Dimethylacetamide-induced occupational toxic hepatitis with a short term recurrence: a rare case report
Introduction
DMAc (CAS NO. 127-19-5) is one of the important organic solvents in chemical industry (1). In China, it is mainly used in the wet process of acrylic fiber production, especially during spandex spinning (2). It could also be applied for extracting butadiene from ethylene pyrolysis gas as well as the production of polyimide film (3). Reportedly, DMAc could be inhaled or absorbed through the skin leading to occupational damage with liver as the mainly susceptible organ (4,5). Here, we report a case of hepatotoxicity due to DMAc exposure, who recovered after treatment but relapsed as soon as coming back to work.
Case presentation
The patient was a 42-year-old man who had been working as a shift leader and operator in a polyimide film factory. It was approximately 6 months exposing to DMAc before he visited the hospital. He complained of no specific medical history or familial or genetic problems, no smoking and rarely consumed alcohol. His pre-job medical examination showed a normal hepatic function.
Fifteen days prior to his admission to hospital, he developed vague abdominal pain in a paroxysmal manner, as well as xanthochromia. Physical examination results were as follows: clear mind, poor spirit, moderate to severe jaundice of sclera and skin, mild abdominal tenderness; the size of liver and spleen was normal.
His laboratory data on admission were as shown below: white blood cell count, 6,000/mm3; hemoglobin, 156 g/L; platelet count, 227,000/mm3, aspartate aminotransferase (AST), 415 IU/L; alanine aminotransferase (ALT), 474 IU/L; γ-glutamyl transpeptidase (γ-GT), 173 IU/L; albumin, 43.1 g/L; total bilirubin (TBIL), 226.4 µmol/L; direct bilirubin (DBIL), 169.0 µmol/L; potassium, 1.61 mmol/L; sodium, 50.3 mmol/L; chloride, 33.1 mmol/L; total bile acid (TBA), 153.6 µmol/L; urinary leukocyte, 196.1/µL; alpha-fetoprotein (AFP), 378.3 ng/mL. Serologic testings for hepatitis (A, B, C, D and E), cytomegalovirus, Epstein-Barr virus, herpes simplex, and varicella zoster were all negative. Tests for antinuclear antibodies and anti-smooth muscle antibodies were also negative. Ultrasound and CT inspection of the abdomen was unremarkable. In summary, this case was tentatively diagnosed as DMAc-induced acute toxic hepatitis.
After admittance, he was treated with stomachic and hepatoprotective agents along with conservative management. His symptoms subsequently lessened, and AST/ALT level stabilized. On hospital day 4, AST/ALT declined to 59/112 IU/L; γ-GT, 90 IU/L; TBIL, 194.1 µmol/L;DBIL, 161.8 µmol/L; urinary leukocyte 108.7/µL. Seven days after hospitalization, there was no tenderness or discomfort in his right upper quadrant of the abdomen, no jaundice with nausea, vomiting, loss of appetite either. No notable findings were present upon examination of the other systems. The predominant laboratory findings were as below: AST, 30 IU/L; ALT, 36 IU/L; γ-GT, 86 IU/L.
He was discharged to work after remission of liver function. However, during the next 3 days, the patient developed progressive scleral jaundice with anepithymia. His hepatic function worsened as the laboratory data revealed AST, 166.5 IU/L; ALT, 137.5 IU/L; TBIL, 106.7 µmol/L; DBIL, 83.8 µmol/L; AFP 711.4 ng/mL. Then he was taught to recuperate at home with medical advice. After stopping work, his liver enzymes gradually returned to normalcy. On Out Patient Department follow up, his AST/ALT value subsequently declined to 88/104 and 35/22.5 IU/L 6 days and 2 months later, respectively. Complete laboratory examination was performed again 3 months afterward, indicating AST, 29 IU/L; ALT, 29 IU/L; γ-GT, 86 IU/L; TBIL, 22.7 µmol/L; DBIL, 7.7 µmol/L; AFP, 15.2 ng/mL.
This study was approved by Ethics Committee of Jiangsu Provincial Center for Disease Prevention and Control. And the ID of the approval was SL2014-B019-02. Written informed consent was obtained and recorded. In the preparation of this article, all efforts were made to protect patient privacy and anonymity.
Workplace inspection
Production process
4,4-diaminodiphenyl and pyromellitic anhydride were employed as raw materials, with DMAc as the solvent. After combining them to synthetize polyamide acid, defoaming and stretching process were involved to generate the end-products. The production equipments mainly included reactor, vacuum degassing vessel, filter, hopper, casting and winding machines, along with hot air systems.
Occupational history
Before moving to this factory, the patient was a 12-years’ professional fitter with no history of exposure to any chemicals. As a shift leader and operator of current plant who worked fixed 12-hours schedules in two shifts, his daily task consisted of routing inspection on equipments and production process, solvent extraction and recovery as well as reactor operation at resin synthesis area, during which time he could be directly exposed to DMAc. Though the workshop was equipped with a local ventilation system, the employees reflected it didn’t run smoothly all day long. A distinct pungent odor was found when we carried out the field investigation. Long-sleeved coveralls and gauze masks were normatively provided to the workers.
Field test data
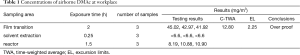
The regular monitor of occupational hazards was not normally put into effect. We carried on an on-site detection in order to meet the diagnosis criteria of corresponding occupational disease. As a result, the 8 hours time-weighted average (C-TWA) measurement of DMAc air concentration in his worksite was 12.8 mg/m3 lower than that of the national occupational health standard (PC-TWA: 20 mg/m3, China GBZ 2.1-2007). However, the 15 minutes short-term exposure concentrations at the inspection site of film transition, solvent extraction area and the reactor were 45.0, <6.6 and 10.90 mg/m3, respectively, giving rise to a maximum excursion limits (EL) of 2.25 which was beyond the airborne standard of 2 (China GBZ 2.1-2007, Table 1).
Full table
Health condition of the workmates
Other six workers in similar worksite were arranged for a medical examination. It turned out that abnormal hepatic function was observed in 2 female workers without rational symptoms. They admitted no contacting with other chemicals before and the pre-employment medical reports showed nothing special about their physical status. One of them got in touch with DMAc for 6 months, revealing ALT 350.4 IU/L, ketone 2+, proteinuria +/−, and occult blood 1+; The other exposed to DMAc for 3 months got a laboratory index of ALT 115.6 IU/L. They followed the doctor’s advice to discontinue working and rest at home, resulting in a restored liver function after 1 month.
Diagnosis
Based on the occupational toxic liver disease diagnostic criteria (China GBZ 59-2010), the case was made a definite diagnosis as occupational acute toxic hepatitis induced by DMAc.
Discussion
DMAc and DMF (CAS NO. 68-12-2) are family members of acetamide and formamide methyl derivatives. Reportedly, DMF was tightly associated with abnormal liver function, even in workers exposed below the 10 ppm threshold (3,6). As a substitute for more toxic DMF, DMAc have been widely used in recent years. Despite occupational exposure limits (OELs) and industrial hygiene practices as restrictions, DMAc has been inevitably related to occupational illness, especially in Asia where new and expanded uses have led to overexposures (7,8). Significantly, it is worth noting that DMAc-induced hepatic injury (DIHI) may still occur below OEL if there are dermal exposures (9,10). Jung et al. identified 38 DIHI cases between 2001 and 2004 in two spandex factories. The interval between first exposure and identification of DIHI was mostly less than two months and never exceeded 6 months. In addition, three repeat DIHI cases showed much shorter latent periods for recurrence than their initial latent periods of hepatic injury (11). This conclusion was in line with our observations elucidated above.
To confirm a diagnosis of chemical induced toxic hepatitis, other forms of hepatitis and other disorders with similar symptoms should be ruled out. The diagnostic criteria are as follows: occupational exposure preceding liver damage; liver enzymes at least double the upper limit of normal level; and other causes of liver disease excluded (12). In this case reported herein, workplace DMAc exposure preceded the patient’s recognition of symptoms. His liver function indexes increased far beyond the upper limit of the normal range (Figure 1). Other causes of hepatitis were ruled out during the clinical courses.

Notably, the tumor antigen AFP reached as high as 711.4 ng/mL in the early stage of his recurrence, which was far beyond the normal value of 20 ng/mL. Subsequently, it declined to normal range under effective treatments that made the sufferer feel a palpable sense of relief. As is known to all, AFP is frequently measured for diagnosing hepatocellular carcinoma (13). Occasionally, small transient increases in serum AFP is associated with benign hepatic diseases such as acute and chronic viral hepatitis as well as toxic liver injury (14-16). Importantly, we are the first to report the elevation of AFP among DIHI cases.
Diagnostic criteria of occupational toxic hepatopathy (China GBZ 59-2010) has clarified DMAc as a common hepatotoxic agent. Despite many studies suggest that exposure to organic solvents can cause hepatotoxicity, occupational organic solvent exposure-induced hepatotoxicity is rarely diagnosed or even suspected (17-19). And it is virtually impossible to completely control chronic liver damage among workers because of nonspecific symptoms and signs as well as the low sensitivity of conventional liver enzyme tests. Therefore, it is important to focus on individual cases. In particular, we can learn a lesson that DIHI might recur with a latent period much shorter than the initial stage. The workers for whom there is a significant suspicion of DIHI should be eliminated from further exposure. Furthermore, DIHI should be considered as a relative contraindication for the workers who have to contact with DMAc.
Acknowledgements
We would like to thank Ellen Galloway and Gregory A. Burr from NIOSH of CDC for their generous help with our draft writing.
Funding: This work was supported by Jiangsu Province’s Outstanding Medical Academic Leader program (LJ201130).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying data.
References
- Kennedy GL. Toxicology of dimethyl and monomethyl derivatives of acetamide and formamide: a second update. Crit Rev Toxicol 2012;42:793-826. [Crossref] [PubMed]
- Qian YL, Xu CM, Lu YY, et al. Biological limit value for occupational exposure to N, N-dimethylacetamide Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2012;30:709-11. [PubMed]
- Cheng J, Liu Q, Xu B, et al. Effect of N, N-dimethylformamide on oxidation or antioxidation status among occupational exposed workers. Zhonghua Yu Fang Yi Xue Za Zhi 2014;48:28-32. [PubMed]
- Kennedy GL Jr, Sherman H. Acute and subchronic toxicity of dimethylformamide and dimethylacetamide following various routes of administration. Drug Chem Toxicol 1986;9:147-70. [Crossref] [PubMed]
- Kim SN. Preclinical toxicology and pharmacology of dimethylacetamide, with clinical notes. Drug Metab Rev 1988;19:345-68. [Crossref] [PubMed]
- Twiner MJ, Hirst M, Valenciano A, et al. N,N-Dimethylformamide modulates acid extrusion from murine hepatoma cells. Toxicol Appl Pharmacol 1998;153:143-51. [Crossref] [PubMed]
- Lee CY, Jung SJ, Kim SA, et al. Incidence of dimethylacetamide induced hepatic injury among new employees in a cohort of elastane fibre workers. Occup Environ Med 2006;63:688-93. [Crossref] [PubMed]
- Kim HR, Kim TW. Occupational hepatic disorders in Korea. J Korean Med Sci 2010;25:S36-40. [Crossref] [PubMed]
- Baum SL, Suruda AJ. Toxic Hepatitis from Dimethylacetamide. Int J Occup Environ Health 1997;3:1-4. [Crossref] [PubMed]
- Finlay C, Malley LA, Kennedy GL Jr. Absorption of dimethylacetamide (DMAC) following application of a polymer film to the skin of rabbits. Appl Occup Environ Hyg 2001;16:1103-5. [Crossref] [PubMed]
- Jung SJ, Lee CY, Kim SA, et al. Dimethylacetamide-induced hepatic injuries among spandex fibre workers. Clin Toxicol (Phila) 2007;45:435-9. [Crossref] [PubMed]
- Maria VA, Victorino RM. Development and validation of a clinical scale for the diagnosis of drug-induced hepatitis. Hepatology 1997;26:664-9. [Crossref] [PubMed]
- Wu CS, Lee TY, Chou RH, et al. Development of a highly sensitive glycan microarray for quantifying AFP-L3 for early prediction of hepatitis B virus-related hepatocellular carcinoma. PLoS One 2014;9:e99959. [Crossref] [PubMed]
- Kreczko S, Lipska A, Wysocka J. Alpha-fetoprotein: diagnostic value in hepatic disorders. Pol Merkur Lekarski 2000;8:420-3. [PubMed]
- Seo SI, Kim SS, Choi BY, et al. Clinical significance of elevated serum alpha-fetoprotein (AFP) level in acute viral hepatitis A (AHA). Hepatogastroenterology 2013;60:1592-6. [PubMed]
- Wang L, Huang J, Jiang M, et al. AFP computational secreted network construction and analysis between human hepatocellular carcinoma (HCC) and no-tumor hepatitis/cirrhotic liver tissues. Tumour Biol 2010;31:417-25. [Crossref] [PubMed]
- Franco G, Fonte R, Candura F. Hepatotoxicity of organic solvents. Br J Ind Med 1986;43:139. [PubMed]
- Døssing M. Occupational toxic liver damage. J Hepatol 1986;3:131-5. [Crossref] [PubMed]
- Ito D, Tanaka T, Akamatsu N, et al. Recurrent Acute Liver Failure Because of Acute Hepatitis Induced by Organic Solvents: A Case Report. Medicine (Baltimore) 2016;95:e2445. [Crossref] [PubMed]


