteria
(I) Type of study: study on influencing factors of postoperative delirium in patients with acute type A aortic dissection; (II) subjects: patients with acute type A aortic dissection diagnosed according to cardiovascular imaging technology, who developed delirium after surgery and survived during postoperative hospitalization; (III) outcomes: the data in the included literatures are complete and may have extractable or converted risk factors.
Exclusion criteria
(I) The patients enrolled in the study had severe visual or hearing impairments and could not communicate; (II) articles involving patients with a history of stroke and renal insufficiency preoperatively; (III) reviews, comments, news, and other literature without original data; (IV) studies with repeated publications or data duplication.
Data extraction and quality assessment
The literature search was independently carried out by 2 researchers, and the Chinese and English data were searched and screened according to the included search terms and inclusion/exclusion criteria. When disagreements were encountered, a third researcher was included to discuss and decide to extract data from the finally included references.
The extracted data mainly included the author, year, region, sample number of patients in the two groups, age, and the original data of the included outcome indicators. The literature quality evaluation was performed using the Newcastle-Ottawa Scale (NOS), and the evaluation criteria mainly included three parts: the selection of research objects, comparability between the groups, and outcome measurement (total NOS score: 9 points).
Sensitivity and publication bias analyses
The sensitivity analysis was evaluated using the odd risk (OR) value with the 95% confidence interval (CI) of the random effect model, and the stability of the OR and 95% CI were observed by sequentially eliminating the literature. If the result after elimination had little effect, the combined result was considered relatively stable. Egger’s and Begg’s tests were used to evaluate the publication bias, and P<0.05 was considered to indicate publication bias.
Statistical analysis
R 4.2.1 software (Lucent Technologies, USA) was used for meta-analysis, and the OR and 95% CI were converted into logOR and its Standard error (SE) of multivariate analysis for meta-analysis. The heterogeneity test was conducted using the I2 test. I2≤50% indicated that the heterogeneity among the studies was relatively small, and the fixed-effect model was used to analyze the results. However, I2>50% suggested that there was heterogeneity among the included studies, and the random-effects model was used for analysis.
Bilateral P<0.05 was considered to indicate statistical significance.
Results
Literature search results
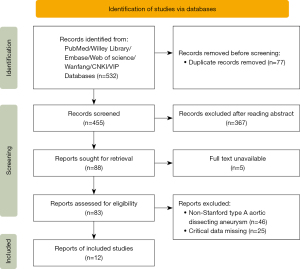
Through a preliminary search in the above-mentioned Chinese and English databases, 532 articles related to postoperative delirium after acute type A aortic dissection were obtained, including 210 articles in Chinese and 322 articles in English. After removing 77 duplicate articles, we read the titles, abstracts, and full texts of the remaining 455 articles. Finally, 12 studies were included (Figure 1).
Basic characteristics and quality assessment of the included literature
Basic characteristics of literature
The publication period of the included studies was between 2016 and 2022. The research institutes were all located in China. There were no statistical differences in the age and sex of the patients (Table 1).
Table 1
| Reference | Country | Type of study | Delirium group | Control group | Outcome measures | Literature quality | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Numbers | Age (years) | Sex ration (male/female) | BMI (kg/m2) | Numbers | Age (years) | Sex ration (male/female) | BMI (kg/m2) | ||||||
| Fang, 2016 (12) | China | Case-control study | 169 | 48.7±9.0 | 151/18 | – | 166 | 48.4±11.5 | 139/27 | – | 1, 2, 3 | B | |
| Zhou, 2016 (15) | China | Case-control study | 72 | 46.1±11.4 | 64/8 | 27.3±3.7 | 101 | 45.0±9.5 | 87/14 | 26.5±4.9 | 2, 3, 4, 5, 6, 7 | B | |
| Liu, 2017 (5) | China | Case-control study | 34 | 51.9±11.76 | 24/10 | – | 66 | 48.83±9.65 | 42/24 | – | 1, 3, 4, 5 | A | |
| Shi, 2019 (2) | China | Case-control study | 68 | 59.9±10.17 | 44/24 | 25.80±3.44 | 80 | 50.73±12.57 | 58/22 | 25.36±3.34 | 5, 6 | A | |
| Cai, 2020 (11) | China | Case-control study | 73 | 51.27±12.08 | 56/17 | – | 228 | 50.46±12.32 | 179/49 | – | 4, 7 | A | |
| Cheng, 2020 (3) | China | Case-control study | 30 | 45.87±3.45 | 20/10 | – | 50 | 44.89±4.03 | 35/15 | – | 1, 2, 4, 7 | B | |
| He, 2020 (18) | China | Case-control study | 92 | 52.56±6.34 | 71/21 | – | 208 | 50.77±5.28 | 146/62 | – | 2, 5 | B | |
| Zhu, 2020 (19) | China | Case-control study | 55 | 50.2±11.6 | 71/26 | – | 97 | 51.1±13.5 | 47/8 | – | 2, 3, 5 | B | |
| Lin, 2021 (13) | China | Case-control study | 103 | 53.3±10.5 | 81/41 | 25.4 | 154 | 51.1±12.8 | 113/41 | 24.0 | 1, 5, 6 | B | |
| Zhao, 2022 (14) | China | Case-control study | 148 | 56.4±5.2 | 118/30 | – | 262 | 55.5±6.6 | 204/58 | – | 1, 5, 6 | B | |
| Li, 2022 (6) | China | Case-control study | 51 | 55.39±10.47 | 46/5 | – | 194 | 48.04±12.57 | 148/46 | – | 3 | B | |
| Niu, 2022 (8) | China | Case-control study | 32 | 52. 4±9.1 | 22/10 | 23. 8±4. 2 | 78 | 45.2±11.4 | 56/26 | 24.9±3.6 | 3, 5, 7 | B | |
Outcome indicators: 1, hypoxemia; 2, duration of ventilator assistance; 3, renal insufficiency; 4, hemoglobin; 5, duration of stay in the ICU; 6, duration of hospitalization; 7, Acute Physiology and Chronic Health Evaluation II (APACHE II). BMI, body mass index; ICU, intensive care unit.
Literature quality evaluation
All the included literatures were case-control studies. NOS was used for quality evaluation. The results showed that there were 4 literatures with scores of 4–6, with medium risk of bias, and 8 literatures with scores of 7–9, with low risk of bias (Table 2). The quality of literatures met the requirements.
Table 2
| Reference | Case selection | Comparability | Exposure factors | Scoring | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | A | B | C | |||
| Fang, 2016, (12) | * | * | * | ** | * | * | 7 | ||
| Zhou, 2016, (15) | * | * | * | * | * | * | 6 | ||
| Liu, 2017, (5) | * | * | * | * | ** | * | * | * | 9 |
| Shi, 2019, (2) | * | * | * | * | ** | * | * | 8 | |
| Cai, 2020, (11) | * | * | * | * | ** | * | * | * | 9 |
| Cheng, 2020, (3) | * | * | * | ** | * | * | 7 | ||
| He, 2020, (18) | * | * | * | * | * | * | * | 7 | |
| Zhu, 2020, (19) | * | * | ** | * | * | 6 | |||
| Lin, 2021, (13) | * | * | * | ** | * | * | 7 | ||
| Zhao, 2022, (14) | * | * | * | * | * | 5 | |||
| Li, 2022, (6) | * | * | * | ** | * | * | 7 | ||
| Niu, 2022, (8) | * | * | * | * | * | * | 6 | ||
NOS, Newcastle-Ottawa Scale.
The relationship between postoperative hypoxemia and delirium
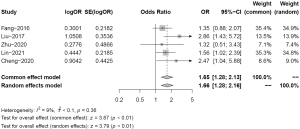
Five studies compared the blood oxygen levels of patients with acute type A aortic dissection with and without postoperative delirium. There was low heterogeneity (I2=9%) among the included studies. Fixed effects model analysis was used. Compared with the non-delirium group, patients in the delirium group had a higher probability of hypoxemia (OR =1.65, 95% CI: 1.28–2.13, P<0.01), indicating that postoperative hypoxemia was a high-risk factor for delirium (Figure 2).
The relationship between the duration of postoperative ventilator assistance and delirium
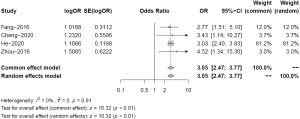
Four studies compared the duration of postoperative ventilator assistance in patients with acute type A aortic dissection with and without postoperative delirium. There was no heterogeneity (I2=0%) among the included studies. Fixed effects model analysis was used. Compared with the non-delirium group, patients in the delirium group had a longer postoperative ventilator assistance time (OR =3.05, 95% CI: 2.47–3.77, P<0.01), indicating that the duration of postoperative ventilator assistance was a high-risk factor for delirium (Figure 3).
The relationship between postoperative renal insufficiency and delirium
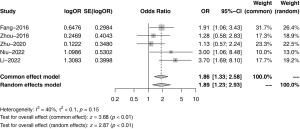
Five studies compared postoperative renal insufficiency between the two groups, and there was low heterogeneity (I2=40%) among the included studies. Fixed effects model analysis was used. Compared with the control group, patients in the delirium group had a higher incidence of postoperative renal insufficiency (OR =1.86, 95% CI: 1.33–2.58, P<0.01), indicating that postoperative renal insufficiency was a high-risk factor for delirium (Figure 4).
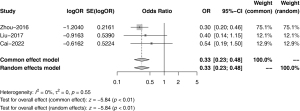
The relationship between postoperative hemoglobin level and delirium
Three studies compared the postoperative hemoglobin levels between the two groups, and the included studies were homogeneous (I2=0%), so the fixed effect model was used for analysis. Compared with the control group, patients in the delirium group had lower hemoglobin levels (OR =0.33, 95% CI: 0.23–0.48) but the difference was statistically significant (P<0.01). Thus, postoperative hemoglobin decrease was not a high-risk factor for delirium (Figure 5).
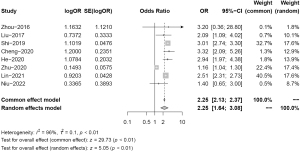
The relationship between postoperative duration in the ICU and delirium
Eight studies compared postoperative duration in the ICU between patients with acute type A aortic dissection with and without postoperative delirium. There was a high degree of heterogeneity among the included studies (I2=96%). An analysis of the source of heterogeneity showed that it may be caused by differences in the level of each medical institution. The results showed that compared with the control group, patients in the delirium group had a longer postoperative ICU stay (OR =2.25, 95% CI: 2.13–2.37, P<0.01), as shown in Figure 6. Therefore, the duration of postoperative ICU stay is a high-risk factor for delirium.
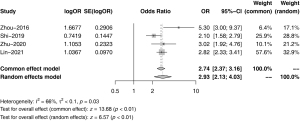
The relationship between postoperative duration of hospitalization and delirium
Four studies compared the difference in postoperative duration of hospitalization between the two groups, and there was a moderate degree of heterogeneity among the included studies (I2=66%). Compared with the control group, the total duration of hospital stay in the delirium group was longer (OR =2.74, 95% CI: 2.37–3.16) but the difference was not statistically significant (P<0.01, see Figure 7). Thus, the total duration of postoperative hospital stay was not a high-risk factor for delirium.
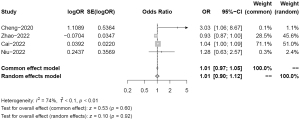
The relationship between postoperative APACHE II score and delirium
Four studies compared the differences in Acute Physiology and Chronic Health Evaluation II (APACHE II) scores between the two groups of patients. There was a moderate degree of heterogeneity among the included studies (I2=74%). The APACHE II score in the delirium group was significantly higher (OR =1.01, 95% CI: 0.90–1.12, P=0.92) than that in the control group, as shown in Figure 8, which indicated that the postoperative APACHE II score was not a high-risk factor for delirium.
Sensitivity analysis and evaluation of publication bias
The included literature had good stability. Except for the risk factors of postoperative renal insufficiency, the result of Egger’s and Begg’s tests showed P<0.05, indicating that there was no publication bias among the included literature (Table 3).
Table 3
| Risk factors | OR (95% CI) | Stability | Begg’s test | Egger’s test |
|---|---|---|---|---|
| Hypoxemia | 1.66 (1.28–2.16) | Stable | 0.62 | 0.36 |
| Duration of ventilator assistance | 3.05 (2.47–3.77) | Stable | 0.17 | 0.44 |
| Renal insufficiency | 1.89 (1.23–2.93) | Stable | 0.62 | 0.54 |
| Hemoglobin | 0.33 (0.23–0.48) | Stable | 0.60 | 0.26 |
| Duration of ICU stay | 2.25 (1.64–3.08) | Stable | 0.22 | 0.91 |
| Duration of hospital stay | 2.93 (2.13–4.03) | Stable | 0.50 | 0.51 |
| APACHE II score | 1.01 (0.90–1.12) | Stable | 1.00 | 0.63 |
OR, odds risk; CI, confidence interval; ICU, intensive care unit; APACHE II, Acute Physiology and Chronic Health Evaluation II.
Discussion
Acute type A aortic dissection is a critical illness characterized by disseminated intravascular coagulation that can accumulate in multiple viscera (6,20,21). Although the level of surgical treatment has been improved in recent years and the mortality rate has been reduced, postoperative complications are still an important factor leading to the death of patients (9,22). As a common complication after cardiac surgery, postoperative delirium has a high incidence rate. In acute type A aortic dissection, both the operative time and extracorporeal circulation time are longer, making it more likely that insufficient brain tissue irrigation will lead to postoperative delirium (8). Hypoxemia and long-term postoperative ventilator assistance are independent risk factors that have been reported in numerous studies (6,18). This may be because patients are more severely ill and have undergone complex surgical procedures. In our study, it was also found that patients in the delirium group had a higher probability of hypoxemia and a longer duration of ventilator-assisted ventilation (P<0.01). A study has reported that postoperative hemoglobin level reduction in patients was a high-risk factor for postoperative delirium (2), which is consistent with the conclusion of our paper. There is also a certain correlation between delirium and ICU stay time, as the ICU often involves limb restraint, indwelling catheter, sleep deprivation, etc., and delirium is prone to occur (2). Therefore, prolonged ICU stay may be an independent risk factor for delirium, which is consistent with the results of prolonged ICU stay in the delirium group. However, the total duration of hospital stay in the delirium group did not appear to be prolonged (12), which may be because there are other factors influencing the total length of hospital stay. Postoperative renal insufficiency is another common occurrence in patients with delirium, which is closely related to the prolongation of extracorporeal circulation, hypoxemia, and other poor irrigation factors (12). Thus, postoperative renal insufficiency is also a high-risk factor for postoperative delirium.
There were some limitations in this study that should be noted and considered. Firstly, due to the differences in the experience levels of various hospitals, there was relatively large heterogeneity among the outcome indicators in some articles, such as the number of days spent in the ICU. Secondly, the studies included in this paper were case-control studies and there was a lack of random clinical trials. Also, the considerable difference in sample size between the delirium and non-delirium groups in most studies may have some adverse effects on the results. Furthermore, all of the research was conducted in China. Although the sources of heterogeneity were minor, there is only a single source of evidence in this paper, and thus, new studies need to be included for further analysis.
Conclusions
In summary, low oxygen levels, prolonged mechanical ventilation, renal dysfunction, low hemoglobin, and prolonged ICU stay are all risk factors for postoperative delirium in patients with acute type A aortic dissection, clinical intervention measures can be taken according to the risk factors to prevent the occurrence of postoperative delirium. However, considering the shortcomings of this paper, more high-quality literature should be included in the future for further verification of the product.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MOOSE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-10/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-10/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gaul C, Dietrich W, Friedrich I, et al. Neurological symptoms in type A aortic dissections. Stroke 2007;38:292-7. [Crossref] [PubMed]
- Shi Q, Mu X, Zhang C, et al. Risk Factors for Postoperative Delirium in Type A Aortic Dissection Patients: A Retrospective Study. Med Sci Monit 2019;25:3692-9. [Crossref] [PubMed]
- Cheng LM. Risk factors and prevention of delirium after aortic dissection. International Journal of Nursing 2020;39:1862-864.
- Rubino AS, Onorati F, Caroleo S, et al. Impact of clonidine administration on delirium and related respiratory weaning after surgical correction of acute type-A aortic dissection: results of a pilot study. Interact Cardiovasc Thorac Surg 2010;10:58-62. [Crossref] [PubMed]
- Liu Z, Pang X, Zhang X, et al. Incidence and Risk Factors of Delirium in Patients After Type-A Aortic Dissection Surgery. J Cardiothorac Vasc Anesth 2017;31:1996-9. [Crossref] [PubMed]
- Li XP, Wang L, Zhang H, et al. Construction and evaluation of a risk prediction model of postoperative delirium in patients with Stanford type A aortic dissection. Chinese Journal of Nursing 2022;57:950-7.
- Abelha FJ, Luís C, Veiga D, et al. Outcome and quality of life in patients with postoperative delirium during an ICU stay following major surgery. Crit Care 2013;17:R257. [Crossref] [PubMed]
- Niu YS, Li L, Wei HY, et al. Risk factors of postoperative delirium in patients with acute type A aortic dissection. Journal of Clinical Anesthesiology 2022;38:622-6.
- Liu J, Yang F, Luo S, et al. Incidence, Predictors and Outcomes of Delirium in Complicated Type B Aortic Dissection Patients After Thoracic Endovascular Aortic Repair. Clin Interv Aging 2021;16:1581-9. [Crossref] [PubMed]
- Zhang WY, Wu WL, Gu JJ, et al. Risk factors for postoperative delirium in patients after coronary artery bypass grafting: A prospective cohort study. J Crit Care 2015;30:606-12. [Crossref] [PubMed]
- Cai S, Zhang X, Pan W, et al. Prevalence, Predictors, and Early Outcomes of Post-operative Delirium in Patients With Type A Aortic Dissection During Intensive Care Unit Stay. Front Med (Lausanne) 2020;7:572581. [Crossref] [PubMed]
- Fang MX, Xiong WP, Zeng R, et al. Research on the Risk Factors for Delirium of Stanford Type A Aortic Dissection Patients after Surgery. Chinese Journal of Thoracic and Cardiovascular Surgery 2016;23:357-61.
- Lin YJ, Lin LY, Peng YC, et al. Association between glucose variability and postoperative delirium in acute aortic dissection patients: an observational study. J Cardiothorac Surg 2021;16:82. [Crossref] [PubMed]
- Zhao YY, Shi XX, Lv L, et al. Study on related factors of postoperative delirium in patients with aortic dissection. Journal of Hubei University of Medicine 2022;41:392-7.
- Zhou CZ, Yang JA, Wen JM, et al. Analysis of risk factors for postoperative delirium in patients with acute type A aortic dissection. Chinese Journal of Arteriosclerosis 2016;24:1253-7.
- Gosselt AN, Slooter AJ, Boere PR, et al. Risk factors for delirium after on-pump cardiac surgery: a systematic review. Crit Care 2015;19:346. [Crossref] [PubMed]
- Kim WK, Song SW, Yoo KJ. The presence of left ventricular hypertrophy in patients with acute type A aortic dissection: weight on the postoperative clinical outcomes. J Thorac Dis 2022;14:4212-4. [Crossref] [PubMed]
- He Q, Xue C, Li BY, et al. Analysis of delirium characteristics and risk factors after hybridization in patients with Stanford type A aortic dissection. Shaanxi Medical Journal 2020;49:1432-5.
- Zhu YQ, Yang J, Sun X, et al. Analysis of risk factors for delirium after acute Stanford type A dissection. The Journal of Practical Medicine 2020;36:940-3.
- Wang Z, Ge P, Lu L, et al. Surgical outcomes of acute type A aortic dissection in dialysis patients: lessons learned from a single-center's experience. Sci Rep 2022;12:5372. [Crossref] [PubMed]
- He J, Ling Q, Chen Y. Construction and Application of a Model for Predicting the Risk of Delirium in Postoperative Patients With Type a Aortic Dissection. Front Surg 2021;8:772675. [Crossref] [PubMed]
- Hirakawa K, Nakayama A, Saitoh M, Hori K, Shimokawa T, Iwakura T, Haraguchi G, Isobe M. Factors Related to Hospitalisation-Associated Disability in Patients after Surgery for Acute Type A Aortic Dissection: A Retrospective Study. Int J Environ Res Public Health 2022;19:12918. [Crossref] [PubMed]
(English Language Editor: A. Kassem)