Abnormal bone mineral density and bone turnover marker expression profiles in patients with primary spontaneous pneumothorax
Introduction
A pneumothorax is air within the pleural space. Clinically, pneumothorax is often categorized as either spontaneous pneumothorax or traumatic pneumothorax. Spontaneous pneumothorax can be further divided into primary spontaneous pneumothorax (PSP) and secondary spontaneous pneumothorax. PSP typically refers to pneumothorax seen in populations without previous underlying lung diseases.
As a clinically common benign lung disease, PSP has an incidence of 18–28/100,000 in males and 1.2–6/100,000 in females. The incidence can be particularly high in smokers. Although many clinical centers and international guidelines have described the management of PSP (including prevention of its relapse) in the past decades (1-3), the pathogenesis of PSP remains unclear and controversial.
It is widely believed that adolescents and young adults aged 20–30 years old are more susceptible to PSP; thin individuals with a low basal metabolic index are also at higher risk. In the 11–14 age group, PSP patients are significantly taller than healthy individuals (4). Many studies have found that chest height is remarkably higher in adolescent PSP patients than in populations of the same age (5). Rapid height and chest height growth is much earlier in PSP patients than in normal populations, and may quickly stabilize at 14–16 years of age. This rapid growth in adolescents may be a risk factor for PSP.
Development of the spine and supporting bones of the lower limbs is directly related with height and chest height. The growth of the spine directly determines height and indirectly affects chest height. However, whether rapid height and chest height growth also play a role in bone turnover (including bone formation and resorption) of the spine or other bones remains unclear.
We hypothesized that there were significant differences in bone metabolism status between PSP patients or without PSP, and possible risk factors included the height, weight, body mass index, and the levels of vitamin D. We explored this hypothesis by measuring bone mineral density and circulating bone biomarkers, including bone formation marker procollagen type I aminoterminal propeptide (PINP) and N-terminal midmolecule fragment osteocalcin (N-MID), bone resorption marker b-C-telopeptides of type I collagen (b-CTX) and tartrate-resistant acid phosphatase 5b (TRACP5b) in young patients aged 12 to 30 years with PSP and healthy individuals of the same ages. Also, we collected clinical data for statistical analysis, and analyzed the factors that contributed to the onset of the PSP and the change in bone metabolism.
Methods
Study subjects
From September 2013 to August 2015, 83 consecutive patients with sporadic PSP who were admitted to the Department of Thoracic Surgery, Beijing Chaoyang Hospital (Beijing, China), defined by spontaneous air accumulation in the thoracic cavity without evidence of clinical lung disease, were enrolled in the study. The inclusion criteria were: (I) conform to the diagnostic criteria of primary spontaneous pneumothorax, pneumothorax noted by chest radiography; (II) patient age between 11 and 30 years. The exclusion criteria were: (I) a history of lung diseases such as COPD, pulmonary tuberculosis and infection; (II) a history of chest trauma, such as rib fracture and pulmonary contusion; (III) unable to determine the presence of secondary factors, or a set of data not congruent effect into the standard to judge; (IV) had undergone any therapy affecting bone metabolism for more than two weeks in the three months directly preceding the study, including therapy of bisphosphonates, estrogen, androgen-stimulating, parathyroid hormone, calcitonin or progestin; (V) had a history of metabolic bone disease. Meanwhile, 87 healthy individuals who received health check-ups at the Center of Health Examination, Beijing Chao-Yang Hospital (Beijing, China), and were confirmed to be free of lung disease by medical imaging were included as control group. The inclusion criteria were as follow: (I) conform to be free of lung disease by medical imaging; (II) patient age between 11 and 30 years. The exclusion criteria were the same as above, such as: (I) a history of lung diseases; (II) a history of chest trauma; (III) unable to determine the presence of secondary factors, or a set of data not congruent effect into the standard to judge; (IV) had undergone any therapy affecting bone metabolism for more than two weeks in the three months directly preceding the study; (V) had a history of metabolic bone disease. Given that age is an influential factor for bone metabolism and bone density, age-matched healthy individuals (11–30 years old) were used. The study protocol and consent procedure were approved by the ethics committee of Beijing Chao-Yang Hospital (ethics number: 2015-151).
Study design
Clinical data
This included age, gender, height, body weight, body mass index (BMI) and whether there was a history of familial pulmonary disease. BMI, height, and weight were measured barefoot and in lightweight indoor clothing and the BMI was calculated.
Dual-energy X-ray absorptiometry
Bone mineral density (BMD) of the head, chest, lumbar vertebrae 1–4 (L1–4), left femur neck, Ward’s triangle, greater trochanter, and left proximal part of the femur were determined by dual-energy X-ray absorptiometry.
Bone metabolism biomarkers and biochemistry assays
Fasting venous blood samples were collected from each participant between 8:00 and 9:00 AM. Participants were asked to avoid strenuous exercise in the preceding 24 hours and to fast overnight. Collected specimens were transferred to serum separation tubes (BD, Franklin Lakes, NJ, USA). Blood samples were placed at room temperature for 30 min to coagulate, and then centrifuged at 2,500 ×g for 10 min to separate serum, which was stored at −70 °C. Frozen serum specimens were stored in the laboratory at the Clinical Research Center of Beijing Institute of Respiratory Diseases. Unified detection of serum levels of b-CTX, PINP, N-MID and 25-OH VD was conducted in the Clinical Laboratory, Beijing Chao-Yang Hospital (Beijing, China) using a computer-controlled automatic analyzer for chemiluminescence workstation with Elecsys reagent kits supplied by Roche Diagnostics (Basel, Switzerland). The serum TRACP5b level was measured by ELISA using a TRACP5b assay kit (Immunodiagnostic Systems, IDS, UK).
Statistical analysis
Data analysis was performed using the Statistical Package for the Social Sciences (SPSS, Chicago, IL, USA), version 20.0. Quantitative parameters were expressed as means ± standard deviation (SD), median, and 95% confidence interval, while qualitative variables were described as numbers and percentage values. Distributions were described by scatter plot. Analyses included independent t-test, Chi-square test and Mann-Whitney U test. Pearson’s correlation analysis was used for evaluating associations between bone formation markers, bone resorption marker and 25OH VD levels. Risk factors for PSP were analyzed using logistic regression analysis. A P value of <0.05 was considered statistically significant.
Results
Participants’ characteristics
A total of 83 PSP patients were included in the PSP group and 87 healthy participants in the control group. In the PSP group, there were 62 males (75%) and 21 females (25%), with a median age of 19 years (17.0, 25.0). In the control group, there were 46 males (53%) and 41 females (47%), with a median age of 21 years (19.0, 25.0). The age composition showed no significant difference between these two groups (P=0.053).
There were 21 cases of smoking patients (25.3%) in the PSP group and 10 cases of smokers (11.5%) in the control group. Smoking rate of the PSP group was significantly higher than that of control group (P=0.020).
Mean height of the PSP group was significantly greater than that of the control group (174.25±7.41 vs. 167.20±10.69 cm, respectively; P<0.05); whereas weight and BMI were significantly lower (58.30±9.38 vs. 63.16±13.57 kg, respectively; and 19.15±2.45 vs. 22.15±3.82, respectively; both P<0.05).
Bone mineral density and serum bone metabolism markers
BMD measurements were taken from 31 patients in the PSP group and 31 participants in the control group. The PSP group had significantly lower mean BMD than the control group (1.01±0.13 vs. 1.08±0.10 g/cm2, respectively; P=0.015). Of the 31 PSP patients who had BMD measurements, 26 (83.9%) also underwent T-score collection (data were absent for the remaining five patients). According to WHO Criteria for Diagnosis of Osteoporosis (which is based on dual-energy X-ray absorptiometry findings), 12 patients had osteopenia or osteoporosis (12/26, 46.2%), among whom 11 patients had osteopenia (11/12, 91.7%) and one patient had osteoporosis (1/12, 8.3%).
The serum bone metabolism markers, including PINP, N-MID, b-CTX, and TRACP5b, were overexpressed in the PSP group. Forty patients from the PSP group and 40 participants from the control group received bone turnover marker measurements. Expression of the bone formation marker PINP was significantly higher in the PSP group [in which data were obtained from only 36 patients (90.0)] compared with the control group (P=0.012). Expression of the bone resorption markers β-CTX and TRACP5b were also significantly higher in the PSP group (P<0.05). Expression of bone turnover marker N-MID was significantly higher in the PSP group compared with the control group (P<0.05).
The difference in 25-OH VD was statistically significant between the PSP group and the control group. Detection of 25-OH VD in 40 patients from the PSP group and 40 participants from the control group showed that the PSP group had significantly lower expression of 25-OH VD compared with the control group (P<0.05) (see Table 1).
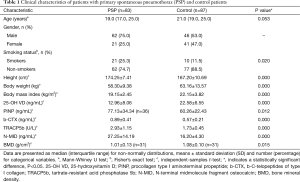
Full table
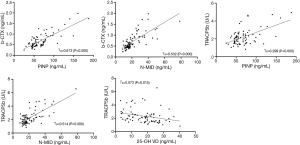
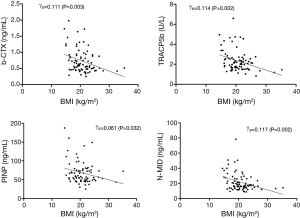
Pearson’s correlation analysis revealed significant positive correlation between PINP, N-MID and b-CTX, TRACP5b levels in the whole study population, respectively. A simple linear equation was fitted, indicating the close coupling relationship between bone resorption and bone formation. PINP, N-MID and b-CTX levels had no correlations with 25-OH VD but TRACP5b negatively correlated with 25-OH VD, though correlation coefficients were relatively low (r=−0.27, P=0.015) (Figure 1). Also, all the bone metabolism marker levels (PINP, N-MID, b-CTX, and TRACP5b) negatively correlated with BMI, with low correlation coefficients(r=−0.247, −0.342, −0.333 and −0.338, respectively) (Figure 2).
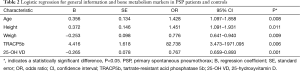
Logistic analysis showed that PSP correlated with five risk factors, including age, height, weight, TRACP5b, and 25-OH VD; among which age, height, and TRACP5b positively correlated with PSP, whereas weight and 25-OH VD negatively correlated with this condition (see Table 2).
Full table
Discussion
PSP is a common clinical emergency that is generally believed to be caused by the rupture of subpleural pulmonary bullae. Emphysema-like changes have been found in over 80% of PSP patients who have received chest scans or in more than 79% of patients who have received surgical treatment (6). Although it remains controversial whether the presence of emphysema-like changes or its severity is directly related with the recurrence of pneumothorax, it has been widely recognized that there is a direct relationship with the onset of pneumothorax (7-11). According to the theory of pleural porosity, mesothelial cells of the visceral pleura at the lesion site will be replaced by a layer of inflammatory elastic fibers, which increase pleural pores; and air leaks can occur when intra-alveolar pressure increases, thus leading to pneumothorax. This may also explain why pneumothorax patients who have undergone pulmonary bulla resection alone still have a relapse rate of up to 20% (12-14).
Inflammatory responses and oxidative stress are also thought to be involved in the pathogenesis of PSP. Overexpression of some inflammatory mediators and oxidative stress factors has been found in serum and lung tissues of PSP patients (15-18). Smoking, environmental factors and psychological/mental status have also been found to be associated with the pathogenesis of PSP (19-23).
In our previous study, we detected the whole-body BMD of 26 adolescents and young adults with PSP and 31 age-matched healthy participants and found that mean BMD was remarkably lower in PSP patients compared with normal individuals, suggesting that osteopenia and osteoporosis might exist in young Chinese PSP patients.
In our current study, we collected general data and measured BMD and relevant bone turnover markers in 83 PSP patients and 87 healthy controls, and explored possible relationships. Since the human body grows and develops rapidly during adolescence, we screened age compositions in these two groups to rule out the influence of age on BMD and bone metabolism; age composition showed no significant difference between these two groups. We found that the male:female ratio was 3:1 in the PSP group, indicating that males were more susceptible to PSP.
As known that smoking status might be potential risk factors for PSP, we conducted a statistical analysis on this between these two groups. Results showed that the smoking rate in PSP group was significantly higher than that of control group. It suggests that smokers are more likely to suffer from PSP, and this conclusion is consistent with previous reports.
The PSP group had significantly increased height and decreased weight and BMI than the control group, findings that are consistent with previous reports. Considering that the PSP group had approximately three fold more male patients than that of control group, and these gender differences would have affected the study results on average height, we splited the data of two groups by gender and compared between the two groups of men and women by subjects of average height, respectively. Results showed that the height difference between the two groups also accord with our conclusion in this paper, namely the average height of men in PSP group is significantly higher than the control group (176.89±6.12 vs. 172.46±6.94 cm, P<0.05), and also to the average height of women in two groups (166.48±5.11 vs. 161.29±11.15 cm, P<0.05). Shows that the height difference in two groups is not due to the different gender ratio and it can eliminate gender ratio factors on the influence of the height.
In addition, mean BMD of adolescents and young adults with PSP was lower than that of the healthy control group at the same ages. Research on T-scores showed that such bone abnormalities mainly manifest as osteopenia, whereas osteoporosis accounts for only 8.3%. Whether populations with PSP accompanied by bone abnormalities are more susceptible to osteoporosis with aging remains unclear.
In addition to PSP, some other lung diseases have been reported to be associated with bone loss and osteoporosis. Mineo et al. (24) carried out preoperative measurements and postoperative follow-up on BMD and bone turnover markers in 40 severe emphysema patients who had received bilateral lung volume reduction surgery and found that BMD and bone alkaline phosphatase levels were significantly different between the study group and the control group (individuals receiving rehabilitation care because of respiratory conditions). Correlation analysis concluded that such changes might be associated with postoperative improvements in respiratory function, which affected metabolism and nutritional status and thus affected bone turnover and mineral levels in the body. In another survey of BMD in patients with airway hyper-responsiveness or asthma, the authors retrospectively analyzed 7,034 patients and found that, after factors such as gender, age, and steroid use were ruled out, BMD of the lumbar vertebrae and femurs was significantly lower in these patients than in normal populations, which might be related with vitamin D (25).
In the current study, we examined possible causes of bone mass abnormality in terms of bone metabolism. Along with research advances in relevant fields, bone turnover markers have been recognized as more accurate indicators of bone metabolism in the earlier stages (compared with BMD). b-CTX and PINP are two markers of bone resorption and bone formation that are recommended by the International Osteoporosis Foundation and the International Federation of Clinical Chemistry and Laboratory Medicine for the diagnosis of osteoporosis. TRACP5b, originating from osteoclasts, is highly specific and its diagnostic efficiency is not affected by circadian rhythm, diet, or liver/kidney diseases; thus, it has become the second-generation biochemical marker of bone resorption. Osteocalcin, also known as bone gamma-carboxyglutamic acid-containing protein, is synthesized and secreted by osteoblasts during the non-proliferation phase. It has been recognized as a specific marker that can reflect osteoblast function. In particular, the molecular fragment N-MID (N-terminal midfragment osteocalcin) in its N-terminal has good stability and sensitivity during detection, and can well reflect changes during bone turnover (26,27).
In the current study, we detected serum bone metabolism markers, including TRACP5b, b-CTX, PINP, and N-MID, and found that the markers of bone resorption and bone formation were present at significantly higher levels in the PSP group compared with the control group. This suggests that PSP patients have varying degrees of bone metabolism disorders, namely enhanced bone resorption and bone formation capabilities, which indirectly reflect the strengthened abilities of osteoclasts and osteoblasts in PSP patients.
Previous studies have reported that TRACP5b and b-CTX could achieve earlier prediction of osteoporosis and showed a negative correlation with BMD (28), which is consistent with our findings. Therefore, increased expression of TRACP5b and b-CTX in PSP patients represents the increased bone absorption capability of osteoclasts. Active osteoclasts secrete acids and enzymes to decompose and absorb the mineralized bone matrix. As a result, the bone mass in this area decreases, leading to osteopenia or osteoporosis, which may explain the abnormal BMD in PSP patients.
Increases in the bone formation marker PINP and bone turnover marker N-MID indicate increased osteoblast activity during bone metabolism in PSP patients. Research has shown that osteoblasts can secrete RANKL and thus activate the MAPK signaling pathway to promote osteoclast differentiation and maturation via the OPG/RANK/RANKL signaling pathway (29), leading to increased osteoclast activation. The OPG/RANK/RANKL system is a recently identified extracellular signal regulation system that regulates differentiation, maturation, and apoptosis of osteoclasts. The OPG/RANK/RANKL system is not only involved in physiological bone reconstruction but also closely associated with pathological bone resorption. The binding of RANKL to receptor activator of nuclear factor-κB (RANK), a receptor located on the osteoclast membrane, is a precondition for osteoclast precursors to further mature and differentiate into functional osteoclasts and exert their bone resorption activity. Osteoprotegerin (OPG), a soluble tumor necrosis factor receptor homolog, can competitively bind RANKL and thus prevent the binding of RANKL and RANK. By doing so, it can inhibit the differentiation and maturation of osteoclasts and reduce bone resorption activity and thus induce apoptosis. During differentiation from bone marrow mesenchymal stem cells into osteoblasts, the OPG/RANKL ratio changes constantly to ensure that bone resorption and bone formation are well balanced. The imbalance of this ratio or the RANK signal, as the common pathological basis of many bone diseases, mainly manifests as excessive bone loss, abnormal bone formation, or disordered bone reconstruction (30). In PSP patients, increased osteoblast activity or metabolic disorders may affect the OPG/RANK/RANKL system, leading to increased osteoclast activity, enhanced bone resorption, and elevated levels of bone resorption markers, which further result in osteopenia. The results of correlation analysis are consistent with this conclusion. Expression levels of bone resorption markers and bone formation markers were found to be upregulated simultaneously and showed certain positive correlations.
In the current study, the 25-OH VD level of the PSP group was significantly lower than that of the control group. The physiological function of vitamin D is to help the body absorb calcium and phosphorus. Thus, vitamin D is necessary for bone formation. Vitamin D deficiency can result in disorders in the absorption of calcium and phosphorus, affect bone formation, and thus cause a series of bone metabolism diseases, such as rickets, osteomalacia, osteoporosis, and osteopenia. Results of the current study support this conclusion. Therefore, a low 25-OH VD level may be another risk factor for decreased BMD in PSP patients.
Regression analysis showed a negative correlation between 25-OH VD and the expression level of TRAP5b, although the value of the correlation coefficient was not high. Relationships with other bone metabolism markers were not statistically significant. Thus, the 25-OH VD level may only have a relationship with bone resorption activities. Furthermore, 25-OH VD deficiency may be not a decisive factor for reduced BMD in PSP patients. In this population, intervention, such as vitamin D supplementation, cannot effectively improve osteopenia. However, this conclusion needs further verification.
We found a negative linear relationship between BMI and bone metabolism markers. Individuals with a low BMI tended to have higher bone resorption and bone formation marker expression profiles, suggesting higher bone resorption/formation activities. Therefore, BMI might be a useful indicator to monitor bone metabolism levels.
For all participants, regression analysis of all indicators showed that age, height, weight, and expression of TRACP5b and 25-OH VD might be risk factors for PSP. Specifically, age, height, and TRACP5b positively correlated with PSP onset; whereas weight and 25-OH VD showed negative correlations. Older individuals who were taller, weighed more, had higher TRACP5b expression, and lower 25-OH VD expression were more susceptible to PSP. These indicators may be useful for screening individuals at high risk of PSP among adolescents and young adults so as to facilitate early diagnosis and early intervention.
We also noted some individuals with osteopenia and bone metabolism disorders in the control group (although the proportion was low). Although these individuals did not experience PSP onset during the study period, whether they will develop PSP in the future remains to be seen. If they are found to show a higher prevalence of PSP during the follow-up period, our current conclusions could be further validated.
As far as we know this study is the first report of correlation between the abnormal bone mineral density and bone turnover marker expression and primary spontaneous pneumothorax, however, it has a limitation in this work. The age and gender did not match exactly between two groups. Although we had made some subgroup analysis as much as possible to minimize the impact of these factors on the basis of existing information, there may still be a bias in the data. A large, prospective study would be warranted to confirm our findings and thus reduce the potential biases observed in this study.
Conclusions
Osteopenia can be seen in PSP patients, along with high expression profiles for the bone resorption and bone formation markers b-CTX, TRAP5b, PINP, and N-MID, and relatively low expression levels of 25-OH VD. Age, height, weight, and TRACP5b and 25-OH VD expression levels can serve as potential indicators of risk factors for PSP.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- MacDuff A, Arnold A, Harvey J, et al. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii18-31. [Crossref] [PubMed]
- Baumann MH, Strange C, Heffner JE, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest 2001;119:590-602. [Crossref] [PubMed]
- De Leyn P, Lismonde M, Ninane V, et al. Guidelines Belgian Society of Pneumology. Guidelines on the management of spontaneous pneumothorax. Acta Chir Belg 2005;105:265-7. [Crossref] [PubMed]
- Fujino S, Inoue S, Tezuka N, et al. Physical development of surgically treated patients with primary spontaneous pneumothorax. Chest 1999;116:899-902. [Crossref] [PubMed]
- Chang PY, Wong KS, Lai JY, et al. Rapid increase in the height and width of the upper chest in adolescents with primary spontaneous pneumothorax. Pediatr Neonatol 2015;56:53-7. [Crossref] [PubMed]
- Müller NL. CT diagnosis of emphysema. It may be accurate, but is it relevant? Chest 1993;103:329-30. [PubMed]
- Martínez-Ramos D, Angel-Yepes V, Escrig-Sos J, et al. Usefulness of computed tomography in determining risk of recurrence after a first episode of primary spontaneous pneumothorax: therapeutic implications. Arch Bronconeumol 2007;43:304-8. [Crossref] [PubMed]
- Ouanes-Besbes L, Golli M, Knani J, et al. Prediction of recurrent spontaneous pneumothorax: CT scan findings versus management features. Respir Med 2007;101:230-6. [Crossref] [PubMed]
- Chou SH, Li HP, Lee JY, et al. Is prophylactic treatment of contralateral blebs in patients with primary spontaneous pneumothorax indicated? J Thorac Cardiovasc Surg 2010;139:1241-5. [Crossref] [PubMed]
- Huang TW, Lee SC, Cheng YL, et al. Contralateral recurrence of primary spontaneous pneumothorax. Chest 2007;132:1146-50. [Crossref] [PubMed]
- Grundy S, Bentley A, Tschopp JM. Primary spontaneous pneumothorax: a diffuse disease of the pleura. Respiration 2012;83:185-9. [Crossref] [PubMed]
- Hatz RA, Kaps MF, Meimarakis G, et al. Long-term results after video-assisted thoracoscopic surgery for first-time and recurrent spontaneous pneumothorax. Ann Thorac Surg 2000;70:253-7. [Crossref] [PubMed]
- Horio H, Nomori H, Kobayashi R, et al. Impact of additional pleurodesis in video-assisted thoracoscopic bullectomy for primary spontaneous pneumothorax. Surg Endosc 2002;16:630-4. [Crossref] [PubMed]
- Noppen M, De Keukeleire T. Pneumothorax. Respiration 2008;76:121-7. [Crossref] [PubMed]
- Chen CK, Chen PR, Huang HC, et al. Overexpression of matrix metalloproteinases in lung tissue of patients with primary spontaneous pneumothorax. Respiration 2014;88:418-25. [Crossref] [PubMed]
- Fang HY, Lin CY, Chow KC, et al. Microarray detection of gene overexpression in primary spontaneous pneumothorax. Exp Lung Res 2010;36:323-30. [Crossref] [PubMed]
- Tabakoglu E, Ciftci S, Hatipoglu ON, et al. Levels of superoxide dismutase and malondialdehyde in primary spontaneous pneumothorax. Mediators Inflamm 2004;13:209-10. [Crossref] [PubMed]
- Goven D, Boutten A, Leçon-Malas V, et al. Induction of heme oxygenase-1, biliverdin reductase and H-ferritin in lung macrophage in smokers with primary spontaneous pneumothorax: role of HIF-1alpha. PLoS One 2010;5:e10886. [Crossref] [PubMed]
- Cheng YL, Huang TW, Lin CK, et al. The impact of smoking in primary spontaneous pneumothorax. J Thorac Cardiovasc Surg 2009;138:192-5. [Crossref] [PubMed]
- Haga T, Kurihara M, Kataoka H, et al. Influence of weather conditions on the onset of primary spontaneous pneumothorax: positive association with decreased atmospheric pressure. Ann Thorac Cardiovasc Surg 2013;19:212-5. [Crossref] [PubMed]
- Noppen M, Verbanck S, Harvey J, et al. Music: a new cause of primary spontaneous pneumothorax. Thorax 2004;59:722-4. [Crossref] [PubMed]
- Lee SH, Choi H, Kim S, et al. Association between anger and first-onset primary spontaneous pneumothorax. Gen Hosp Psychiatry 2008;30:331-6. [Crossref] [PubMed]
- Lim HK, Yoon SH, Oh CH, et al. The impact of primary spontaneous pneumothorax on multiphasic personal inventory test results in young South Korean males. Yonsei Med J 2012;53:901-5. [Crossref] [PubMed]
- Mineo TC, Ambrogi V, Mineo D, et al. Bone mineral density improvement after lung volume reduction surgery for severe emphysema. Chest 2005;127:1960-6. [Crossref] [PubMed]
- Jung JW, Kang HR, Kim JY, et al. Are asthmatic patients prone to bone loss? Ann Allergy Asthma Immunol 2014;112:426-31. [Crossref] [PubMed]
- Seibel MJ. Biochemical markers of bone turnover: part I: biochemistry and variability. Clin Biochem Rev 2005;26:97-122. [PubMed]
- Brown JP, Delmas PD, Malaval L, et al. Serum bone Gla-protein: a specific marker for bone formation in postmenopausal osteoporosis. Lancet 1984;1:1091-3. [Crossref] [PubMed]
- Zhao D, Wang J, Liu Y, et al. Expressions and clinical significance of serum bone Gla-protein, bone alkaline phosphatase and C-terminal telopeptide of type I collagen in bone metabolism of patients with osteoporosis. Pak J Med Sci 2015;31:91-4. [PubMed]
- Clézardin P. The role of RANK/RANKL/osteoprotegerin (OPG) triad in cancer-induced bone diseases: physiopathology and clinical implications. Bull Cancer 2011;98:837-46. [PubMed]
- Hofbauer LC, Heufelder AE. Role of receptor activator of nuclear factor-kappaB ligand and osteoprotegerin in bone cell biology. J Mol Med (Berl) 2001;79:243-53. [Crossref] [PubMed]


