
Clinicopathological features and surgical outcomes of lobectomy combined with segmentectomy: a cohort study
Highlight box
Key findings
• Lobectomy + segmentectomy was performed for resection of multiple lobe lesions, a lesion invading two lobes, or a lesion with a lymph node invading the bronchial bifurcation. The incidence of major complications was similar to lobectomy + wedge resection, and there was no difference in mortality.
What is known and what is new?
• Although there is considerable data on routine segmentectomies, data on lobectomy + segmentectomy are scarce. Lobectomy + segmentectomy was associated with a higher rate of thoracotomy, longer operation time, and higher incidence of overall complications compared to lobectomy + wedge resection. However, there were no significant differences in major complications and mortality. Also, a greater variety of procedures was performed on the right lung, mostly combining a right upper or middle lobectomy with atypical segmentectomies.
What is the implication, and what should change now?
• Lobectomy + segmentectomy is a lung-preserving procedure that can benefit carefully selected patients with multiple or advanced diseases involving two lobes.
Introduction
Traditionally, a pneumonectomy, a bilobectomy, or a lobectomy combined with wedge resection is selected for multiple lesions of different lobes or a lesion invading two lobes. However, the popularization of segmentectomy has facilitated diverse surgical options for the resection of multiple lobe lesions, such as simultaneous multiple segmentectomies or lobectomy combined with segmentectomy (lobectomy + segmentectomy) (1,2). The feasibility of segmentectomy as a sublobar resection has been reported not only for lung cancer but also for the resection of metastatic lung cancers (3,4). To date, data on lobectomy + segmentectomy are scarce (5). Thus, we aimed to define the clinicopathological features and surgical outcomes of lobectomy + segmentectomy. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-696/rc).
Methods
Ethical statement
This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Institutional Review Board of Gunma University Hospital (protocol No. HS2019-279, approval on August 13th, 2021). Due to the retrospective nature of our study, patient consent was waived.
Study population and variables
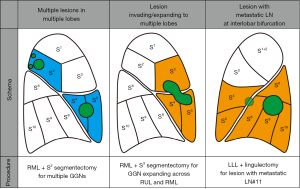
We retrospectively analyzed patients who underwent lobectomy between January 2010 and July 2021 at Gunma University Hospital, Japan. Lobectomy combined with segmentectomy (lobectomy + segmentectomy) was defined as the simultaneous performance of lobectomy and segmentectomy of the ipsilateral side. Lobectomy + segmentectomy was performed for (I) resection of multiple lobe lesions, (II) resection of a lesion invading two lobes, and/or (III) resection of a lesion with a lymph node invading the bronchial bifurcation (Figure 1). In order to assess the features of lobectomy + segmentectomy, we selected patients who underwent lobectomy combined with wedge resection (lobectomy + wedge resection) as control group. The sample size was taken as the number of lobectomies performed at our institute during the study period. We included all consecutive cases in an effort to decrease bias. We collected clinicopathological data by reviewing the patients’ charts. Surgical outcomes included the approach, operation time, blood loss, length of drainage, length of postoperative hospital stay, complications, and mortality. Complications were graded using the Clavien-Dindo classification (6,7). Lung cancer was classified according to the World Health Organization classification scheme (8).
Planning of surgical procedures
The surgical procedure (lobectomy, segmentectomy, and wedge resection) was planned preoperatively by the thoracic surgery team, according to the size and location of the lesions. Briefly, in cases of multiple lesions located in different lobes, lobectomy was performed for the lobe containing the largest invasive lesion. Selection between additional segmentectomy or wedge resection was decided preoperatively according to CT images, in order to obtain sufficient surgical margin. If a lesion extended to more than one lobe, lobectomy was performed for the lobe where the main lesion was situated, with the addition of segmentectomy or wedge resection. The extent of additional segmentectomy was planned so as to preserve as much lung parenchyma as possible while also achieving a sufficient surgical margin. Lobectomy + segmentectomy was also selected when a metastatic lymph node was invading the bronchial bifurcation of two lobes (i.e., lymph node #11 invading both the left upper and lower bronchus).
Statistical analysis
The resultant data were summarized as medians with interquartile ranges or as numbers with percentages. Chi-square test was used for categorical variables, and one-way analysis of variance, Kruskal-Wallis test, and Mann-Whitney test were used for continuous variables. P values were two-sided, with significance set at <0.05. Statistical analysis was performed using SPSS version 24 software (IBM Corp., Armonk, NY, USA).
Results
Patient and tumor characteristics
A total of 1,237 lobectomy cases were performed at Gunma University Hospital during the study period (Figure 2). There were 72 cases of lobectomy + wedge resection and 22 cases of lobectomy + segmentectomy. There were no significant differences in age, sex, comorbidities, pulmonary function, smoking status, laterality, and number of tumors (single vs. multiple) between both groups (Tables 1,2). However, there were differences in the pathological diagnosis of the resected tumors. Although the ratio of lung cancer was similar between the two groups (approximately 80%), patients with metastatic lung tumors were only present in the lobectomy + wedge resection group. When focused on lung cancer, the lobectomy + segmentectomy group included cases of more advanced disease than the lobectomy + wedge resection group, with more lymph node metastasis (50% vs. 26%, respectively) and advanced-stage disease (33% vs. 16%, respectively).
Table 1
| Characteristics | Lobectomy + wedge resection (n=72) | Lobectomy + segmentectomy (n=22) | P value |
|---|---|---|---|
| Age (year), median [IQR] | 69 [64–74] | 70 [64–77] | 0.531 |
| Sex, n (%) | 0.603 | ||
| Women | 34 (47%) | 9 (41%) | |
| Men | 38 (53%) | 13 (59%) | |
| Comorbidities, n (%) | |||
| COPD | 9 (13%) | 3 (14%) | 0.569 |
| Interstitial pneumonia | 3 (4%) | 1 (5%) | 0.663 |
| Diabetes mellitus | 13 (18%) | 2 (9%) | 0.259 |
| Cardiac disorder | 1 (1%) | 1 (5%) | 0.415 |
| Renal dysfunction | 3 (4%) | 0 (0%) | 0.445 |
| Pulmonary function, median [IQR] | |||
| FEV1 (L) | 2.1 [1.9–2.9] | 2.4 [1.8–2.8] | 0.846 |
| FEV1% (%) | 73.8 [68.8–79.5] | 77.0 [72.0–79.2] | 0.399 |
| Smoking, n (%) | 0.684 | ||
| Yes | 46 (64%) | 13 (59%) | |
| No | 26 (36%) | 9 (41%) | |
| Brinkman index, median [IQR] | 840 [421–1,145] | 733 [469–1,440] | 0.902 |
COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in one second; FEV1%, percent predicted FEV1; IQR, interquartile range.
Table 2
| Characteristics | Lobectomy + wedge resection (n=72) | Lobectomy + segmentectomy (n=22) | P value |
|---|---|---|---|
| Laterality, n (%) | 0.727 | ||
| Right | 55 (76%) | 16 (73%) | |
| Left | 17 (24%) | 6 (27%) | |
| Number of tumors, n (%) | 0.934 | ||
| Single | 32 (44%) | 10 (45%) | |
| Multiple | 40 (56%) | 12 (55%) | |
| Pathological diagnosis, n (%) | 0.018* | ||
| Lung cancer | 61 (85%) | 17 (77%) | |
| Metastatic lung tumor | 7 (10%) | 0 (0%) | |
| Non-malignant | 0 (0%) | 2 (9%) | |
| Others | 1 (1%) | 2 (9%) | |
| Combination | 3 (4%) | 1 (5%) | |
| Preoperative tumor diameter of largest lesion (mm), median [IQR] | 2.5 [1.7–3.4] | 3.0 [2.2–4.0] | 0.312 |
*, P<0.05. IQR, interquartile range.
Surgical features of lobectomy + segmentectomy
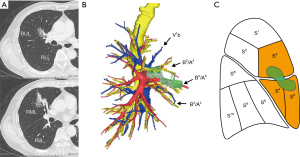
Approximately half of the lobectomy + segmentectomy cases were performed to resect a single lesion (Figure 3, orange), and the remainder were performed to resect two or more lesions (Figure 3, blue; range, 2–5 lesions). The most frequent type of lobectomy + segmentectomy was a combination of left lower lobectomy + lingulectomy (6 out of 22 cases, 27%), and all were performed by thoracotomy, with a high incidence of sleeve resection (5 out of 6, 83%). Furthermore, on the left side, the only type of lobectomy + segmentectomy performed was left lower lobectomy + lingulectomy, whereas on the right side, 10 different types of procedures were performed, many of which were approached thoracoscopically (7 out of 16 cases, 44%) and mainly for multiple lesions (10 out of 16 cases, 63%) (Table 3). The number of resected lesions was also higher on the right side than on the left (median: 2 vs. 1, respectively), whereas the amount of lung parenchyma resected on the right side was smaller (median: 4 vs. 6 segments, respectively). A representative case of lobectomy + segmentectomy is shown in Figure 4 and Video 1 (right middle lobectomy + S3 segmentectomy).
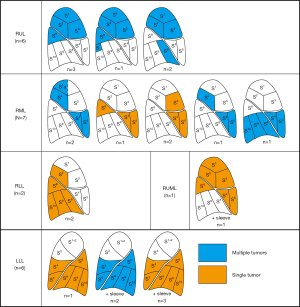
Table 3
| Lobectomy | Segmentectomy | Additional resection | Approach | Number of resected segments | Number of resected lesions |
|---|---|---|---|---|---|
| RUL (n=6) | S6 | None | Thoracotomy | 4 | 2 |
| S6 | None | Thoracotomy | 4 | 2 | |
| S6+S* | None | VATS | 5 | 2 | |
| S6 | S8 wedge | VATS | 4 | 5 | |
| S8 | None | Thoracotomy | 4 | 2 | |
| S8 | None | VATS | 4 | 2 | |
| RML (n=7) | S1a+S2 | None | VATS | 3.5 | 2 |
| S1a+S2 | None | VATS | 3.5 | 2 | |
| S2 | None | Thoracotomy | 3 | 4 | |
| S3 | None | Thoracotomy | 3 | 1 | |
| S3 | None | Thoracotomy | 3 | 1 | |
| S6 | None | Thoracotomy | 3 | 1 | |
| Basal | None | Thoracotomy | 6 | 3 | |
| RLL (n=2) | S2 | None | VATS | 6 | 1 |
| S2 | None | VATS | 6 | 1 | |
| RUML (n=1) | S6 | Sleeve resection | Thoracotomy | 6 | 1 |
| LLL (n=6) | Lingula | None | Thoracotomy | 6 | 1 |
| Sleeve resection | Thoracotomy | 6 | 1 | ||
| Sleeve resection | Thoracotomy | 6 | 1 | ||
| Sleeve resection | Thoracotomy | 6 | 1 | ||
| Sleeve resection | Thoracotomy | 6 | 2 | ||
| Sleeve resection | Thoracotomy | 6 | 2 | ||
| Median [IQR] | 4.5 [3.6–6.0] | 2 [1–2] |
RUL, right upper lobe; RML, right middle lobe; RLL, right lower lobe; RUML, right upper and middle lobe; LLL, left lower lobe; S*, subsuperior segment; VATS, video-assisted thoracic surgery; IQR, interquartile range.
Surgical outcomes and complications
When compared with the lobectomy + wedge resection group, patients in the lobectomy + segmentectomy group had a higher ratio of thoracotomy (59% vs. 24%) and a longer operation time (median: 273 vs. 201 min). Although not significant, the amount of blood loss was higher, and the length of drainage and postoperative hospital stay were longer in the lobectomy + segmentectomy group (Table 4). Postoperative complications are summarized in Tables 4 and 5. The overall incidence of complications was higher in the lobectomy + segmentectomy group than in the lobectomy + wedge resection group (50% vs. 31%, respectively). However, there were no significant differences in terms of major complications (higher than Clavien-Dindo grade IIIa) and mortality between the two groups. We experienced one case of bronchopleural fistula in each group: one after a right upper + middle lobectomy + S6 segmentectomy and another after a left lower lobectomy + left upper lobe wedge resection. The only 90-day mortality case was in the lobectomy + wedge resection group, which was due to the rapid progression of the lung cancer, with multiple metastases to the brain, lymph nodes, and digestive tract.
Table 4
| Characteristics | Lobectomy + wedge resection (n=72) | Lobectomy + segmentectomy (n=22) | P value |
|---|---|---|---|
| Approach, n (%) | 0.002* | ||
| VATS | 55 (76%) | 9 (41%) | |
| Thoracotomy | 17 (24%) | 13 (59%) | |
| Surgical outcomes, median [IQR] | |||
| Operation time (min) | 201 [163–239] | 273 [230–306] | <0.001* |
| Blood loss (mL) | 30 [5–130] | 95 [19–167] | 0.880 |
| Postoperative outcomes | |||
| Length of drainage (days), median [IQR] | 3 [2–4] | 4 [2–8] | 0.286 |
| Length of stay (days), median [IQR] | 7 [6–10] | 9 [7–12] | 0.180 |
| Mortality (30-day), n (%) | 0 (0%) | 0 (0%) | NA |
| Mortality (90-day), n (%) | 1 (1.4%) | 0 (0%) | 0.766 |
| Complications, n (%) | |||
| Overall | 22 (31%) | 11 (50%) | 0.094 |
| Major (> grade IIIa) | 5 (7%) | 2 (9%) | 0.520 |
*, P<0.05. IQR, interquartile range; NA, not assessed; VATS, video-assisted thoracic surgery.
Table 5
| Characteristics | Lobectomy + wedge resection (n=72) | Lobectomy + segmentectomy (n=22) | P value |
|---|---|---|---|
| Pulmonary complications, n (%) | |||
| Bronchopleural fistula | 1 (1%) | 1 (5%) | 0.415 |
| Pulmonary fistula (last >7 days or requiring adhesion therapy) | 13 (18%) | 5 (23%) | 0.417 |
| Late-onset pulmonary fistula | 1 (1%) | 0 (0%) | 0.766 |
| Pneumonia | 1 (1%) | 2 (9%) | 0.136 |
| Chylothorax | 0 (0%) | 0 (0%) | NA |
| Empyema | 0 (0%) | 1 (5%) | 0.234 |
| Other types of complications, n (%) | |||
| Brain infarction | 0 (0%) | 0 (0%) | NA |
NA, not assessed.
Discussion
We analyzed the clinicopathological features and surgical outcomes of patients who underwent lobectomy + segmentectomy. As reference, we compared clinicopathological and surgical data to those who underwent lobectomy + wedge resection. Our analysis revealed several key findings. First, lobectomy + segmentectomy was a rare procedure compared with lobectomy + wedge resection (2% vs. 6% of all lobectomy cases, respectively). Second, lobectomy + segmentectomy was often performed by thoracotomy and required a longer operation time and had higher ratio of overall complications. However, the incidence of major complications was similar to lobectomy + wedge resection (7% for lobectomy + segmentectomy vs. 9% for lobectomy + segmentectomy), and there was no difference in 90-day mortality. Third, a greater variety of lobectomy + segmentectomy procedures was performed on the right lung compared with the left lung.
The patient and tumor characteristics in our study cohort were similar between the lobectomy + wedge resection and the lobectomy + segmentectomy groups. The lobectomy + segmentectomy group required a significantly longer operation time. This is expected because a combined segmentectomy is more complex than a wedge resection and the ratio of sleeve resection was also higher. The operation time in our lobectomy + segmentectomy group was similar to previously reported bronchoplastic and sleeve resections, reporting an average of 248 minutes (9). The incidence of overall complications was also higher for the lobectomy + segmentectomy group in our study. That coincides with previous reports, since complex lung procedures are a risk factor for surgical complications (10). A benefit of lobectomy + segmentectomy is that segmentectomy allows better assessment and dissection of lymph nodes related to the segmentectomy, when compared to a lobectomy + wedge resection. Amongst the 22 cases of lobectomy + segmentectomy in our study, there were three cases of postoperative upstaging related to positive lymph nodes.
Interestingly, the types of lobectomy+ segmentectomy were fairly diverse on the right side, mostly combining a right upper lobectomy or middle lobectomy with atypical segmentectomies (i.e., S1a, S2, S3, or S8). The right lung has more lobes and segments than the left lung, which allows for more diverse options. In contrast, the only lobectomy + segmentectomy performed on the left side was lower lobectomy + lingulectomy, often requiring bronchial sleeve resection. Left lower lobectomy + lingulectomy with sleeve resection is a subtype of extended sleeve resection, known as type C (11-16). Amongst other studies focusing on extended sleeve resections, type C was one of the most commonly performed extended sleeve resection (14,16,17). Our study includes a type A extended sleeve resection on the right side (i.e., right upper + middle lobectomy + S6 segmentectomy). Another putative type of left-sided lobectomy + segmentectomy is left upper lobectomy + S6 segmentectomy (type B extended sleeve), but this procedure was not performed in our institute during the study period. This might be because our rationale when performing an extended sleeve resection is to perform a resection that preserves as much lung parenchyma as possible while still securing sufficient surgical margins. Therefore, in a clinical case requiring a left upper lobectomy + S6, we might have selected a left upper division + S6 segmentectomy.
This study has several limitations. Firstly, this was a retrospective analysis with a small sample size and possible selection bias for selection of procedures. In this study, we used the lobectomy + wedge resection group as reference to highlight the features of lobectomy + segmentectomy. However, background difference in tumor location and size was a bias that prevented comparison of the two procedures on equal terms. Most importantly, we believe that procedures were not interchangeable. For example, we would not perform segmentectomy for a lesion that could be resected by wedge resection. Similarly, the lobectomy + segmentectomy group included six cases of extended sleeve lobectomy with positive lymph nodes or tumors invading the fissure, for which we would not perform a lobectomy + wedge resection. Furthermore, comparing lobectomy + segmentectomy to bilobectomy or pneumonectomy was also difficult due to the current rarity of these procedures. That is, the recent rate of pneumonectomy for primary pulmonary malignancy falls below 1% in Japan (18). Secondly, our study mainly focused on the clinicopathological features and short-term outcomes of lobectomy + segmentectomy. As a result, we included patients with diverse diseases and number of lesions, which resulted in a heterogenous study population. Therefore, an analysis of long-term oncological outcome was not relevant. In order to assess the possible impact of lesion numbers, we compared single and multiple tumor cases (Tables S1,S2). The single tumor group had larger tumor diameter, longer operative time, and higher amount of blood loss when compared to the multiple tumor cases. However, the incidence of lobectomy + segmentectomy cases was similar in both groups, accounting for about one fourth of cases. Overall, more large-scale studies on lobectomy + segmentectomy are necessary to further clarify the long-term outcomes of this procedure.
Conclusions
In conclusion, lobectomy + segmentectomy was selected in our study cohort for the resection of (I) multiple lobe lesions, (II) a lesion invading two lobes, or (III) a lesion with a lymph node invading the bronchial bifurcation. As expected, this procedure had a longer operation time and higher blood loss compared with lobectomy + wedge resection and was also associated with longer drainage periods, longer postoperative hospital stays, and higher rates of overall complications. However, the rates of major complications and mortality was comparable to lobectomy + wedge resection. Data concerning lobectomy + segmentectomy are scarce. However, cases of lobectomy + segmentectomy will increase as segmentectomy gains more popularity, leading to more diverse procedures, including atypical segmentectomies, segmentectomy + segmentectomy, or lobectomy + segmentectomy, becoming part of a surgeon’s armamentarium (2,19-23). Summarily, lobectomy + segmentectomy is a lung-preserving procedure that can benefit patients with multiple or advanced diseases involving two lobes.
Acknowledgments
We thank Enago (www.enago.com) for the English review.
Funding: This work was partly supported by KAKENHI Grant-in-Aid for Young Scientists Japan Society for the Promotion of Science (Grant No. 19K18203 to SN).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-696/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-696/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-696/coif). KS serves as an unpaid editorial board member of Journal of Thoracic Disease from April 2019 to March 2024. SN received a grant from the Japan Society for the Promotion of Science. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Institutional Review Board of Gunma University Hospital (protocol No. HS2019-279, approval on August 13th, 2021). Due to the retrospective nature of our study, patient consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nakazawa S, Shimizu K, Mogi A, et al. VATS segmentectomy: past, present, and future. Gen Thorac Cardiovasc Surg 2018;66:81-90. [Crossref] [PubMed]
- Nakazawa S, Shimizu K, Kawatani N, et al. Surgical outcomes after multiple segmentectomy: a cohort study. J Thorac Dis 2022;14:113-22. [Crossref] [PubMed]
- Suzuki K, Saji H, Aokage K, et al. Comparison of pulmonary segmentectomy and lobectomy: Safety results of a randomized trial. J Thorac Cardiovasc Surg 2019;158:895-907. [Crossref] [PubMed]
- Shiono S, Okumura T, Boku N, et al. Outcomes of segmentectomy and wedge resection for pulmonary metastases from colorectal cancer. Eur J Cardiothorac Surg 2017;51:504-10. [PubMed]
- Yamamoto S, Kawahara K, Shirakusa T, et al. Consecutive left lower sleeve lobectomy and left S3 segmentectomy for a patient with node-negative double lung cancer. Jpn J Thorac Cardiovasc Surg 2006;54:342-4. [Crossref] [PubMed]
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187-96. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol 2015;10:1243-60. [Crossref] [PubMed]
- Zhu XY, Ding C, Xu C, et al. Techniques and outcomes of bronchoplastic and sleeve resection: an 8-year single-center experience. Transl Lung Cancer Res 2021;10:4538-48. [Crossref] [PubMed]
- Galata C, Karampinis I, Roessner ED, et al. Risk factors for surgical complications after anatomic lung resections in the era of VATS and ERAS. Thorac Cancer 2021;12:3255-62. [Crossref] [PubMed]
- Okada M, Tsubota N, Yoshimura M, et al. Extended sleeve lobectomy for lung cancer: the avoidance of pneumonectomy. J Thorac Cardiovasc Surg 1999;118:710-3; discussion 713-4. [Crossref] [PubMed]
- Berthet JP, Paradela M, Jimenez MJ, et al. Extended sleeve lobectomy: one more step toward avoiding pneumonectomy in centrally located lung cancer. Ann Thorac Surg 2013;96:1988-97. [Crossref] [PubMed]
- Chida M, Minowa M, Miyoshi S, et al. Extended sleeve lobectomy for locally advanced lung cancer. Ann Thorac Surg 2009;87:900-5. [Crossref] [PubMed]
- Voltolini L, Gonfiotti A, Viggiano D, et al. Extended sleeve-lobectomy for centrally located locally advanced non-small cell lung cancer is a feasible approach to avoid pneumonectomy. J Thorac Dis 2020;12:4090-8. [Crossref] [PubMed]
- Wang X, Jiang S, You X, et al. Extended Sleeve Lobectomy is an Alternative for Centrally Located Lung Cancer With Superior Short- and Long-term Outcomes. Clin Lung Cancer 2021;22:e621-8. [Crossref] [PubMed]
- Qu JC, Soultanis KM, Jiang L. Surgical techniques and outcome analysis of uniportal video-assisted thoracic surgery complex sleeve lung resection: a 20 case-series study. J Thorac Dis 2021;13:2255-63. [Crossref] [PubMed]
- Hong TH, Cho JH, Shin S, et al. Extended sleeve lobectomy for centrally located non-small-cell lung cancer: a 20-year single-centre experience. Eur J Cardiothorac Surg 2018;54:142-8. [Crossref] [PubMed]
- Committee for Scientific Affairs. Thoracic and cardiovascular surgeries in Japan during 2018: Annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 2021;69:179-212. [Crossref] [PubMed]
- Yajima T, Shimizu K, Mogi A, et al. Thoracoscopic right middle lobe segmentectomy. Gen Thorac Cardiovasc Surg 2019;67:344-7. [Crossref] [PubMed]
- Yajima T, Shimizu K, Mogi A, et al. Medial-basal segment (S(7))-sparing right basal segmentectomy. Gen Thorac Cardiovasc Surg 2020;68:306-9. [Crossref] [PubMed]
- Shimizu K, Nagashima T, Yajima T, et al. Thoracoscopic Medial-Basal Segment Segmentectomy. Ann Thorac Surg 2017;104:e403-6. [Crossref] [PubMed]
- Shimizu K, Mogi A, Yajima T, et al. Thoracoscopic Subsuperior Segment Segmentectomy. Ann Thorac Surg 2017;104:e407-10. [Crossref] [PubMed]
- Nakazawa S, Yajima T, Numajiri K, et al. Superior Lingular S(4) Segmentectomy. Ann Thorac Surg 2022;113:e141-4. [Crossref] [PubMed]



