
Chest computed tomography scan utilization and diagnostic outcomes in chronic cough patients with normal chest X-rays: analysis of routinely collected data of a tertiary academic hospital
Highlight box
Key findings
• Chest CT scans were frequently prescribed to chronic cough patients with normal X-rays (20.0%), but the diagnostic yield for critical findings (e.g., malignancy or infectious disease) was less than 1%.
What is known and what is new?
• There is controversy over the utility of chest CT scans in improving cough outcomes for patients with chronic cough and normal chest X-rays.
• In the present study, chest CT scans identified critical conditions in less than 1% of patients.
What is the implication, and what should change now?
• Given the low diagnostic yield and potential risk of radiation harm, performing routine chest CT scans may not be warranted for chronic cough patients with normal chest X-rays.
Introduction
Chronic cough, typically defined as a cough lasting for over 8 weeks in adults, is a prevalent medical condition (1-3). Also, it is a major cause of morbidity, posing a substantial impact on patient quality of life (QoL) (4-7).
Identifying and controlling treatable traits is crucial in managing patients with chronic cough. The current cough guidelines recommend detailed history taking, physical examination, and chest X-rays as part of the initial assessments (8-10). Chest X-rays especially are routinely recommended to screen out critical lung parenchymal diseases. However, the diagnostic roles of chest computed tomography (CT) scan remain controversial in patients with chronic cough with normal chest X-rays.
Chest CT scans may be useful in detecting lung lesions that are not readily visible on chest X-rays; however, the causal relationships between CT findings and cough are often difficult to determine. In addition, there is a concern about the potential risk of radiation exposure (8,11). The European Respiratory Society (ERS) cough guideline task force developed a conditional recommendation against routine chest CT scans in chronic cough patients with normal chest X-rays and physical examination (8). However, the level of supporting evidence was very low (8), and to date, the number and sample size of relevant studies remains small (12-14).
Routinely collected data (RCD), such as health administrative data or electronic health records (EHRs), can offer an opportunity to analyze real-world practice patterns and clinical outcomes on a large scale. We recently established a retrospective cohort of patients with chronic cough using an academic institutional EHR database (15). Utilizing the cohort database, we investigated the real-world application pattern and diagnostic outcomes of chest CT scans in chronic cough patients with normal chest X-rays. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1404/rc).
Methods
Study population
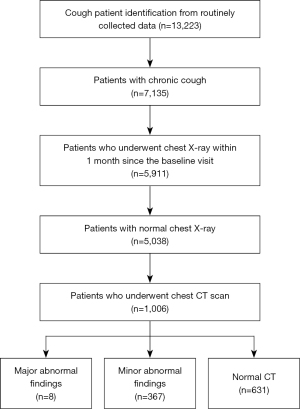
This is a retrospective analysis of adult patients with chronic cough referred to allergy and asthma clinics between January 2010 and August 2018. The patient cohort was established using the RCD from the tertiary institutional EHR, and the study methodology has been reported previously (15). Briefly, chronic cough cases were identified using the search term “cough” or “coughing” (in English or Korean) in the EHR data field of the chief complaint, combined with the data field for the duration of chronic cough (>8 weeks). Patients were excluded if other symptoms, such as hemoptysis, fever, chest discomfort, or pain, were indicated as co-chief complaints. The selection flow of the study population is presented in Figure 1. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the hospital institutional review board of Asan Medical Center (No. 2019-0511) and individual consent for this retrospective analysis was waived.
Baseline clinical information
Baseline data were retrieved from routinely collected case report forms: demographics, present illness, concomitant symptoms, smoking history, and past medical history. The case report form was filled out by specialist nurses and physicians (allergists or pulmonologists) at the clinics.
Chest X-ray and CT scan data
Records of chest X-rays conducted within 1 month from the baseline visit were retrieved with records of the subsequently performed chest CT scans. All imaging test outcomes were based on formal reports by radiologists. Chest X-rays were defined as abnormal if the patient had bronchiectasis, tuberculosis, malignancy, or other grossly abnormal parenchymal lesion according to the formal interpretation of the radiologist and were otherwise normal.
This RCD based study presents challenges in determining the causal relationships between CT findings and chronic cough. The CT findings were arbitrarily classified into three groups based on the needs for immediate management: (I) major abnormal; (II) minor abnormal; or (III) normal. Major abnormal findings included malignancy, infection, or critical lung diseases warranting immediate treatment decisions. Minor abnormal findings included any other abnormalities that likely did not warrant immediate treatment, such as benign nodules, focal fibrosis, fibrocalcified lesion, subsegmental atelectasis, bronchial wall thickening, bronchiectasis, or calcified nodule or granuloma.
Statistical analysis
Continuous data were expressed as mean ± standard deviation or median [interquartile range (IQR)]. Categorical data were calculated as the number of patients and percentages.
Group differences were assessed using Student’s t-test, Mann-Whitney U-tests, or chi-square tests. One-way analysis of variance was conducted to examine differences among the three groups (i.e., major, minor, vs. normal CT findings), and all calculations were performed using the Stata 15.1 software (Stata Corp., College Station, TX, USA). A two-sided P value of <0.05 was considered statistically significant.
Results
Study population
Of the 7,135 patients with chronic cough identified from the routinely collected healthcare database, 5,911 patients underwent chest X-rays within 1 month of the baseline visit. Of these, 5,038 patients had normal chest X-rays and were finally analyzed (Figure 1). Compared with patients with abnormal chest X-rays, those with normal chest X-rays were younger, with a greater proportion of females, and had shorter cough duration, less smoking history, but more self-reported history of respiratory diseases. The detailed characteristics are presented in Table S1.
Baseline factors associated with chest CT scan utilization
Among the 5,038 chronic cough patients with normal chest X-rays, chest CT scans were performed in 1,006 patients (20.0%); and 459 (45.6%) and 547 (54.4%) of patients underwent contrast and non-contrast chest CT scans, respectively. Their baseline characteristics and demographics were compared according to chest CT scan utilization (Table 1). Chest CT scans were performed significantly more often in patients who had longer cough duration, older age, male sex, more smoking history, more lung parenchymal diseases, or more non-respiratory comorbidities, including malignancy.
Table 1
| Parameters | Patients who underwent chest CT (n=1,006, 20.0%) | Patients who did not undergo chest CT (n=4,032, 80.0%) | P value |
|---|---|---|---|
| Cough duration (months) | 8 [3–12] | 6 [3–12] | 0.002 |
| Age (years) | 57.3±12.1 | 49.7±16.0 | <0.001 |
| Female sex (%) | 58.6 | 66.1 | <0.001 |
| Smoking history (%) | |||
| Never smoker | 65.3 | 72.4 | <0.001 |
| Former smoker | 23.3 | 15.9 | <0.001 |
| Current smoker | 9.6 | 8.6 | 0.288 |
| Physician-diagnosed history | |||
| Respiratory disease (%) | |||
| Allergic rhinitis | 6.6 | 13.4 | <0.001 |
| Chronic rhinosinusitis | 19.3 | 18.5 | 0.569 |
| Asthma | 19.4 | 22.0 | 0.068 |
| Chronic obstructive pulmonary disease | 2.7 | 1.0 | <0.001 |
| Bronchiectasis | 1.1 | 0.1 | 0.001 |
| Pulmonary tuberculosis | 0.7 | 0.02 | <0.001 |
| Interstitial lung disease | 1.4 | 0.2 | <0.001 |
| None | 59.3 | 55.9 | 0.047 |
| Non-respiratory disease (%) | |||
| Gastroesophageal reflux disease | 12.9 | 9.7 | 0.002 |
| Malignancy | 14.5 | 4.9 | <0.001 |
| Heart failure | 0.4 | 0.5 | 0.834 |
| Hypertension | 28.5 | 20.4 | <0.001 |
| Diabetes mellitus | 11.0 | 7.4 | <0.001 |
| None | 48.4 | 66.3 | <0.001 |
| Concomitant symptoms (%) | |||
| Abnormal throat sensation* | 73.4 | 72.5 | 0.571 |
| Sputum production | 62.4 | 59.5 | 0.093 |
| Postnasal drip/throat clearing | 32.9 | 39.8 | <0.001 |
| Rhinorrhea | 29.8 | 34.2 | 0.009 |
| Sneeze | 29.4 | 32.0 | 0.113 |
| Nasal obstruction | 21.5 | 28.6 | <0.001 |
| Dyspnea | 26.2 | 24.3 | 0.208 |
| Wheeze | 19.7 | 17.7 | 0.146 |
| Hoarseness | 10.7 | 11.7 | 0.400 |
| Throat pain | 10.0 | 11.4 | 0.217 |
| Heartburn | 19.3 | 19.4 | 0.965 |
| Acid regurgitation | 13.8 | 16.8 | 0.022 |
Data were presented as mean ± standard deviation, median [interquartile range], or percentages. *, globus, tickling, or dryness. CT, computed tomography.
Diagnostic outcomes of chest CT scans in chronic cough patients with normal chest X-rays
Of the 1,006 patients with chest CT scans, 8 (0.8%) had major abnormal findings, 367 (36.5%) had minor findings, and 631 (62.7%) had normal CT. The major and minor findings are presented in Figure 2 and Table 2. Major abnormal findings were noted in 4 cases with pneumonia, 2 with pulmonary tuberculosis, and 2 with lung cancer. Patients with minor CT findings comprised 69 cases with focal fibrosis, 59 noncalcified nodule/benign small infiltrates, 59 subsegmental atelectasis, 45 bronchial wall thickening, 41 bronchiectasis, 27 ground glass opacity, 25 calcified nodule/calcified granuloma, 23 emphysema, 13 bulla, 5 pleural thickening/pleural plaque, and 1 subpleural reticular opacity (Figure 2 and Table 2).

Table 2
| CT findings | Proportion of patients, n=1,006 (%) |
|---|---|
| Major findings | |
| Pneumonia | 4 (0.4) |
| Pulmonary tuberculosis | 2 (0.2) |
| Lung cancer | 2 (0.2) |
| Minor findings | |
| Fibrocalcified lesion/focal fibrosis | 69 (6.9) |
| Noncalcified nodule/benign small infiltrates | 59 (5.9) |
| Subsegmental atelectasis | 59 (5.9) |
| Bronchial wall thickening | 45 (4.5) |
| Bronchiectasis | 41 (4.1) |
| Ground glass opacity | 27 (2.7) |
| Calcified nodule/calcified granuloma | 25 (2.5) |
| Emphysema | 23 (2.3) |
| Bulla | 13 (1.3) |
| Pleural thickening/pleural plaque | 5 (0.5) |
| Subpleural reticular opacity | 1 (0.1) |
CT, computed tomography.
Comparison of baseline patient characteristics according to chest CT findings
Baseline characteristics were compared according to chest CT findings (Table 3). Across the three groups, there were no statistically significant differences in the baseline characteristics, such as cough duration, age, sex, history of smoking and respiratory disease, or concomitant symptoms. The proportion of patients with dyspnea or history of malignancy was significantly different (P<0.001), but the differences were only significant between normal and minor findings, but not with major findings.
Table 3
| Parameters | Major CT findings (n=8) | Minor CT findings (n=367) | Normal CT (n=631) | P value |
|---|---|---|---|---|
| Cough duration (months) | 6.5 [3–12] | 8 [3–12] | 7 [3–12] | 0.674 |
| Age (years) | 57.5±12.9 | 56.8±12.6 | 57.5±11.7 | 0.710 |
| Female sex, n (%) | 5 (62.5) | 208 (56.7) | 377 (59.7) | 0.611 |
| Current or former smokers, n (%) | 1 (14.3) | 122 (33.2) | 208 (33.0) | 0.576 |
| Physician-diagnosed history, n (%) | ||||
| Respiratory disease | 2 (25.0) | 141 (38.4) | 266 (42.2) | 0.363 |
| Allergic rhinitis | 0 (0.0) | 16 (4.4) | 50 (7.9) | 0.069 |
| Chronic rhinosinusitis | 2 (25.0) | 69 (18.8) | 123 (19.5) | 0.792 |
| Asthma | 1 (12.5) | 72 (19.6) | 122 (19.3) | 0.977 |
| Chronic obstructive pulmonary disease | 0 (0.0) | 9 (2.5) | 18 (2.9) | 0.872 |
| Bronchiectasis | 0 (0.0) | 4 (1.1) | 7 (1.1) | 1.000 |
| Pulmonary tuberculosis | 0 (0.0) | 1 (0.3) | 6 (1.0) | 0.464 |
| Interstitial lung disease | 0 (0.0) | 8 (2.2) | 6 (1.0) | 0.250 |
| Non-respiratory disease | ||||
| Gastroesophageal reflux disease | 2 (25.0) | 45 (12.3) | 83 (13.2) | 0.418 |
| Malignancy | 1 (12.5) | 21 (5.7) | 124 (19.7) | <0.001 |
| Hypertension | 2 (25.0) | 103 (28.1) | 182 (28.8) | 0.947 |
| Diabetes mellitus | 0 (0.0) | 36 (9.8) | 75 (11.9) | 0.469 |
| Concomitant symptoms, n (%) | ||||
| Abnormal throat sensation* | 8 (100.0) | 279 (76.0) | 45 (71.5) | 0.063 |
| Sputum production | 5 (62.5) | 242 (65.9) | 381 (60.4) | 0.193 |
| Postnasal drip/throat clearing | 4 (50.0) | 129 (35.2) | 198 (31.4) | 0.264 |
| Rhinorrhea | 2 (25.0) | 97 (26.4) | 201 (31.9) | 0.210 |
| Nasal obstruction | 4 (50.0) | 74 (20.2) | 138 (21.9) | 0.114 |
| Dyspnea | 0 (0.0) | 72 (19.6) | 192 (30.4) | <0.001 |
| Wheeze | 0 (0.0) | 71 (19.4) | 127 (20.1) | 0.501 |
| Hoarseness | 2 (25.0) | 40 (10.9) | 66 (10.5) | 0.315 |
| Throat pain | 0 (0.0) | 35 (9.5) | 66 (10.5) | 0.857 |
| Heartburn | 1 (12.5) | 75 (20.4) | 118 (18.7) | 0.755 |
| Acid regurgitation | 2 (25.0) | 54 (14.7) | 83 (13.2) | 0.358 |
Data were presented as mean ± standard deviation, median [interquartile range], or number (percentages). *, globus, tickling, or dryness. CT, computed tomography.
Discussion
Using a large academic institutional EHR collected over 8 years, we investigated the real-world utilization of chest CT scans and diagnostic outcomes in chronic cough patients with normal chest X-rays. Despite normal X-rays, chest CT scans were frequently prescribed to chronic cough patients (20%). Abnormalities were observed in 37.3% of CT scans, but the critical findings that warrant immediate treatment decisions, such as malignancy or infection, were identified in less than 1%. An association with cough was unclear in the minor findings (36.5%). Based on the diagnostic yield and potential radiation harm, a routine chest CT scan may not be warranted in chronic cough patients with normal chest X-rays.
The decision to prescribe a chest CT scan can depend on several factors, including patient characteristics, medical needs, and referral and insurance coverage system. In this study utilizing the RCD of a tertiary allergy and asthma clinic, we first analyzed patient characteristics associated with the decision of the allergy or pulmonology specialist physicians to conduct a CT scan. We observed that CT scans were significantly associated with longer cough duration, older age, male sex, smoking history, history of lung parenchymal diseases, and non-respiratory comorbidities such as malignancy. The reasons for the associations are not clear, but it may be partly because such factors are perceived as risk factors of malignancy and they may influence patient preferences and physician decision. These findings represent baseline factors influencing a physician to prescribe chest CT scans (Table 1). However, none of these factors were specifically associated with the presence of major abnormal findings (vs. normal or minor findings) (Table 2). Our analyses were based on routinely collected parameters, and there may be unmeasured factors that could predict critical outcomes on CT scans; however, the diagnostic yield for malignancy or infection was less than 1%, and the gap between the decision of the physician and major CT findings may indicate the need to identify predictors to guide prescription of CT scans in patients with normal chest X-rays.
Several outcomes are relevant in the decision-making for diagnostic tests, such as (I) diagnostic yield, (II) sensitivity and specificity, and (III) impact on treatment decisions or outcomes. In this study, we calculated the diagnostic yield of a chest CT scan for malignancy or infection (defined “major abnormal findings”). Given the difficulty in determining causal relationships between CT findings and cough outcomes, setting “reference standards (such as abnormal CT findings causally related to cough)” is challenging and thus may not be ideal for utilizing sensitivity and specificity in clinical decision-making. The impact on treatment decisions has been evaluated by Descazeaux and colleagues in France (14), who found that chest CT scans had an impact on chronic cough management among only 3.0% of 595 patients with normal chest X-rays, leading to cough improvement in 1.5%. Although different outcomes were utilized, our findings align with the French study (14) in that the diagnostic yield for critical findings that warrant immediate treatment decisions may be low if patients have normal chest X-rays.
In our view, the clinical decision to prescribe a chest CT scan despite a normal chest X-ray should be personalized. In addition to the French study, our findings suggest that the diagnostic yield for medically critical conditions can be as low as 1%. However, health concern substantially impacts the QoL of chronic cough patients (4); in this regard, a chest CT scan to exclude critical lung diseases could help to reduce health anxiety and improve their health-related QoL. Also, early diagnosis of hidden critical lung lesions through chest CT scans may improve the prognosis of patients with chronic cough, especially those with lung cancer, which would be additional benefit of CT scan beyond etiological evaluation. Thus, the choice of chest imaging modality may depend on clinical context. Meanwhile, a modeling study in the USA reported that lung cancer was estimated to be the most common projected radiation-related cancer, the future risk of which can be three times higher in females than in males (11). Utilizing the cohort database, we investigated the real-world application pattern and diagnostic outcomes of chest CT scans in chronic cough patients with normal chest X-rays. Further studies are warranted to develop clinical evidence to guide the decision making on chest CT scans.
Several limitations of our study should be taken into consideration. Firstly, this is a retrospective analysis of routinely collected healthcare data at a tertiary institution in South Korea. Therefore, the external validity may be limited. However, the findings were derived from allergy and asthma clinics, not specialist cough clinics, and thus may be extrapolated to a similar setting. Secondly, there is a risk of misclassification because the baseline parameters were collected during routine practice and relied on patient reporting. Additionally, there was no information on physical examination findings in a structured case report form. Third, our classification of chest CT findings (major or minor) was arbitrary, and we could not confirm causal relationships between CT findings and chronic cough. To our knowledge, there is no consensus on how to classify CT findings in relation to cough causes and outcomes. We presented the absolute number of each finding for future use in secondary analyses such as meta-analyses. Fourth, we could not differentiate patients with refractory chronic cough in this RCD. Further studies are warranted to evaluate benefits of chest CT scans in patients with refractory chronic cough, including etiological confirmation and psychological impact. Despite these limitations, the present study is the largest analysis to date, and also assessed the patient factors associated with CT utilization (practice pattern) and diagnostic outcomes.
Conclusions
In conclusion, although chest CT scans are frequently prescribed for chronic cough patients with normal chest X-rays, the diagnostic yield for malignancy or infectious diseases may be very low (<1%). Given the potential radiation harm, routine chest CT scans may not be warranted for all chronic cough patients with normal chest X-rays. Further studies are warranted to develop clinical evidence to guide the use of chest CT scans in these patients.
Acknowledgments
Funding: This work was partly supported by a research grant from the Investigator-Initiated Studies Program of Merck Sharp & Dohme Corp. The opinions expressed in this paper are those of the authors and do not necessarily represent those of Merck Sharp & Dohme Corp.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Thoracic Disease for the series “Novel Insights Into Chronic Cough”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1404/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1404/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1404/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1404/coif). The series “Novel Insights Into Chronic Cough” was commissioned by the editorial office without any funding or sponsorship. WJS serves as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Journal of Thoracic Disease. WJS declares academic grants from MSD, consulting fees from MSD, GSK, AstraZeneca, and Novartis, and honoraria from MSD, GSK, AstraZeneca, and Novartis. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the hospital institutional review board of Asan Medical Center (No. 2019-0511) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dicpinigaitis PV. Clinical perspective—cough: an unmet need. Current Opinion in Pharmacology 2015;22:24-8. [Crossref] [PubMed]
- Chung KF, McGarvey L, Song WJ, et al. Cough hypersensitivity and chronic cough. Nat Rev Dis Primers 2022;8:45. [Crossref] [PubMed]
- Song WJ, Chang YS, Faruqi S, et al. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J 2015;45:1479-81. [Crossref] [PubMed]
- French CL, Irwin RS, Curley FJ, et al. Impact of chronic cough on quality of life. Arch Intern Med 1998;158:1657-61. [Crossref] [PubMed]
- Birring SS, Prudon B, Carr AJ, et al. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax 2003;58:339-43. [Crossref] [PubMed]
- Won HK, Lee JH, An J, et al. Impact of Chronic Cough on Health-Related Quality of Life in the Korean Adult General Population: The Korean National Health and Nutrition Examination Survey 2010-2016. Allergy Asthma Immunol Res 2020;12:964-79. [Crossref] [PubMed]
- Yu CJ, Song WJ, Kang SH. The disease burden and quality of life of chronic cough patients in South Korea and Taiwan. World Allergy Organ J 2022;15:100681. [Crossref] [PubMed]
- Morice AH, Millqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J 2020;55:1901136. [Crossref] [PubMed]
- Irwin RS, French CL, Chang AB, et al. Classification of Cough as a Symptom in Adults and Management Algorithms: CHEST Guideline and Expert Panel Report. Chest 2018;153:196-209. [Crossref] [PubMed]
- Song DJ, Song WJ, Kwon JW, et al. KAAACI Evidence-Based Clinical Practice Guidelines for Chronic Cough in Adults and Children in Korea. Allergy Asthma Immunol Res 2018;10:591-613. [Crossref] [PubMed]
- Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med 2009;169:2071-7. [Crossref] [PubMed]
- Truba O, Rybka A, Klimowicz K, et al. Is a normal chest radiograph sufficient to exclude pulmonary abnormalities potentially associated with chronic cough? Adv Respir Med 2018; [Crossref] [PubMed]
- Yu L, Xu X, Niu S. Should computed tomography and bronchoscopy be routine examinations for chronic cough? J Thorac Dis 2020;12:5238-42. [Crossref] [PubMed]
- Descazeaux M, Brouquières D, Didier A, et al. Impact of chest computed tomography scan on the management of patients with chronic cough. ERJ Open Res 2021;7:00222-2021. [Crossref] [PubMed]
- An J, Lee JH, Won HK, et al. Cough Presentation and Cough-Related Healthcare Utilization in Tertiary Care: Analysis of Routinely Collected Academic Institutional Database. Lung 2022;200:431-9. [Crossref] [PubMed]


