Bioresorbable vascular scaffolds—time to vanish?
Why bioresorbable vascular scaffolds (BVS)?
Percutaneous coronary interventions have undergone a stepwise evolution with some tops and some flops since their inception by Andreas Grüntzig in 1977 (1). Bare metal stents (BMS), who suppressed the risk of occlusive dissection and lowered the risk of restenosis (2), dual antiplatelet therapy which decreased the risk of thrombosis, and drug-eluting stents (DES) which minimized the risk of restenosis were all significant advances. Other novelties, such as laser revascularisation and endobrachytherapy were nipped in the bud. Even the latest generation of metallic DES, despite continuous and significant improvements, may impair coronary vasomotion (3), trigger neoatherosclerosis and hamper surgical attempts to treat failed stented segments.
The studies on DES thrombosis in the years 2005 triggered a somewhat artificial emulation amongst stent-makers. From this, rose the concept and development of vanishing stents. Such temporary devices were thought to potentially restore lumen size and flow while disappearing over time and restoring vasomotor tone and normal coronary physiology. The first of these devices to receive CE-approval was the ABSORB (Abbot Vascular, Santa Clara, California, USA) BVS. Its technology relies on a polylactic acid polymer that serves as scaffold platform. It is coated with the antiproliferative drug everolimus, which is almost entirely eluted during the first 3 months after scaffold placement. Polylactic acid has been used in other medical specialities for quite a while as it induces minimal inflammation during bioresorption. The degradation of the polymer starts as early as 6 months after implantation, and full bioresorption may be reached after several years. Polylactic acid is transformed via the cycle of Krebs into carbon dioxide and hydrogen.
Putative advantages over conventional DES are early restoration of physiological processes, superior conformability, beneficial edge-vascular response, and suppression of late stent-related complications (i.e., in-stent restenosis and stent thrombosis).
From excitement to uncertainty
The initial reports from single-arm studies in highly selected patients with simple coronary lesions were very reassuring (4). However, an increasing body of evidence from “real-life” registries reported concerning rates of stent thrombosis as high as 3% at 1 year (5-7). Although several randomised-controlled trials have shown equivalent safety and efficiency outcomes at mid-term between BVS and other newer generation DES (8-10), all were of relatively small size and underpowered to assess differences in clinically relevant but rare events such stent thrombosis. To date, 3 meta-analyses have assessed the performance of the device compared to metallic DES (Table 1). There seems to be a definite trend towards higher rates of myocardial infarction and device thrombosis with the use of BVS.
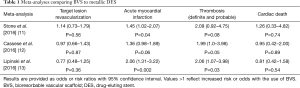
Full table
There are several limitations to the unrestricted use of BVS that may explain these observations. First, accurate sizing is necessary when using the device in order to achieve optimal strut apposition (14). Choosing too small a scaffold diameter results in the need for overstretch dilation. Overstretching the BVS is limited to <1.0 mm above the nominal scaffold diameter. As the largest BVS is 3.5 mm and the maximal post-expansion recommended is 0.5 mm over the nominal diameter, major bifurcations and large vessels (≥4 mm) need best be avoided, including the left main coronary artery. There have been reports of polymer fracture after post-dilatation, triggered by overstretching of the device (15). Furthermore, local overexpansion might induce edge dissection. On the other hand, the use of an inappropriately large BVS results in oversizing and underexpansion, which has been linked to scaffold thrombosis (16). The use of the device in small vessels, particularly in vessels <2.25 mm, may augment the footprint of the device, i.e., the % of the vascular circumference occupied by the relatively thick BVS struts (150 µm) (17). The performance of the device is poor in small vessels and a high footprint has been identified as a predictor for scaffold thrombosis (7).
Secondly, the polymer platform is not as strong and has less radial strength than metallic stents (18), which is an issue in highly calcific lesions. As bioresorption progresses, radial strength further declines harbouring the risk for scaffold collapse.
The duration of dual antiplatelet therapy (DAPT) after BVS is an unresolved, important issue. Extended and efficient DAPT is indeed indicated. DAPT interruption results in high rates of scaffold thrombosis. In the acute phase after BVS placement, inflammation and the formation of micro-thrombi can be observed by histopathological examination (19). As time advances, struts are covered—a phenomenon, which can be visualised by optical coherence tomography (OCT) and is referred to as ‘capping’. In metallic stents this ‘capping’ represents vascular healing and the visualized tissue is mainly composed of neointima. It might be that ‘capping’ of BVS-struts does not represent vascular healing but rather a correlate of thrombin apposition. The micro-thrombi visualized in the acute phase eventually grow and evolve into chronic organized thrombi visible on OCT imaging and undistinguishable from neointima. This mechanism possibly explains the deleterious effects of insufficient DAPT prescription, whether in efficacy or in duration.
The rate of thombosis has also been higher for BVS-treated ostial lesions compared to metallic stents where the abrasion of the catheter is thought to provoke more BVS strut distorsion (20). Another concern is the risk of side-branch occlusion, again, due to the bulky device with a higher scaffold to artery ratio (21). Interestingly, when the above issues are known and anticipated, a dedicated protocol for BVS implantation seems to be efficient in reducing the risk of thrombosis (7). Ultimately, and according to evidence gathered in the late 1960s by Charles Dotter, it is no surprise that contrary to the initial belief, BVS are not devoid of device thrombosis (22).
It is likely that, much like first-generation DES, the technical and bio-chemical limitations of first-generation BVS will be overcome. A new treatment standard for coronary artery disease (CAD) could be set if the industry manages to increase stretchability while creating stronger yet thinner backbones with less biodegradation-related inflammation. Several BVS devices are currently being tested clinically and many trials are ongoing, some of which will include patients with acute coronary syndrome (ACS) (4).
BVS in ST-elevated myocardial infarction
Percutaneous coronary intervention with a reperfusion strategy and stenting are all class I recommendations for the treatment of ST-elevation myocardial infarction (STEMI) (23). There is a of course a strong incentive to demonstrate clinical efficiency and safety of BVS in those who have the strongest indication for percutaneous coronary intervention.
And although BVS may have some limitations, their use in STEMI patients is particularly appealing. The lesions are indeed more often focal and less calcified. Moreover, patients tend to be younger than NSTEMI and other CAD-patients, and the advantages of BVS, such as a restoration of vasomotion or late lumen enlargement would be of greatest benefit on the long-term. However, STEMI-patients are also a high-risk patient subset, which present with higher rates of adverse events than patients with stable CAD.
The first reports of BVS-treated STEMI patients
The first reports of short to mid-term clinical outcome in BVS-treated STEMI patients were rather encouraging. However, the data stemmed from single-arm or unadjusted comparative studies (Table 2). Device related adverse events as defined by the academic research consortium ranged from 0% to 9.1% in the 192 reported patients.
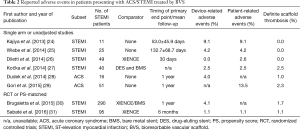
Full table
The BVS-EXAMINATION Study
Brugaletta et al. made an important contribution to our understanding of the application of BVS in STEMI patients by reporting the outcomes of 290 consecutive patients treated at 6 institutions across the globe (30). The study was published in the January issue of the JACC Cardiovascular Interventions in 2015. The BVS-treated patients were compared to 290 propensity score (PS) matched everolimus-eluting stents (EES) and 290 PS matched BMS treated patients enrolled in the EXAMINATION Trial. The investigators assessed the occurrence of device-oriented adverse events, as well as stent or scaffold thrombosis at 1 month and 1 year. There were no significant differences in individual end points but they observed a numerically higher rate of early definite scaffold/stent thrombosis in the BVS group.
The information provided on short and mid-term outcome in BVS treated STEMI patients is of utmost clinical relevance and raises the question whether the unrestricted use of the device in a subgroup with an increased baseline risk for stent thrombosis is reasonable. Indeed, owing to the novelty of the technique and the distinct physical properties of the device, treatment of STEMI patients may be accompanied by unforeseen complications. Even though not statistically significant, the numerically higher rate of early stent thrombosis is concerning and likely the result of an implantation technique that was not tailored to the decreased radial strength, the increased acute recoil, and the need for optimal lesion preparation to avoid mechanistic complications such as underexpansion or incomplete stent apposition. Relevant information on target lesion revascularization and target-vessel related MI rates suggested an acceptable hazard with BVS. However, the patient sample was relatively small and the data was observational in nature with residual differences in baseline characteristics between treatment arms.
The ABSORB-stemi TROFI II trial
Sabaté et al. made another important contribution by publishing the primary outcome of the multicentric, randomised, single-blinded TROFI II trial (31). They reported BVS to be non-inferior to EES in STEMI patients at six months for arterial healing based on a multimodal imaging score. Clinical outcomes were not different between the treatment groups. Clinical follow-up is still on-going and will explore the mid- and long-term outcomes. It is important to point out, however, that patients with cardiogenic shock and significant vessel tortuosity or calcifications were not included in this trial.
Conclusions
Is BVS better than the other DES in our cathlabs? No, and the evidence shows that it is, at best and for specific patients and lesions, non-inferior with a trend toward being inferior. The evidence for BVS implantation in STEMI patients is very limited. While it appears to be safe in the hands of experienced operators who are well aware of the technical limitations, the ABSORB BVS does show a trend towards a higher rate of myocardial infarction compared to other metallic DES. The major safety concerns from the initial European experience have led to more careful lesion selection and preparation thus reducing the risk of stent thrombosis. Is ABSORB BVS a step toward a paradigm shift? Maybe.
There is no convincing evidence that the hypothetical advantages of BVS are or will be of any benefit to patients. More definitive evidence will only be available in about 5 to 7 years. Until then, the “optimistic” will continue to use it and the “sceptic” will wait. In March 2016, the advisory panel of the Food and Drug Administration has given near-unanimous support for approval of the ABSORB BVS, while its use has drastically decreased in Europe. One can only hope that the fruit will continue to ripen, and for our patients to benefit from further technological enhancements.
Acknowledgements
None.
Footnote
Provenance: This is an invited Perspective commissioned by the Section Editor Yue Liu (Associate professor, Department of Cardiology, The First Affiliated Hospital of Harbin Medical University, Harbin, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Grüntzig AR, Senning A, Siegenthaler WE. Nonoperative dilatation of coronary-artery stenosis: percutaneous transluminal coronary angioplasty. N Engl J Med 1979;301:61-8. [Crossref] [PubMed]
- Sigwart U, Puel J, Mirkovitch V, et al. Intravascular stents to prevent occlusion and restenosis after transluminal angioplasty. N Engl J Med 1987;316:701-6. [Crossref] [PubMed]
- Puricel S, Kallinikou Z, Espinola J, et al. Comparison of endothelium-dependent and -independent vasomotor response after abluminal biodegradable polymer biolimus-eluting stent and persistent polymer everolimus-eluting stent implantation (COMPARE-IT). Int J Cardiol 2016;202:525-31. [Crossref] [PubMed]
- Iqbal J, Onuma Y, Ormiston J, et al. Bioresorbable scaffolds: rationale, current status, challenges, and future. Eur Heart J 2014;35:765-76. [Crossref] [PubMed]
- Capodanno D, Gori T, Nef H, et al. Percutaneous coronary intervention with everolimus-eluting bioresorbable vascular scaffolds in routine clinical practice: early and midterm outcomes from the European multicentre GHOST-EU registry. EuroIntervention 2015;10:1144-53. [Crossref] [PubMed]
- Kraak RP, Hassell ME, Grundeken MJ, et al. Initial experience and clinical evaluation of the Absorb bioresorbable vascular scaffold (BVS) in real-world practice: the AMC Single Centre Real World PCI Registry. EuroIntervention 2015;10:1160-8. [Crossref] [PubMed]
- Puricel S, Cuculi F, Weissner M, et al. Bioresorbable Coronary Scaffold Thrombosis: Multicenter Comprehensive Analysis of Clinical Presentation, Mechanisms, and Predictors. J Am Coll Cardiol 2016;67:921-31. [Crossref] [PubMed]
- Ellis SG, Kereiakes DJ, Metzger DC, et al. Everolimus-Eluting Bioresorbable Scaffolds for Coronary Artery Disease. N Engl J Med 2015;373:1905-15. [Crossref] [PubMed]
- Serruys PW, Chevalier B, Dudek D, et al. A bioresorbable everolimus-eluting scaffold versus a metallic everolimus-eluting stent for ischaemic heart disease caused by de-novo native coronary artery lesions (ABSORB II): an interim 1-year analysis of clinical and procedural secondary outcomes from a randomised controlled trial. Lancet 2015;385:43-54. [Crossref] [PubMed]
- Puricel S, Arroyo D, Corpataux N, et al. Comparison of everolimus- and biolimus-eluting coronary stents with everolimus-eluting bioresorbable vascular scaffolds. J Am Coll Cardiol 2015;65:791-801. [Crossref] [PubMed]
- Stone GW, Gao R, Kimura T, et al. 1-year outcomes with the Absorb bioresorbable scaffold in patients with coronary artery disease: a patient-level, pooled meta-analysis. Lancet 2016;387:1277-89. [Crossref] [PubMed]
- Cassese S, Byrne RA, Ndrepepa G, et al. Everolimus-eluting bioresorbable vascular scaffolds versus everolimus-eluting metallic stents: a meta-analysis of randomised controlled trials. Lancet 2016;387:537-44. [Crossref] [PubMed]
- Lipinski MJ, Escarcega RO, Baker NC, et al. Scaffold Thrombosis After Percutaneous Coronary Intervention With ABSORB Bioresorbable Vascular Scaffold: A Systematic Review and Meta-Analysis. JACC Cardiovasc Interv 2016;9:12-24. [Crossref] [PubMed]
- Foin N, Torii R, Mattesini A, et al. Biodegradable vascular scaffold: is optimal expansion the key to minimising flow disturbances and risk of adverse events? EuroIntervention 2015;10:1139-42. [Crossref] [PubMed]
- Ormiston JA, Webber B, Ubod B, et al. An independent bench comparison of two bioresorbable drug-eluting coronary scaffolds (Absorb and DESolve) with a durable metallic drug-eluting stent (ML8/Xpedition). EuroIntervention 2015;11:60-7. [Crossref] [PubMed]
- Cuculi F, Puricel S, Jamshidi P, et al. Optical Coherence Tomography Findings in Bioresorbable Vascular Scaffolds Thrombosis. Circ Cardiovasc Interv 2015;8:e002518. [PubMed]
- Kereiakes DJ. New Randomized Trial Data (1-Year Outcomes): ABSORB III (TCT Late-Breaking Clinical Trial Results and Beyond). Transcatheter Cardiovascular Therapeutics 2015. Available online: http://www.tctmd.com/show.aspx?id=398&ref_id=132165
- Onuma Y, Serruys PW. Bioresorbable scaffold: the advent of a new era in percutaneous coronary and peripheral revascularization? Circulation 2011;123:779-97. [Crossref] [PubMed]
- Joner M. Rationale for BRS in Vulnerable Plaque. Transcatheter Cardiovascular Therapeutics 2014. Available online: http://www.tctmd.com/show.aspx?id=124932
- Cassese S, Kastrati A. Bioresorbable Vascular Scaffold Technology Benefits From Healthy Skepticism. J Am Coll Cardiol 2016;67:932-5. [Crossref] [PubMed]
- Muramatsu T, Onuma Y, García-García HM, et al. Incidence and short-term clinical outcomes of small side branch occlusion after implantation of an everolimus-eluting bioresorbable vascular scaffold: an interim report of 435 patients in the ABSORB-EXTEND single-arm trial in comparison with an everolimus-eluting metallic stent in the SPIRIT first and II trials. JACC Cardiovasc Interv 2013;6:247-57. [Crossref] [PubMed]
- Dotter CT. Transluminally-placed coilspring endarterial tube grafts. Long-term patency in canine popliteal artery. Invest Radiol 1969;4:329-32. [Crossref] [PubMed]
- Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg PG, James SK, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012;33:2569-619.
- Kajiya T, Liang M, Sharma RK, et al. Everolimus-eluting bioresorbable vascular scaffold (BVS) implantation in patients with ST-segment elevation myocardial infarction (STEMI). EuroIntervention 2013;9:501-4. [Crossref] [PubMed]
- Wiebe J, Möllmann H, Most A, et al. Short-term outcome of patients with ST-segment elevation myocardial infarction (STEMI) treated with an everolimus-eluting bioresorbable vascular scaffold. Clin Res Cardiol 2014;103:141-8. [Crossref] [PubMed]
- Diletti R, Karanasos A, Muramatsu T, et al. Everolimus-eluting bioresorbable vascular scaffolds for treatment of patients presenting with ST-segment elevation myocardial infarction: BVS STEMI first study. Eur Heart J 2014;35:777-86. [Crossref] [PubMed]
- Kočka V, Malý M, Toušek P, et al. Bioresorbable vascular scaffolds in acute ST-segment elevation myocardial infarction: a prospective multicentre study 'Prague 19'. Eur Heart J 2014;35:787-94. [Crossref] [PubMed]
- Dudek D, Rzeszutko Ł, Zasada W, et al. Bioresorbable vascular scaffolds in patients with acute coronary syndromes: the POLAR ACS study. Pol Arch Med Wewn 2014;124:669-77. [PubMed]
- Gori T, Schulz E, Hink U, et al. Clinical, Angiographic, Functional, and Imaging Outcomes 12 Months After Implantation of Drug-Eluting Bioresorbable Vascular Scaffolds in Acute Coronary Syndromes. JACC Cardiovasc Interv 2015;8:770-7. [Crossref] [PubMed]
- Brugaletta S, Gori T, Low AF, et al. Absorb bioresorbable vascular scaffold versus everolimus-eluting metallic stent in ST-segment elevation myocardial infarction: 1-year results of a propensity score matching comparison: the BVS-EXAMINATION Study (bioresorbable vascular scaffold-a clinical evaluation of everolimus eluting coronary stents in the treatment of patients with ST-segment elevation myocardial infarction). JACC Cardiovasc Interv 2015;8:189-97. [Crossref] [PubMed]
- Sabaté M, Windecker S, Iñiguez A, et al. Everolimus-eluting bioresorbable stent vs. durable polymer everolimus-eluting metallic stent in patients with ST-segment elevation myocardial infarction: results of the randomized ABSORB ST-segment elevation myocardial infarction-TROFI II trial. Eur Heart J 2016;37:229-40. [Crossref] [PubMed]


