
Temporal trend in burden of asthma in China, South Korea, and Japan, 1990–2019: results from the Global Burden of Disease Study 2019
Highlight box
Key findings
• The burden of asthma in China, South Korea, and Japan has a downward trend, but elderly patients still need more attention. Our prediction model shows that the burden of asthma in the three East Asian countries continued to decline or stabilize until 2030, especially in China and Japan.
What is known and what is new?
• Asthma is still a public health problem worthy of concern, special in China, South Korea, and Japan.
• We clarify the temporal trend of the incidence, deaths, and DALYs of asthma in China, South Korea, and Japan by gender, age, and risk factors from 1990 to 2019 using global Burden of Disease data 2019.
What is the implication, and what should change now?
• We can more clearly understand the burden of asthma in parts of East Asia and promote a more accurate prevention and control strategy for asthma.
Introduction
Asthma is one of the most common chronic diseases in children and adults and the fastest-growing respiratory disease (1). According to the Global Burden of Disease study, the global prevalence of asthma was 262.4 million in 2019 (2). Since 2006, the Global Initiative for Asthma (GINA) began to emphasize the concept of “asthma control” (3), which reflected the change in asthma management from reducing the acute exacerbation to achieving asthma control. Presently, asthma remains a global public health concern, which imposes a large economic burden on society.
A recent study showed that the prevalence of asthma in individuals >20 years old was 4.2%, and the total number of patients was 45.7 million in China (4). China has a large number of asthma patients, characterized by sustainable growth, an extended course of the disease, repeated paroxysms, and many related comorbidities (5). The results of Phase 2 of the Asthma Insights and Reality in Asia-Pacific (AIRIAP2) showed that 53.4% of patients had uncontrolled asthma in the Asia-Pacific region, but only 2.5% of patients achieved asthma control, suggesting that the overall asthma care and control effect was not ideal (6). Owing to the increasing disease burden of asthma, many countries have raised the prevention and treatment of the disease as a national health strategy project (7).
The epidemiological distribution of asthma shows substantial geographical heterogeneity. In 2019, the age-standardized prevalence of asthma was highest in high-income North America, and lowest in East Asia (2). The deaths of asthma have declined to varying degrees in all regions of the world, with the largest decline occurring in the high-income Asia Pacific region. And Oceania has the highest age-standardized disability-adjusted life year rate (ASDALR), while East Asia has the lowest. East Asia is at a low level of asthma burden globally. Therefore, in-depth understanding of the disease burden of asthma in East Asia is more conducive to controlling the overall disease burden of asthma. Nevertheless, the epidemiology of asthma in all age groups in China or East Asia is yet to be clarified. Although China, Japan, and South Korea have many similarities in cultural, economic, and ancestral backgrounds, but the corresponding disease burden is at different levels. Therefore, the present study aimed to clarify the temporal trend of the incidence, deaths, and disability-adjusted life years (DALYs) of asthma by gender, region, and risk factors in China, Japan, and South Korea from 1990–2019. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-22/rc).
Methods
Data source
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The original data sources are derived from the Global Burden of Disease 2019 (GBD 2019) Data Input Sources Tool website (http://ghdx.healthdata.org/gbd-2019/data-input-sources). The database monitored and assessed 204 countries and regions of different disease characteristic indexes, including the incidence, deaths, and DALYs (8-11). Next, we used the data from 1990–2019 in the GBD 2019 to estimate the trends of burden of asthma in China, South Korea, Japan, and the world with three standard epidemiological measures: incidence, deaths, and DALYs. Moreover, we assessed the burden of tobacco, metabolic risks, and environmental/occupational risks between the sexes in the three countries. In the GBD 2019 research, 95% uncertainty intervals (UIs) of all estimates were reported (8,9). The age of patients was divided into the following groups: 1 to 4, 5 to 9, 10 to 14, 15 to 19, 20 to 24, 25 to 29, 30 to 34, 35 to 39, 40 to 44, 45 to 49, 50 to 54, 55 to 59, 60 to 64, 65 to 69, 70 to 74, 75 to 79, 80 to 84, 85 to 89, 90 to 94, 95 and above.
Definition of asthma
Bronchial asthma (asthma) is characterized by chronic airway inflammation and airway hyperresponsiveness (12). The typical symptom is paroxysmal expiratory dyspnea accompanied by wheezing, and a few patients have chronic cough as the only symptom. It is generally accepted that the interaction of environmental factors and associated genes contribute to the development of asthma, and the mechanism is extremely complex (13-15). The definition of asthma was coded by the 10th edition of the International Statistical Classification of Diseases and Related Health Problems (ICD-10). The coding range for asthma is J45-J46. In addition, the definition of asthma between some countries and regions is based on a doctor’s diagnosis and wheezing symptoms in the past year (2,9).
Statistical analysis
The standardized methods of the GBD 2019 have been described previously (8,9). The age- and sex-specific incidence, mortality, and DALYs from asthma were reasonably estimated for the three countries and the world from 1990–2019. Briefly, DisMod-MR 2.1, a Bayesian meta-regression tool for GBD, was used to ensure internal consistency between incidence, prevalence, excess mortality, and cause-specific mortality (8,9). Furthermore, the changes in age-standardized rates (ASRs) for incidence and mortality were assessed to evaluate the trends in disease burden of asthma for each region. We extracted data on major risk factors related to asthma, such as tobacco, metabolic factors, and environmental/occupational factors, and conducted risk factor analysis on age-standardized incidence rate (ASIR) and ASDALR between different genders. The identified trends of varying internal in ASRs were described by annual percentage change (APC), which is the change in the slope of the linear trend. Subsequently, the average annual percentage change (AAPC), a weighted average of the APC calculated by the Joinpoint Regression Program version 4.8.0.1 (https://surveillance.cancer.gov/joinpoint/).
Age-period-cohort is a common statistical analysis model, which can evaluate its impact on the outcome variables from three dimensions of age, period, and birth cohort. Based on the APC prediction model, the present study analyzed the prediction model of three East Asian countries from 1990–2019 and predicted the disease burden attributed to asthma from 2020–2030. Specifically, the model described the trends in age-standardized indicators of asthma burden every 5 years according to the independent effects of age, period, and cohort. In addition, the R package “nordpred” was used for fitting the model with a power five-link function, which has been shown to improve the accuracy of projection (16). All statistical analyses were conducted using the R program (version 4.1.2).
Results
Burden of asthma in China, South Korea, Japan, and the world
The burden of asthma in China, South Korea, Japan, and the world from 1990–2019 is shown in Tables 1,2. The incident cases, deaths, and DALYs of asthma showed a decreasing trend in China, South Korea and Japan from 1990–2019. The incident cases, and deaths of the world have a slow upward trend, but DALYs are still declining. In 2019, the incident cases, deaths, and DALYs of asthma in China were 376.13/10,000 (95% UI: 290.11–491.79), 2.48/10,000 (95% UI: 2.02–3.08), and 141.32/10,000 (95% UI: 105.23–191.88), respectively. Compared to 1990, the changes of the above indicators were −16.24% (−19.00% to −13.75%), −38.61% (−47.26% to −33.33%), and −29.48% (−29.94% to −27.18%) (Table 1). The incident cases, deaths, and DALYs of asthma in 2019 were 21.11/10,000 (17.78–25.06), 0.27/10,000 (0.20–0.33), and 10.40/10,000 (7.69–13.92) in South Korea, respectively, and 56.17/10,000 (46.71–67.68), 0.22/10,000 (0.16–0.30), and 22.20/10,000 (15.17–31.19) in Japan, respectively (Table 1). Compared to 1990, the incident cases, deaths, and DALYs of asthma in both South Korea and Japan recorded a decline in 2019.
Table 1
| China, No. ×104 (95% UI) | South Korea, No. ×104 (95% UI) | Japan, No. ×104 (95% UI) | Global, No. ×104 (95% UI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2019 | 1990 | 2019 | 1990 | 2019 | 1990 | 2019 | ||||
| Both | |||||||||||
| Incidence | 449.06 (336.35–607.12) |
376.13 (290.11–491.79) |
22.55 (18.62–27.50) |
21.11 (17.78–25.06) |
112.53 (94.54–134.70) |
56.17 (46.71–67.68) |
3,216.32 (2,575.28–4,051.31) |
3,697.93 (2,960.20–4,592.81) |
|||
| Deaths | 4.04 (3.03–5.84) |
2.48 (2.02–3.08) |
0.61 (0.39–0.72) |
0.27 (0.20–0.33) |
0.61 (0.54–0.65) |
0.22 (0.16–0.30) | 46.00 (34.26–59.96) |
46.11 (36.66–55.90) |
|||
| DALYs | 200.4 (150.20–263.50) |
141.32 (105.23–191.88) |
17.34 (13.28–21.06) |
10.40 (7.69–13.92) |
55.61 (40.61–75.23) |
22.20 (15.17–31.19) |
2,232.11 (1,790.95–2,734.42) |
2,155.10 (1,714.16–2,697.20) |
|||
| Male | |||||||||||
| Incidence | 253.07 (187.64–344.28) |
218.13 (167.58–288.42) |
11.11 (9.08–13.64) |
10.04 (8.40–12.00) |
53.03 (44.31–63.78) |
22.78 (18.55–27.78) |
1,628.01 (1,282.90–2,100.90) |
1,862.72 (1,469.48–2,364.98) |
|||
| Deaths | 2.05 (1.38–3.22) |
1.44 (1.14–1.88) |
0.27 (0.22–0.31) |
0.10 (0.08–0.12) |
0.35 (0.33–0.37) |
0.09 (0.07–0.11) |
23.29 (16.84–32.34) |
21.37 (17.41–26.02) |
|||
| DALYs | 108.39 (80.33–144.93) |
81.52 (60.43–109.56) |
8.71 (7.19–10.54) |
4.82 (3.51–6.49) |
26.69 (20.09–35.57) |
8.94 (6.22–12.57) |
1,118.99 (896.42–1,392.93) |
1,043.47 (831.89–1,305.02) |
|||
| Female | |||||||||||
| Incidence | 195.99 (148.60–260.09) |
158.00 (122.12–203.42) |
11.43 (9.31–14.09) |
11.07 (9.33–13.17) |
59.50 (49.71–70.91) |
33.38 (27.91–39.92) |
1,588.31 (1,295.51–1,970.68) |
1,835.21 (1,495.63–2,237.83) |
|||
| Deaths | 1.99 (1.32–3.61) |
1.04 (0.71–1.39) |
0.34 (0.16–0.43) |
0.17 (0.11–0.22) |
0.26 (0.21–0.29) |
0.13 (0.09–0.19) |
22.71 (15.29–31.40) |
24.74 (17.98–32.01) |
|||
| DALYs | 92.06 (67.82–133.66) |
59.80 (43.00–80.94) |
8.63 (5.87–10.85) |
5.58 (4.07–7.53) |
28.92 (20.53–39.60) |
13.26 (9.00–18.75) |
1,113.12 (854.82–1,393.92) |
1,111.63 (867.46–1,407.52) |
|||
UI, uncertainty interval; DALY, disability-adjusted life year. Data Source: Global Burden of Disease 2019.
Table 2
| ASIR/105 (95% UI) | 1990–2019 AAPC (95% CI) | ASDR/105 (95% UI) | 1990–2019 AAPC (95% CI) | ASDALR/105 (95% UI) | 1990–2019 AAPC (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2019 | 1990 | 2019 | 1990 | 2019 | ||||||
| Both | |||||||||||
| Global | 580.09 (474.68–715.04) |
504.28 (400.64–633.26) |
−0.47 (−0.67 to −0.27) |
11.91 (8.80–15.86) |
5.80 (4.62–7.03) | −2.65 (−2.73 to −2.57) |
476.28 (378.49–579.59) |
273.63 (216.71–343.38) |
−2.05 (−2.16 to −1.94) |
||
| China | 394.58 (295.36–529.45) |
355.33 (259.68–492.64) |
−0.59 (−1.25 to 0.07) |
6.37 (4.69–9.45) |
1.51 (1.23–1.86) | −5.22 (−5.45 to −5.00) |
209.24 (159.57–272.33) |
102.81 (72.30–147.42) |
−2.89 (−3.36 to −2.42) |
||
| South Korea | 586.87 (486.52–715.45) |
510.52 (400.45–652.89) |
−0.57 (−0.67 to −0.47) |
35.60 (20.81–42.09) | 3.48 (2.56–4.31) | −9.59 (−10.30 to −8.87) |
645.60 (465.16–764.32) |
178.52 (126.09–251.80) |
−5.27 (−5.65 to −4.89) |
||
| Japan | 963.11 (785.39–1201.19) |
584.11 (439.70–775.33) |
−2.50 (−2.89 to −2.10) |
4.04 (3.59–4.32) |
0.46 (0.36–0.62) | −8.46 (−8.89 to −8.02) |
401.27 (289.81–546.61) |
161.15 (104.80–241.75) |
−4.03 (−4.47 to −3.58) |
||
| Male | |||||||||||
| Global | 577.74 (466.39–721.91) |
505.76 (394.92–649.36) |
−0.40 (−0.60 to −0.19) |
13.76 (9.82–19.51) | 5.93 (4.84–7.21) | −3.06 (−3.14 to −2.98) |
498.88 (392.53–620.97) |
272.16 (216.88–340.92) |
−2.22 (−2.33 to −2.10) |
||
| China | 432.76 (321.69–584.77) |
397.59 (289.86–554.46) |
−0.42 (−1.04 to 0.21) |
7.40 (4.94–12.68) |
2.09 (1.70–2.65) | −4.55 (−4.75 to −4.34) |
231.54 (173.30–318.39) |
119.43 (86.12–169.82) |
−2.61 (−3.04 to −2.18) |
||
| South Korea | 599.09 (496.90–740.65) |
510.14 (397.98–655.36) |
−0.71 (−0.81 to −0.62) |
45.54 (34.87–53.77) | 3.68 (2.90–4.53) | −10.42 (−11.21 to −9.62) |
808.32 (669.51–938.49) |
183.17 (130.23–256.88) |
−6.14 (−6.57 to −5.71) |
||
| Japan | 952.80 (772.20–1193.38) |
515.04 (383.98–684.34) |
−3.80 (−4.33 to −3.27) |
5.83 (5.42–6.17) |
0.52 (0.41–0.65) | −9.48 (−9.94 to −9.01) |
423.97 (314.19–568.34) |
138.63 (90.93–207.19) |
−5.35 (−5.85 to −4.85) |
||
| Female | |||||||||||
| Global | 582.27 (480.29–709.48) |
501.55 (402.41–621.43) |
−0.55 (−0.75 to −0.34) |
10.67 (7.15–14.80) | 5.72 (4.16–7.39) | −2.32 (−2.41 to −2.24) |
461.30 (353.71–579.02) |
275.24 (214.89–349.63) |
−1.94 (−2.05 to −1.84) |
||
| China | 354.20 (268.02–469.26) |
309.71 (226.92–424.00) |
−0.85 (−1.57 to −0.12) |
5.71 (3.77–10.09) |
1.12 (0.78–1.51) | −5.86 (−6.12 to −5.60) |
190.74 (140.71–277.12) |
87.45 (59.60–126.36) |
−3.29 (−3.81 to −2.76) |
||
| South Korea | 575.39 (471.34–701.81) |
511.94 (405.72–653.90) |
−0.44 (−0.57 to −0.30) |
30.97 (14.04–38.85) | 3.27 (2.20–4.27) | −9.26 (−9.94 to −8.57) |
553.17 (352.88–678.08) |
176.13 (122.68–251.89) |
−4.67 (−5.04 to −4.29) |
||
| Japan | 977.54 (791.13–1202.89) |
654.04 (496.70–865.61) |
−1.48 (−1.93 to −1.04) |
2.95 (2.31–3.26) |
0.42 (0.32–0.62) | −7.56 (−7.98 to −7.15) |
389.68 (274.25–546.52) |
184.12 (119.28–277.56) |
−2.99 (−3.46 to −2.51) |
||
ASIR, age-standardized incidence rate (per 100,000); ASDR, age-standardized death rate (per 100,000); ASDALR, age-standardized DALY rate (per 100,000); AAPC, average annual percentage change; UI, uncertainty interval; CI, confidence interval; DALY, disability-adjusted life year. Data Source: Global Burden of Disease 2019.
The ASIR, age-standardized death rate (ASDR), and ASDALR of asthma in China, South Korea, Japan, and the world showed a decreasing trend from 1990–2019. In 2019, the ASIR, ASDR, and ASDALR of asthma in China were 355.33/100,000 (95% UI: 259.68–492.64), 1.51/100,000 (95% UI: 1.23–1.86), and 102.81/100,000 (95% UI: 72.30–147.42), respectively. Compared to 1990, the changes were −9.95% (−12.08% to −6.95%), −76.30% (−80.32% to −73.77%), and −50.87% (−54.69% to −45.87%) in 2019 (Table 2). Notably, the burden of asthma in terms of incidence, deaths, and DALYs in China ranked top among the three countries in 2019, but ASRs were lower than that of Japan and South Korea (Tables 1,2). In terms of gender, the asthma burden of males in China was worse than that of females. Conversely, the burden of asthma in Japan was worse for females than for males and was close to equilibrium by gender in South Korea (Tables 1,2). The ASDR of asthma in China declined obviously from 1990–2019 with AAPC of −5.22 [95% confidence interval (CI): −5.45 to −5.00], and the AAPCs in ASIR and ASDALR of asthma in China were −0.59 (95% CI: −1.25 to 0.07) and −2.89 (95% CI: −3.36 to −2.42) (Table 2).
Age-wise distribution of asthma burden
The data of incident cases, deaths, and DALYs of asthma in different age groups in China, South Korea, Japan, and the world from 1990–2019 are shown in Figure 1. From 1990–2019, the burden of asthma was primarily concentrated in <19 and >65 years old age groups in China, South Korea, Japan, and the world (Figure 1A-1D). The overall burden of asthma in different age groups in China from 1990–2019 is on the decline, and the number of asthma patients increased slightly after 40 years of age and reached a peak at the age of 65 years (Figure 1B). Notably, the incident cases of asthma worldwide have a slow downward trend, and the number of cases of individuals >40 years in China and South Korea is increasing slightly (Figure 1A-1C). The deaths of asthma in the world are in the declining stage, and the number of patients >90 years old in South Korea and Japan is augmenting acutely (Figure 1A,1C,1D). The DALYs in China, South Korea, Japan, and the world have decreased in varying degrees in different age groups, while the DALYs in >95 years old in South Korea and Japan are increasing (Figure 1A-1D).

Burden of asthma by gender
The ASIR, ASDR, and ASDALR of asthma of different genders in China, South Korea, Japan, and the world are shown in Figure 2. Globally, 505.76/100,000 (95% UI: 394.92–649.36) of the ASIR with asthma occurred in males compared to 501.55/100,000 (95% UI: 402.41–621.43) in females in 2019 (Figure 2A and Table 2). The ASDR in males with asthma worldwide was 5.93/100,000 (95% UI: 4.84–7.21) compared to 5.72/100,000 (95% UI: 4.16–7.39) in females in 2019 (Figure 2B and Table 2). The ASDALR in males with asthma worldwide was 272.16/100,000 (95% UI: 216.88–340.92) compared to 275.24/100,000 (95% UI: 214.89–349.63) in females in 2019 (Figure 2C and Table 2). In 2019, 56.21% (397.59/100,000) of the ASIR of asthma occurred in males compared to 43.79% (309.71/100,000) in females in China (Table 2). Among ASDR of asthma in China, males accounted for 65.11% (2.09/100,000) and females accounted for 34.89% (1.12/100,000) of all patients (Table 1). The ASDR of asthma between males and females in China, South Korea, Japan, and the world is in a continuous downward trend (Figure 2B). The ASIR and ASDALR of asthma of different genders in China, South Korea, and Japan declined first and stabilized (Figure 2A,2C). Compared to 1990, the ASIR and ASDR in males decreased markedly in South Korea and Japan, and ASDALR in females reduced significantly in China and South Korea in 2019.

Prediction of asthma burden
The predictions of asthma disease burden are shown in Figure 3. In 2030, the projected ASIR, ASDR, and ASDALR of asthma in China would be 323.05/100,000 (95% CI: 317.21–329.39), 0.81/100,000 (95% CI: 0.55–1.17), and 83.21/10,000 (95% CI: 72.96–96.33), respectively (Figure 3A-3C). From 2019–2030, the ASIR of asthma in China and Japan continued to decrease from 355.33/100,000 (95% UI: 259.68–492.64) in 2019 to 323.05/100,000 (95% CI: 317.21–329.39) in 2030, and from 584.11/100,000 (95% UI: 439.70–775.33) in 2019 to 541.35/100,000 (95% CI: 514.97–573.44) in 2030 (Table 2 and Figure 3A). The world’s ASIR remained stable at around 510.52/100,000 (95% UI: 400.45–652.89), while South Korea’s ASIR increased slightly from 510.52/100,000 (95% UI: 400.45–652.89) in 2019 to 533.79/100,000 (95% CI: 524.59–543.55) in 2030 (Table 2 and Figure 3A).
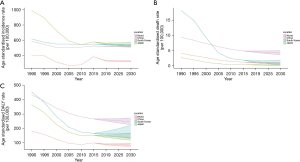
Regarding ASDR of asthma, these countries showed a downward trend, with the number of patients in China, South Korea, and Japan decreasing from 1.51/100,000 to 0.81/100,000, from 3.48/100,000 to 0.87/100,000, and from 0.46/100,000 to 0.22/100,000, respectively (Table 2 and Figure 3B). The ASDALR of asthma in China, South Korea, and Japan decreased from 102.81/100,000 to 83.21/100,000, from 178.52/100,000 to 167.07/100,000, and from 161.15/100,000 to 137.78/100,000, respectively (Table 2 and Figure 3C). The results of the prediction model showed that the burden of asthma in China, Japan, and the world declined slowly and stabilized gradually in the future.
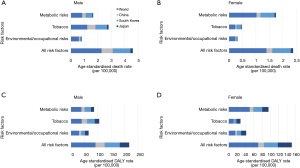
Risk factors of asthma in China, South Korea, Japan, and the world
In 2019, the global leading risk factor for ASDR due to asthma was tobacco in males, which accounted for 12.14/100,000 (95% UI: 6.48–16.98) (Figure 4A). The main risk factors for ASDR in females worldwide were metabolic and environmental/occupational factors, which accounted for 10.20/100,000 (95% UI: 5.29–16.82) and 2.40/100,000 (95% UI: 1.75–3.14), respectively (Figure 4B). The principal risk factor for ASDALR in males and females worldwide was tobacco, which accounted for 40.29/100,000 (95% UI: 21.87–56.08) and 50.45/100,000 (95% UI: 28.84–78.13) (Figure 4C,4D). Tobacco was the main contributor to male ASDALR of asthma in China, South Korea, Japan, and the world (>40.29%, 16.69%, 15.94%, and 11.86%, respectively), but the minor contributor to female ASDALR (1.73, 3.01%, 5.07%, and 4.41%, respectively) (Figure 4A-4D). The present study showed that South Korean male is most affected by these three risk factors in China, South Korea, and Japan. In addition to metabolic factors, the principal feature in China, Japan, and South Korea is that males are more affected by risk factors than females (Figure 4A-4D).
Discussion
This study systematically summarized the burden of asthma, its temporal trend and risk factors in China, South Korea and Japan from 1990 to 2019, as well as the predictions until 2030. The burden of asthma continued to decline in the world, but the incident cases, deaths and DALYs in South Korea were still high. From a global perspective, the disease burden of asthma in the entire Asian region is at a low level. However, there are many significant differences between Asian regions, especially between East Asia and Central Asia and Southeast Asia (2). It is worth noting that the burden of ASDR in the three countries has declined sharply, especially in China. The results of this article show that there are deficiencies in the level of asthma control in China, South Korea and Japan, but there are still different degrees of improvement in the prevention and control of asthma.
The current results showed that the main population suffering from asthma was the children and elderly in China, South Korea, and Japan over the past three decades. This finding was consistent with the general occurrence pattern of asthma (17,18). We also demonstrated that from 1990–2019, the level of asthma control in China was better than the global level and the overall disease burden improved significantly, but the control effect was worse than that of South Korea and Japan. In the current study, the ASIR, ASDR, and ASDALR of different age groups in China, South Korea, and Japan showed a certain downward trend in the past 30 years, and the ASDR decreased significantly. This phenomenon might be attributed to the rational use of inhalation corticosteroids, which decreased the mortality of asthma patients (18). This finding is closely related to the growing global emphasis on respiratory diseases and the improvement of related health conditions. Notably, our prediction model showed that the overall disease burden of China, South Korea, and Japan has a slight decline or balance from 2020–2030. Specifically, ASDR would have a distinct downward trend in 2030, which might be related to the increasingly progressive medical and health environment and disease attention globally.
The morbidity of asthma is closely related to age and gender, but the idiographic mechanism is complicated. This study demonstrated that the burden of male asthma is higher than that of females in China, and the burden of Japanese females is slightly higher than that of males. The gender variations between China and South Korea are different from the anterior epidemiological studies, which may be closely related to the differences in gender composition. Typically, female is about 10.5% more likely than males to suffer from asthma over their lifetime. The morbidity of asthma in adolescent boys aged <18 years is significantly higher than that of girls of the same age (18). This phenomenon indicated sex-related differences in morbidity due to the influence of sex hormones (7,17,19). In addition, the high morbidity of boys is partially due to the fact that the airway of adolescent boys is smaller than that of young girls, which is reversed after puberty (17,20,21). Moreover, the burden of asthma by gender differences is impacted in genetics/epigenetics, sex hormones, social and environmental factors, and response to therapeutics. Gender differences in environmental exposures and healthcare utilization are crucial factors to consider in asthma (19).
In the present study, the number of asthma deaths from asthma and DALYs decreased in different age groups in China, South Korea, Japan, and the world, with the most obvious decrease in South Korea and Japan. This study also demonstrated that the burden of asthma for the elderly in these three countries was high, especially in South Korea and Japan. Baptist et al. (22). confirmed that asthma is a common occurrence among individuals >65 years old, and the elderly had a higher incidence and mortality than other age groups. A Japanese study (23) revealed that elderly patients accounted for nearly 90% of the total asthma-related mortality. Patients aged ≥75 years accounted for about 80% of all deaths. Elderly patients with asthma do not have any typical symptoms of asthma, and fatigue is often the main symptom (22). Compared to young people, elderly patients had lower forced expiratory volume in 1 second (FEV1) and FEV1% prediction and more severe airflow restriction (24). The pathophysiology of asthma in elderly patients is not as good as that in young people and children (25). In addition, older patients with asthma may have altered airway and systemic inflammation, which responds less to corticosteroid therapy (22).
A previous study comprehensively reviewed potential risk factors of asthma, and the differences in the distribution of these risk factors might explain the differences in the prevalence of asthma (9). Moreover, the risk factors in East Asia and the world are different between genders and across countries. However, tobacco is still one of the major risk factors for asthma (4,26). The current study showed that the risk factors attributed to tobacco in China, South Korea, and Japan have a declining trend. This phenomenon may be closely related to the implementation and promotion of the 2005 World Health Organization (WHO) Framework Convention on tobacco control (27,28). Therefore, the implementation of various tobacco control measures, such as banning sales to teenagers, prohibiting smoking in public places, and publicizing the harm of smoking, is conducive to the effective control of the burden of asthma (29,30).
We also found that metabolic and environmental/occupational factors have varied patterns for asthma development in China, Japan, South Korea, and the world. In terms of metabolic risks, obesity increases the risk of asthma in both genders, especially with a pronounced effect in females (31). A cohort study suggested that before conception, a father’s high body mass index (BMI) trajectory increases the risk of asthma in his offspring (32). In East Asia, environmental/occupational factors are the key risk factors for asthma. Polluted air not only aggravates the symptoms but also leads to the development of childhood asthma (33). A parentally administered questionnaire revealed (34) that long-term exposure to NO2, PM10, and traffic air pollution could be risk factors for asthma in Chinese children. In addition, about 10–25% of adult-onset asthma is a work-related exposure (31). The common features of work-related asthma (WRA) are the symptoms and signs corresponding to asthma and the correlation with workplace exposure (35).
Nevertheless, the present study has several limitations. First, the main limitation of this study is that the data are from GBD 2019. Due to the limited data, there is a lack of analysis of disease subtypes. The analysis of different subtypes may be conducive to an overall understanding of the disease. Second, the misdiagnosis rate of each country should be considered. Since most patients with asthma are determined by spirometry, the lack of spirometry evaluation would lead to misdiagnosis and insufficient diagnosis. Third, this study only considers limited risk factors. The risk factors of asthma can also be attributed to other proven factors, such as air pollution, obesity, and psychosocial stress. Due to the limited data in GBD 2019, some risk factors were not considered. The present study is a comprehensive and systematic report on the regional disease burden of asthma in the world, which provides a foundation for better control and management of the disease in the future.
Conclusions
According to GBD 2019, heterogeneity was detected in the epidemiology of asthma across gender, age, and risk factors in three East Asian countries. With the increasing middle-aged and elderly population in several countries, asthma increases the economic burden of public health. Therefore, the prevention measures for middle-aged and senior patients, such as smoking control and improving living and working environment, would be optimal for different genders, age groups, and locations.
Acknowledgments
Funding: This work was supported by Open Project of State Key Laboratory of Respiratory Disease (No. SKLRD-OP-202008), Guangdong Science and Technology program (No. 2021A0505020012), and Incubation Program of National Science Foundation for Distinguished Young Scholars by Guangzhou Medical University (No. GMU2020-207).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-22/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-22/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-22/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ramsahai JM, Hansbro PM, Wark PAB. Mechanisms and Management of Asthma Exacerbations. Am J Respir Crit Care Med 2019;199:423-32. [Crossref] [PubMed]
- Safiri S, Carson-Chahhoud K, Karamzad N, et al. Prevalence, Deaths, and Disability-Adjusted Life-Years Due to Asthma and Its Attributable Risk Factors in 204 Countries and Territories, 1990-2019. Chest 2022;161:318-29. [Crossref] [PubMed]
- Global Initiative for Asthma. Global strategy for asthma management and prevention: update 2019. [2019-04-13]. Available online: http://www.ginaasthma.org/
- Huang K, Yang T, Xu J, et al. Prevalence, risk factors, and management of asthma in China: a national cross-sectional study. Lancet 2019;394:407-18. [Crossref] [PubMed]
- Zhong N, Lin J, Zheng J, et al. Uncontrolled asthma and its risk factors in adult Chinese asthma patients. Ther Adv Respir Dis 2016;10:507-17. [Crossref] [PubMed]
- Wong GW, Kwon N, Hong JG, et al. Pediatric asthma control in Asia: phase 2 of the Asthma Insights and Reality in Asia-Pacific (AIRIAP 2) survey. Allergy 2013;68:524-30. [Crossref] [PubMed]
- Stern J, Pier J, Litonjua AA. Asthma epidemiology and risk factors. Semin Immunopathol 2020;42:5-15. [Crossref] [PubMed]
- Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1223-49. [Crossref] [PubMed]
- Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1204-22. [Crossref] [PubMed]
- Global Burden of Disease Cancer Collaboration. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 2019;5:1749-68. [Crossref] [PubMed]
- O’Donovan MR, Sezgin D, Liew A, et al. Burden of disease, disability-adjusted life years and frailty prevalence. QJM 2019;112:261-7. [Crossref] [PubMed]
- Reddel HK, Bacharier LB, Bateman ED, et al. Global Initiative for Asthma Strategy 2021: executive summary and rationale for key changes. Eur Respir J 2022;59:2102730. [Crossref] [PubMed]
- Weinmann T, Gerlich J, Heinrich S, et al. Establishing a birth cohort to investigate the course and aetiology of asthma and allergies across three generations - rationale, design, and methods of the ACROSSOLAR study. BMC Public Health 2015;15:1210. [Crossref] [PubMed]
- Azalim S, Camargos P, Alves AL, et al. Exposure to environmental factors and relationship to allergic rhinitis and/or asthma. Ann Agric Environ Med 2014;21:59-63. [PubMed]
- Hur GY, Broide DH. Genes and Pathways Regulating Decline in Lung Function and Airway Remodeling in Asthma. Allergy Asthma Immunol Res 2019;11:604-21. [Crossref] [PubMed]
- Møller B, Fekjaer H, Hakulinen T, et al. Prediction of cancer incidence in the Nordic countries up to the year 2020. Eur J Cancer Prev 2002;11:S1-96. [PubMed]
- Dharmage SC, Perret JL, Custovic A. Epidemiology of Asthma in Children and Adults. Front Pediatr 2019;7:246. [Crossref] [PubMed]
- Papi A, Brightling C, Pedersen SE, et al. Asthma. Lancet 2018;391:783-800. [Crossref] [PubMed]
- Chowdhury NU, Guntur VP, Newcomb DC, et al. Sex and gender in asthma. Eur Respir Rev 2021;30:210067. [Crossref] [PubMed]
- Becklake MR, Kauffmann F. Gender differences in airway behaviour over the human life span. Thorax 1999;54:1119-38. [Crossref] [PubMed]
- Wright AL. Epidemiology of asthma and recurrent wheeze in childhood. Clin Rev Allergy Immunol 2002;22:33-44. [Crossref] [PubMed]
- Baptist AP, Busse PJ. Asthma Over the Age of 65: All’s Well That Ends Well. J Allergy Clin Immunol Pract 2018;6:764-73. [Crossref] [PubMed]
- Nakamura Y, Tamaoki J, Nagase H, et al. Japanese guidelines for adult asthma 2020. Allergol Int 2020;69:519-48. [Crossref] [PubMed]
- Tsai CL, Delclos GL, Huang JS, et al. Age-related differences in asthma outcomes in the United States, 1988-2006. Ann Allergy Asthma Immunol 2013;110:240-6, 246.e1.
- Dunn RM, Busse PJ, Wechsler ME. Asthma in the elderly and late-onset adult asthma. Allergy 2018;73:284-94. [Crossref] [PubMed]
- Murrison LB, Brandt EB, Myers JB, et al. Environmental exposures and mechanisms in allergy and asthma development. J Clin Invest 2019;129:1504-15. [Crossref] [PubMed]
- Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet 2017;389:1885-906. [Crossref] [PubMed]
- Hoffman SJ, Mammone J, Rogers Van Katwyk S, et al. Cigarette consumption estimates for 71 countries from 1970 to 2015: systematic collection of comparable data to facilitate quasi-experimental evaluations of national and global tobacco control interventions. BMJ 2019;365:l2231. [Crossref] [PubMed]
- Bilano V, Gilmour S, Moffiet T, et al. Global trends and projections for tobacco use, 1990-2025: an analysis of smoking indicators from the WHO Comprehensive Information Systems for Tobacco Control. Lancet 2015;385:966-76. [Crossref] [PubMed]
- Hoffman SJ, Poirier MJP, Rogers Van Katwyk S, et al. Impact of the WHO Framework Convention on Tobacco Control on global cigarette consumption: quasi-experimental evaluations using interrupted time series analysis and in-sample forecast event modelling. BMJ 2019;365:l2287. [Crossref] [PubMed]
- Kuruvilla ME, Vanijcharoenkarn K, Shih JA, et al. Epidemiology and risk factors for asthma. Respir Med 2019;149:16-22. [Crossref] [PubMed]
- Bowatte G, Bui DS, Priyankara S, et al. Parental preconception BMI trajectories from childhood to adolescence and asthma in the future offspring. J Allergy Clin Immunol 2022;150:67-74.e30. [Crossref] [PubMed]
- Pfeffer PE, Mudway IS, Grigg J. Air Pollution and Asthma: Mechanisms of Harm and Considerations for Clinical Interventions. Chest 2021;159:1346-55. [Crossref] [PubMed]
- Norbäck D, Lu C, Wang J, et al. Asthma and rhinitis among Chinese children - Indoor and outdoor air pollution and indicators of socioeconomic status (SES). Environ Int 2018;115:1-8. [Crossref] [PubMed]
- Maestrelli P, Henneberger PK, Tarlo S, et al. Causes and Phenotypes of Work-Related Asthma. Int J Environ Res Public Health 2020;17:4713. [Crossref] [PubMed]


