Experience of endovascular repair of thoracic aortic dissection after blunt trauma injury in a district general hospital
Introduction
Thoracic aortic injuries are associated with high mortality and are the second most common cause of death in trauma patients after intracranial hemorrhage (1). Thoracic aortic dissection is usually a result of sudden deceleration caused by a traffic accident or fall. The most common rupture location is the aortic isthmus (i.e., the region between the fixed aortic arch and mobile thoracic aorta) (1,2).
Thoracic endovascular aortic repair (TEVAR) is a rapidly evolving therapy for various thoracic aortic pathologies and involves the placement of an endovascular stent graft in the thoracic aorta from a remote peripheral location under imaging guidance. TEVAR is a less invasive option for managing traumatic injuries of the descending aorta in polytraumatized patients. Because TEVAR is less invasive and does not involve thoracotomy or use of heparin, it can be performed even in acutely injured patients without the risk of destabilizing pulmonary, head, or abdominal traumatic lesions. The goal of TEVAR is to reduce the risk of aortic rupture and subsequent fatal hemorrhage.
Methods
Patient demographics
This study was evaluated and approved by the institutional review board of our hospital. In this study, we retrospectively reviewed the clinical data of eight patients with traumatic thoracic dissection who had undergone TEVAR between January 2012 and December 2015 at the vascular surgery department of a district general hospital in Taiwan. All patients had undergone thoracoabdominal computed tomography angiography with an interval slice of 5 mm for evaluation of the entire aorta and possible accompanying injuries in other organ systems. None of the patients had undergone open surgical aortic repair for treating traumatic aortic injuries after TEVAR during the study period. All procedures were performed with the patients under general anesthesia. Cerebrospinal fluid drainage was not performed in any patient, and none of the patients had undergone cervical debranching before stent graft placement. In addition, medical history of the eight patients was reviewed. Data on demography and concurrent injuries were obtained, and the injury severity score (ISS) was calculated. Conformable GORE® TAG® Thoracic Endoprosthesis was used in all patients, and Perclose ProGlide® was used in selected patients. After discharge, the patients were followed up regularly.
Results
Preoperative and postoperative risks
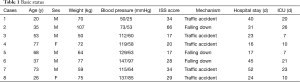
The mean age of the patients was 49±22 years (range, 20–77 years). Of the eight patients assessed, six were men and two were women. All the patients had descending thoracic aortic dissection. All patients had a history of serious trauma and associated severe injury, with a high ISS (range, 17–66). Five patients had been involved in a traffic accident, and three patients had fallen from a height (Table 1).
Full table
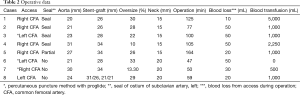
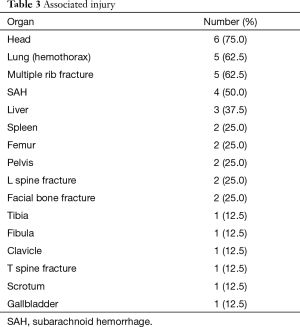
All patients had undergone TEVAR; the endovascular stent graft was placed in the proximal part of the descending aorta. Coverage of the left subclavian artery (LSA) was performed in four patients to achieve a satisfactory proximal sealing zone (Figure 1); none of these four patients developed any complication (Table 2). None of the patients developed paraplegia or left upper extremity ischemia and no patient had died postoperatively. All patients had concomitant injuries (Table 3). Closed head injury and subarachnoid hemorrhage were observed in 75% (6/8) and 50% (4/8) patients, respectively, with traumatic aortic injury. Five (62.5%) patients had multiple rib fractures and hemothorax. Liver injuries and spine fractures were observed in 37.5% (3/8), and spleen injury, pelvic injuries, femur bone fracture, and facial bone injuries were observed in 25% (2/8) of the patients. Perclose ProGlide® was used in three patients. We oversized 10–33% depending on the availability at the time of the trauma and manufacturer instructions. None of the patients died during hospital stay. Moreover, none of the patients showed signs of ischemia or loss of motor function at discharge or during follow-up.

Full table
Full table
Discussion
Traumatic thoracic aortic injuries are uncommon but severe and life-threatening clinical entities. Without appropriate treatment, up to 50% of the initial survivors die within the first 72 hours (3). Parmley and colleagues reported that 88% of the patients died during the first hour and 10% died within two weeks (4). Blunt trauma to the thoracic aorta typically occurs during a high velocity accident because of a combination of sudden deceleration and shearing of the relatively immobile aortic isthmus, which is located distal to the LSA and proximal to the third intercostal artery and is the junction between the relatively mobile aortic arch and the fixed descending aorta. Therefore, the isthmus is the most common location for rupture (50–70% of the cases), followed by the ascending aorta or aortic arch (18%), and the distal thoracic aorta (14%) (3,5). In our study, all patients (8/8, 100%) showed injury to the isthmus. Motor vehicle accidents are responsible for 96.7% of the thoracic aortic injuries, and blunt trauma caused by a fall are responsible for the remaining 3.3% of the injuries (6,7). In our study, 62.5% (5/8) and 37.5% (3/8) of the patients had experienced a traffic accident and a fall, respectively. The incidence rate of a fall from height was higher in the present study than in other studies.
Blunt aortic injury is the most common cause of death in trauma patients, with an overall incidence rate of 0.3% (8). Thoracic aortic injury often goes undiagnosed, unless it is highly suspected by healthcare providers. Therefore, early triage of this condition is critical for survival. However, aortic injuries rarely occur in isolation, and no appropriate cutoff value is available for selecting an appropriate surgical strategy. The first comprehensive review on thoracic aortic injuries was published in 1958 by Parmley et al., who reported an out-of-hospital mortality of 86.2% in 275 cases (4). However, mortality associated with thoracic aortic injury has not reduced much in the last four decades despite considerable advances in prehospital management. In 1994, Williams et al. reported 75% mortality in patients with aortic injury secondary to blunt trauma caused by aortic transection or acute rupture (9). The course for natural progression of a transected thoracic aorta to subsequent rupture is unpredictable. Anxiety pertaining to such rupture is not unfounded, because although 25% of the patients arrive at the hospital on time, their prognosis remains poor, with nearly 30% of these patients dying within 6 hours and 50% of these patients dying within the first 24 hours (10,11).
Multiple organ injuries are frequently observed in patients with traumatic aortic injury, indicating that aortic injury rarely occurs as an isolated injury. Considering its nature, aortic injury is commonly associated with other organ injuries. Fabian et al. and Wahl et al. reported high incidence of multiple organ injuries in patients with traumatic aortic injury, such as closed head injury in 51% of the patients, intracranial hemorrhage in 24%, multiple rib fractures in 46%, pulmonary contusions in 38%, upper limb fractures in 20%, pelvic injuries in 31%, liver injuries in 22%, spine fractures in 4%, spinal cord injuries in 4%, and maxillofacial injuries in 13% of the patients (12-14). In our study, 75% (6/8) of the patients showed closed head injury and 50% (4/8) of the patients showed subarachnoid hemorrhage along with traumatic aortic injury. Five (62.5%) patients sustained multiple rib fractures and hemothorax. Liver injuries and spine fractures were observed in 37.5% (3/8) of the patients, and spleen injury, pelvic injuries, femur bone fracture, and facial bone injuries were observed in 25% of the (2/8) patients. The number of associated injuries reported in the present study was higher than that in other studies because of recent increases in the speed limit on roads, and consequently, higher vehicular speeds. Therefore, evaluating the severity of multiple injuries in these patients is critical and can be performed using ISS. In Fabian et al., the mean ISS was 42.1 (12). In their study, all the patients had a history of serious trauma injury and high ISS (range, 17–66). Smith et al. found that on average, nonsurviving and surviving patients had 4 and 2 associated injuries (14). In the present study, none of the patients died during the hospital stay.
Endovascular repair for chronic infrarenal abdominal aortic aneurysms, introduced in the 1990s, is associated with a low complication rate, less operating time, and a high success rate. Moreover, it appears to be superior to open surgery because it is associated with minor operative trauma and because thoracic endografts have been used for managing blunt aortic injuries since 2001 (15,16). TEVAR is less invasive than conventional surgery. At present, TEVAR is an effective treatment option for treating patients with blunt thoracic aortic injuries (17,18). Because most injuries affect the aortic isthmus and because patients with traumatic thoracic aortic injuries have adequate proximal and distal landing zones, exclusion of an aortic tear with a stent can be performed rather easily. Our experience with traumatic thoracic aortic ruptures suggests that endovascular repair should be the method of choice, especially in unstable multi-trauma patients. TEVAR is associated with better postoperative recovery because it is a minimally invasive procedure that involves excision of an arterial puncture and does not involve creation of a large incision such as those created during thoracotomy, aortic cross-clamping, cardiac bypass, and single-lung ventilation. This in turn prevents major blood pressure variations and coagulopathy, which is advantageous in trauma patients with concomitant injuries, such as pulmonary contusion, in whom a thoracotomy wound could prolong recovery. Moreover, the lower intraoperative blood loss in TEVAR reduces the risks of ischemic events that may lead to spinal cord ischemia and paraplegia, ischemic bowel disease, or kidney failure. Thus far, no studies on endovascular repair of traumatic aortic injuries have reported a paraplegic complication (19). In the present study, we performed isolated TEVAR in eight patients and did not observe paraplegia or major complications. Thus, most severely ill patients admitted to hospitals can survive if they undergo emergency surgery. Because most patients have multiple injuries, evaluation of the severity of these injuries and estimation of survival probability is critical for determining the most appropriate surgical treatment. Moreover, because patients typically have multiple organ injuries, TEVAR, which is minimally invasive, can be performed in tandem with other surgical interventions. Systemic anticoagulation with heparin during TEVAR is rare or occasionally omitted; this is particularly beneficial in patients with concomitant intracranial or abdominal bleeding. In our case series, the timeline for performing TEVAR varied among patients; however, in all patients, TEVAR was performed after treating the life-threatening injuries, which greatly affected the mortality rate.
The aortic isthmus is usually the rupture site in aortic thoracic injuries. Therefore, the distance from the LSA usually allows proximal stent graft fixation. The main challenge is the intentional coverage of the LSA, which is necessary to expand the proximal landing zone and to achieve an adequate seal. We observed complete occlusion in four patients and partial occlusion in the ostium of the LSA in 1 patient while performing TEVAR. None of the patients developed complications during follow-up. Most authors have reported the need for LSA revascularization only for specific indications, such as long aortic segment coverage, prior or concomitant infrarenal aortic replacement, hypoplastic right vertebral artery, patent left internal mammary artery graft, or functioning dialysis fistula in the left arm (20). None of the patients in the present study had indications for LSA revascularization and showed symptoms of subclavian steal syndrome or hand ischemia. A few studies have reported that intentional coverage of the LSA without revascularization is not associated with additional morbidity. However, most studies have reported higher incidence of postoperative arm ischemia and posterior circulation stroke in patients who undergo intentional coverage of the LSA compared with patients who do not undergo intentional coverage (21-24).
Our study has the following limitations. Our sample size was small. Because of constant advances in endovascular repair technologies and the low number of trauma patients undergoing this procedure at each center, following up these patients clinically and scientifically is crucial.
Conclusions
TEVAR is a relatively fast and safe method for treating patients with blunt trauma-associated thoracic aortic injuries and is in consistent with the principles of damage control.
Acknowledgements
We thank all our colleagues in the Department of Medical Research who assisted us in this research.
Funding: This study was supported by a research grant from Tungs’ Taichung Metro-Harbor Hospital Comprehensive Medical Corp (IRB-TTMHH-104C0007).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Richens D, Field M, Neale M, et al. The mechanism of injury in blunt traumatic rupture of the aorta. Eur J Cardiothorac Surg 2002;21:288-93. [Crossref] [PubMed]
- Fattori R, Russo V, Lovato L, et al. Optimal management of traumatic aortic injury. Eur J Vasc Endovasc Surg 2009;37:8-14. [Crossref] [PubMed]
- Demers P, Miller C, Scott Mitchell R, et al. Chronic traumatic aneurysms of the descending thoracic aorta: mid-term results of endovascular repair using first and second-generation stent-grafts. Eur J Cardiothorac Surg 2004;25:394-400. [Crossref] [PubMed]
- Parmley LF, Mattingly TW, Manion WC, et al. Nonpenetrating traumatic injury of the aorta. Circulation 1958;17:1086-101. [Crossref] [PubMed]
- Yilmaz O, Arbatli H, Sirin G, et al. Endovascular treatment of traumatic thoracic aortic aneurysms: report of five cases and review of the literature. Ulus Travma Acil Cerrahi Derg 2010;16:575-8. [PubMed]
- Lee WA, Matsumura JS, Mitchell RS, et al. Endovascular repair of traumatic thoracic aortic injury: clinical practice guidelines of the Society for Vascular Surgery. J Vasc Surg 2011;53:187-92. [Crossref] [PubMed]
- Propper BW, Clouse WD. Thoracic aortic endografting for trauma: a current appraisal. Arch Surg 2010;145:1006-11. [Crossref] [PubMed]
- Arthurs ZM, Starnes BW, Sohn VY, et al. Functional and survival outcomes in traumatic blunt thoracic aortic injuries: An analysis of the National Trauma Databank. J Vasc Surg 2009;49:988-94. [Crossref] [PubMed]
- Williams JS, Graff JA, Uku JM, et al. Aortic injury in vehicular trauma. Ann Thorac Surg 1994;57:726-30. [Crossref] [PubMed]
- Jamieson WR, Janusz MT, Gudas VM, et al. Traumatic rupture of the thoracic aorta: third decade of experience. Am J Surg 2002;183:571-5. [Crossref] [PubMed]
- Lin PH, Huynh TT, Coselli JS, et al. Endovascular Repair of Traumatic Thoracic Aortic Injuries Anatomic considerations, therapeutic limitations, and clinical outcomes. Endovascular Today 2007.
- Fabian TC, Richardson JD, Croce MA, et al. Prospective study of blunt aortic injury: Multicenter Trial of the American Association for the Surgery of Trauma. J Trauma 1997;42:374-80; discussion 380-3. [Crossref] [PubMed]
- Wahl WL, Michaels AJ, Wang SC, et al. Blunt thoracic aortic injury: delayed or early repair? J Trauma 1999;47:254-9; discussion 259-60. [Crossref] [PubMed]
- Smith RS, Chang FC. Traumatic rupture of the aorta: still a lethal injury. Am J Surg 1986;152:660-3. [Crossref] [PubMed]
- Semba CP, Kato N, Kee ST, et al. Acute rupture of the descending thoracic aorta: repair with use of endovascular stent-grafts. J Vasc Interv Radiol 1997;8:337-42. [Crossref] [PubMed]
- Taylor PR, Gaines PA, McGuinness CL, et al. Thoracic aortic stent grafts--early experience from two centres using commercially available devices. Eur J Vasc Endovasc Surg 2001;22:70-6. [Crossref] [PubMed]
- Fattori R, Napoli G, Lovato L, et al. Indications for, timing of, and results of catheter-based treatment of traumatic injury to the aorta. AJR Am J Roentgenol 2002;179:603-9. [Crossref] [PubMed]
- Lachat M, Pfammatter T, Witzke H, et al. Acute traumatic aortic rupture: early stent-graft repair. Eur J Cardiothorac Surg 2002;21:959-63. [Crossref] [PubMed]
- Lin PH, Bush RL, Zhou W, et al. Endovascular treatment of traumatic thoracic aortic injury--should this be the new standard of treatment? J Vasc Surg 2006;43 Suppl A:22A-29A.
- Kotelis D, Geisbüsch P, Hinz U, et al. Short and midterm results after left subclavian artery coverage during endovascular repair of the thoracic aorta. J Vasc Surg 2009;50:1285-92. [Crossref] [PubMed]
- Caronno R, Piffaretti G, Tozzi M, et al. Intentional coverage of the left subclavian artery during endovascular stent graft repair for thoracic aortic disease. Surg Endosc 2006;20:915-8. [Crossref] [PubMed]
- Woo EY, Carpenter JP, Jackson B, et al. Left subclavian artery coverage during thoracic endovascular aortic repair: a single-center experience. J Vasc Surg 2008;48:555-60. [Crossref] [PubMed]
- Peterson BG, Eskandari MK, Gleason TG, et al. Utility of left subclavian artery revascularization in association with endoluminal repair of acute and chronic thoracic aortic pathology. J Vasc Surg 2006;43:433-9. [Crossref] [PubMed]
- Reece TB, Gazoni LM, Cherry KJ, et al. Reevaluating the need for left subclavian artery revascularization with thoracic endovascular aortic repair. Ann Thorac Surg 2007;84:1201-5; discussion 1205. [Crossref] [PubMed]


