
Surgery is a promising strategy for improving overall survival for stage III-N2 non-small cell lung cancer patients
Highlight box
Key findings
• Clinically, stage III-N2 NSCLC patients usually demonstrate higher degrees of heterogeneity due to the characteristics of the involved lymph nodes. This study found that Surgery improved OS in this population, which is a better choice.
What is known and what is new?
• The effectiveness of surgery for treating stage III NSCLC patients is controversial.
• Our study proved that stage III-N2 NSCLC patients who underwent surgery demonstrated better overall survival compared to those receiving radiotherapy.
What is the implication, and what should change now?
• Surgery is a favorable treatment strategy for advanced-stage lung cancer. We would recommend that doctors utilize surgery more widely for the treatment of stage III-N2 NSCLC patients.
Introduction
Lung cancer has become the leading cause of cancer-associated death worldwide, and its incidence has been increasing every year (1,2). Among the approximately 234,000 lung cancer diagnoses, about 154,000 die due to lung cancer-associated factors (3,4). Commonly, early-stage non-small cell lung cancers (NSCLC), such as stage I and stage II, are treated using a standard surgical approach, followed by adjuvant chemotherapy.
NSCLC patients with stage III who are characterized by N1 involvement (stage III-N1) usually undergo surgery followed by adjuvant chemotherapy. However, the therapeutic strategy of stage III NSCLC patients with N2 involvement (stage III-N2) is a controversial topic in the field of lung cancer. Stage III-N2 NSCLC occurs in approximately 15% of all NSCLC patients, and its incidence rate is relatively lower. Stage III-N2 NSCLC, as a highly heterogeneous category of lung cancer, is mainly characterized by lymph-node involvement, invasion of local structures, and varying tumor sizes (3). Clinically, the 5-year overall survival (OS) rate for stage III-N2 NSCLC patients is only 34%, which decreases to 10% when one or more lymph nodes are involved (3,5). A previous study reported that surgery followed by chemoradiotherapy or chemotherapy is an appropriate method for stage III-N2 small cell lung cancer (SCLC) patients; however, whether surgery and/or chemotherapy could benefit stage III-N2 NSCLC patients also needs to be clarified.
At present, some studies (6,7) have recommended that surgery could be applied for the removal of tumor tissues and prolonging the OS rate of advanced-stage SCLC patients, such as those with stage III-N2 or higher stages. Therefore, to clarify the effects of surgery on stage III-N2 NSCLC patients, we conducted a retrospective study to compare surgery with radiotherapy. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-269/rc).
Methods
Patients
The present retrospective study included 204 adult patients (age >18 years) diagnosed the squamous lung cancer with stage III-N2 who underwent therapy in the Fourth Hospital of Hebei Medical University from January 2008 to December 2013 were selected. Among these stage III-N2 NSCLC patients, 60 underwent surgery (III-surgery group) and 144 received radiotherapy (III-radiotherapy group). The diagnosis of stage III-N2 NSCLC was conducted according to the state III-N2 NSCLC guideline published by the European Society of Chest Physicians (ESMO) 2017 (8).
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the Fourth Hospital of Hebei Medical University (No. 2020KS024) and individual consent for this retrospective analysis was waived.
Inclusive criteria and exclusive criteria
The inclusion criteria were as follows: (I) patients who underwent surgical treatment or radiotherapy; (II) patients with survival records; (III) patients with clinical characteristics including T stage, N stage, as well as basic information including gender, age at diagnosis, and smoking/family history. The exclusion criteria were as follows: (I) patients who previously received adjuvant targeted chemotherapy and radiation therapy; (II) patients with sequential or simultaneous second-primary tumors; (III) patients with missing clinical characteristics or basic information; (IV) four patients had previously undergone the pneumonectomy or lobectomy as a surgical procedure.
Treatments (surgery and radiotherapy)
The surgical processes were conducted as described by the state III-N2 NSCLC guideline published by ESMO in 2017 (8). Radiotherapy planning and delivery were carried out at the same institution according to the Positron emission tomography computer tomography (PET-CT) treatment position and conventional planning CT scans. Radiotherapy was conducted using linear accelerators, with a total radiation dosage ranging from 48–54 Gy and a median dosage of 50 Gy for 6–8 MV X-rays at 1.8–2.0 Gy per fraction 5 days per week, as reported by a previous study (9). The dosage-volume constraints for the organ at the risk (OAR) were applied according to the standard described by a previous study (9).
Chemotherapy was administered using synchronous and sequential chemotherapy. The chemotherapy regimen was platinum-based single-agent or combination chemotherapy, with platinum-based drugs such as cisplatin, carboplatin, nedaplatin and loplatin, and combination drugs including paclitaxel, docetaxel and vincristine. One hundred and thirty patients received chemotherapy in the whole group, of which 34 patients belongs to Surgery group and the other 96 patients were in Radiotherapy group. All patients treated with chemotherapy for 1–6 cycles, with a median of 4 cycles.
Evaluation indexes
The TNM stages were classified as described by the eighth edition of the TNM classification in the Union of the International Cancer Control (UICC) (10). Clinical characteristics, such as T stage, N stage, adjuvant chemotherapy, and basic information (including gender, age at diagnosis, and smoking/family history) were evaluated in this study. The ECOG scores of patients were evaluated and the comorbidities of hypertension or diabetes were also determined. Moreover, the OS of patients was also evaluated according to a previously reported study (11).
Statistical analysis
The professional statistical software 22.0 (SPSS, Chicago, IL, USA) was used to analyze the data in this study. Tukey’s post hoc test validated analysis of variance (ANOVA) test was used to compare the measurement data between groups. The Chi-square test was applied to analyze the clinical characteristics or basic information between the surgery and radiotherapy groups. The Kaplan-Meier approach was utilized to analyze the OS of patients. A multivariate Cox proportional hazards model was generated to analyze the OS of patients. P<0.05 was considered to indicate a statistically significant difference.
Results
Basic characteristics for patients with stage III-N2 NSCLC
Among the 204 stage III-N2 NSCLC patients, 60 patients underwent surgery and 144 patients received radiotherapy. There were no marked differences in age, gender, smoking history, and family history between patients in the surgery and radiotherapy groups (Table 1). Therefore, the clinical parameters between the surgery and radiotherapy groups were comparable.
Table 1
| Characteristics | Surgery (n=60) | Radiotherapy (n=144) | P |
|---|---|---|---|
| Age, mean ± SD (years) | 57.53±8.87 | 61.94±9.17 | >0.05 |
| Gender | 0.063 | ||
| Male | 60 | 140 | |
| Female | 0 | 4 | |
| Smoking status | 0.084 | ||
| Never | 11 | 11 | |
| Yes | 49 | 133 | |
| Family history | 0.108 | ||
| Yes | 7 | 12 | |
| No | 53 | 132 | |
| Adjuvant chemotherapy | 0.058 | ||
| Yes | 34 | 93 | |
| No | 26 | 51 | |
SD, standard deviation.
Clinical characteristics of patients with stage III-N2 NSCLC
There was also a significant difference in the disease stages (IIIa and IIIb) between the surgery and radiotherapy groups (Table 2, P<0.001). Compared with the surgical group, there were more patients with ECOG scores of 1 and 2 and fewer patients with ECOG scores of 0 in the radiotherapy group (Table 3, P<0.001). Moreover, among the 60 stage III-N2 NSCLC patients in the surgery group, there were 27 patients (45%) with hypertension, and 75 hypertensive patients (52.08%) in the radiotherapy group (Table 3). Meanwhile, among the stage III-N2 NSCLC patients, there were no diabetic patients in the surgery group and one diabetic patient in the radiotherapy group (Table 3). Therefore, there was a significant difference in the comorbidities between stage III-N2 NSCLC patients in the surgery and radiotherapy groups (Table 3, P=0.011).
Table 2
| Disease stage | Surgery (n=60) | Radiotherapy (n=144) | P |
|---|---|---|---|
| IIIa, n (%) | 38 (63.33) | 39 (27.08) | <0.001 |
| IIIb, n (%) | 22 (36.67) | 105 (72.92) |
Table 3
| Characteristics | Surgery (n=60) | Radiotherapy (n=144) | P |
|---|---|---|---|
| ECOG, n (%) | <0.001 | ||
| 0 | 53 (88.33) | 17 (11.81) | |
| 1 | 7 (11.67) | 109 (75.69) | |
| 2 | 0 (0.00) | 18 (12.50) | |
| Comorbidity, n (%) | 0.011 | ||
| Hypertension | 27 (45.0) | 75 (52.08) | |
| Diabetes | 0 (0.00) | 1 (0.70) |
ECOG, Eastern Cooperative Oncology Group.
Effects of surgery and radiotherapy on the OS of stage III-N2 NSCLC patients
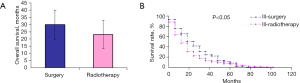
Our findings showed that the OS rate was higher significantly in stage III-N2 NSCLC patients in the surgery group compared to that in the radiotherapy group (Figure 1A, P<0.05). The Kaplan-Meier analysis also demonstrated that the OS of III-N2 NSCLC patients was markedly better in surgery group patients, as compared to those in the radiotherapy group (Figure 1B, P<0.05).
Surgery is an independent prognostic factor for predicting the OS of stage III-N2 NSCLC patients
A univariate analysis was conducted to assess the prognostic value of surgery for predicting OS of stage III-N2 NSCLC patients. The results indicated that age, T stage, surgery, disease stage, and adjuvant chemotherapy were critical factors influencing OS. Multivariate analysis was also performed to verify the respective effects of the above factors. The multivariate proportional hazards model findings showed that the age, T stage, surgery, disease stage, and adjuvant chemotherapy were the independent prognostic predictors for OS of stage III-N2 NSCLC patients (Table 4).
Table 4
| Variables | HR | 95% CI | P | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | 0.198 | 0.135 | 0.227 | 0.019 |
| ECOG | 0.796 | 0.297 | 1.073 | 0.213 |
| Surgery | 1.073 | 0.784 | 1.308 | 0.001 |
| T-stage | 0.886 | 0.569 | 1.342 | 0.027 |
| Disease stage | 0.770 | 0.354 | 1.033 | 0.019 |
| Adjuvant chemotherapy | 0.454 | 0.277 | 0.609 | 0.073 |
| Comorbidity | 0.391 | 0.189 | 0.687 | 0.139 |
HR, hazard ratio; CI, confidence interval; ECOG, Eastern Cooperative Oncology Group.
Discussion
Clinically, stage III-N2 NSCLC patients generally demonstrate a higher degree of heterogeneity due to the characteristics of the lymph nodes involved. Therefore, the treatment of stage III-N2 NSCLC is also considered to be the most controversial issue for lung cancer therapy (3). The newest American Joint Committee on Cancer (version 8) has categorized the stage III-N2 into stages III-N2a1, III-N2a2, and III-N2b, according to the extent of nodal involvement affecting OS and the survival of lung cancer patients.
It has been extensively accepted that surgery resection is not an appropriate strategy for the treatment of advanced-stage lung cancer patients (12). In fact, few stage III lung cancer patients undergo surgery and/or chemotherapy; however, radiotherapy has been proven to be more favorable for treating these patients (13). Also, surgery is not recommended for patients diagnosed with N2 involvement but induction treatment followed by surgery is recommended for patients with minimal nodal involvement or microscopic nodal involvement (3). Therefore, the effectiveness of the surgery for treating stage III NSCLC patients remains controversial, as described by the previous reports (14).
Therefore, in this study, we included a total of 204 stage III-N2 NSCLC patients to verify the abovementioned controversial issues. We proved that stage III-N2 NSCLC patients who underwent surgery demonstrated better OS compared to those who received radiotherapy. As for the beneficial effects of surgery for treating stage III lung cancer patients, the present findings are consistent with those of a previous study (7) but are also inconsistent with some surgery-treated lung cancers (15,16).
In recent years, numerous studies have shown that surgical treatment provides a remarkably improved 5-year survival rate for stage I or stage II lung cancer patients compared to those undergoing other treatments (17-19). Therefore, surgery could also be considered to be a promising treatment for some limited-stage lung cancers. Liu et al. (20) reported that surgery-based treatment could improve the survival of most stage I SCLC patients as well as a proportion of stage II/III patients. In our study, the survival of stage III-N2 NSCLC patients who underwent the surgery was evaluated to be 29.87 months, which was significantly longer than that of patients who received radiotherapy. It might be that the stage III-N2 NSCLC patients who received radiotherapy initially achieved an improvement due to the clearance of sensitive tumor cells. However, insensitive tumor cells are also alive and could be amplified thereafter, which could make radiotherapy less effective. Moreover, the multivariate proportional hazards models showed that age, T stage, surgery, disease stage, and adjuvant chemotherapy were the independent prognostic predictors for the OS of stage III-N2 NSCLC patients. Therefore, surgery would be a favorable treatment strategy for advanced-stage lung cancer. We would recommend that doctors utilize surgery more widely in the treatment of stage III-N2 NSCLC patients.
However, this study also showed the limitation that the sample size of the patients in two groups was small, which could influence the significant comparative value. In the following study, we would involve a large number of patients to further confirm the findings in this study.
Conclusions
In this study, we demonstrated that surgery is associated with improved OS of stage III-N2 NSCLC patients. Thus, for stage III-N2 NSCLC patients, we recommend that surgery is applied clinically. Furthermore, surgery and adjuvant chemotherapy could be combined or coordinated for the individualized therapy of NSCLC patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-269/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-269/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-269/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-269/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics Committee of the Fourth Hospital of Hebei Medical University (No. 2020KS024) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer Statistics, 2021. CA Cancer J Clin 2021;71:7-33. [Crossref] [PubMed]
- Tezel C, Dogruyol T, Alpay L, et al. Prognostic Importance of the Lymph Node Factor in Surgically Resected Non-Small Cell Lung Cancer. Thorac Cardiovasc Surg 2020;68:183-9. [Crossref] [PubMed]
- Behera M, Steuer CE, Liu Y, et al. Trimodality Therapy in the Treatment of Stage III N2-Positive Non-Small Cell Lung Cancer: A National Cancer Database Analysis. Oncologist 2020;25:e964-e975. [Crossref] [PubMed]
- Jakobsen E, Olsen KE, Bliddal M, et al. Forecasting lung cancer incidence, mortality, and prevalence to year 2030. BMC Cancer 2021;21:985. [Crossref] [PubMed]
- Zhong WZ, Wang Q, Mao WM, et al. Gefitinib Versus Vinorelbine Plus Cisplatin as Adjuvant Treatment for Stage II-IIIA (N1-N2) EGFR-Mutant NSCLC: Final Overall Survival Analysis of CTONG1104 Phase III Trial. J Clin Oncol 2021;39:713-22. [Crossref] [PubMed]
- Gao L, Shen L, Wang K, et al. Propensity score matched analysis for the role of surgery in stage III small cell lung cancer based on the eighth edition of the TNM classification: a population study of the US SEER database and a Chinese hospital. Lung Cancer 2021;162:54-60.
- Chai Y, Ma Y, Feng W, et al. Effect of surgery on survival in patients with stage III N2 small cell lung cancer: propensity score matching analysis and nomogram development and validation. World J Surg Oncol 2021;19:258. [Crossref] [PubMed]
- Postmus PE, Kerr KM, Oudkerk M, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2017;28:iv1-iv21. [Crossref] [PubMed]
- Wei W, Zhou J, Zhang Q, et al. Postoperative intensity-modulated radiation therapy reduces local recurrence and improves overall survival in III-N2 non-small-cell lung cancer: A single-center, retrospective study. Cancer Med 2020;9:2820-32. [Crossref] [PubMed]
- Goldstraw P, Chansky K, Crowley J, et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2016;11:39-51. [Crossref] [PubMed]
- Taugner J, Eze C, Käsmann L, et al. Pattern-of-failure and salvage treatment analysis after chemoradiotherapy for inoperable stage III non-small cell lung cancer. Radiat Oncol 2020;15:148. [Crossref] [PubMed]
- Baize N, Monnet I, Greillier L, et al. Second-line treatments of small-cell lung cancers. Expert Rev Anticancer Ther 2017;17:1033-43. [Crossref] [PubMed]
- Tartarone A, Giordano P, Lerose R, et al. Progress and challenges in the treatment of small cell lung cancer. Med Oncol 2017;34:110. [Crossref] [PubMed]
- Turner SR, Butts CA, Debenham BJ, et al. Is lobectomy superior to sublobar resection for early-stage small-cell lung cancer discovered intraoperatively? Interact Cardiovasc Thorac Surg 2019;28:41-4. [Crossref] [PubMed]
- Putora PM, Leskow P, McDonald F, et al. International guidelines on stage III N2 nonsmall cell lung cancer: surgery or radiotherapy? ERJ Open Res 2020; [Crossref] [PubMed]
- Chaft JE, Rimner A, Weder W, et al. Evolution of systemic therapy for stages I-III non-metastatic non-small-cell lung cancer. Nat Rev Clin Oncol 2021;18:547-57. [Crossref] [PubMed]
- Combs SE, Hancock JG, Boffa DJ, et al. Bolstering the case for lobectomy in stages I, II, and IIIA small-cell lung cancer using the National Cancer Data Base. J Thorac Oncol 2015;10:316-23. [Crossref] [PubMed]
- Merritt RE, Abdel-Rasoul M, D'Souza DM, et al. Racial Disparities in Overall Survival and Surgical Treatment for Early Stage Lung Cancer by Facility Type. Clin Lung Cancer 2021;22:e691-8. [Crossref] [PubMed]
- Nachira D, Congedo MT, Tabacco D, et al. Surgical Effectiveness of Uniportal-VATS Lobectomy Compared to Open Surgery in Early-Stage Lung Cancer. Front Surg 2022;9:840070. [Crossref] [PubMed]
- Liu T, Chen Z, Dang J, et al. The role of surgery in stage I to III small cell lung cancer: A systematic review and meta-analysis. PLoS One 2018;13:e0210001. [Crossref] [PubMed]
(English Language Editor: A. Kassem)


