Hypoxemia associated with right-side cardiac tumor: right atrial lymphoma with patent foramen ovale
Introduction
Patients with right-sided cardiac tumor rarely present with hypoxemia unless they are associated with pulmonary embolism. We report a case of cardiac diffuse large B-cell lymphoma (DLBCL) of the right atrium (RA) causing significant right-to left shunting via a patent foramen ovale (PFO).
Case presentation
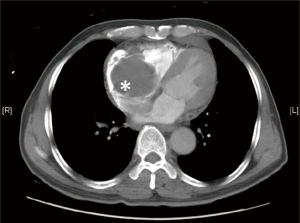
A 66-year-old man presented with dyspnea and intermittent palpitation for 1 week with no associated chest pain, leg swelling or dizziness. He had no recent long-haul flights. Arterial blood gas showed type 1 respiratory failure and increased alveolar-arterial gradient, despite a chest X-ray showing clear lung fields. ECG showed sinus rhythm with no ischemic changes or right heart strain pattern. Urgent contrast computed tomography (CT) scan of thorax showed a 6.5-cm soft tissue density in RA (Figure 1) and no evidence of pulmonary embolism or parenchymal lung disease.
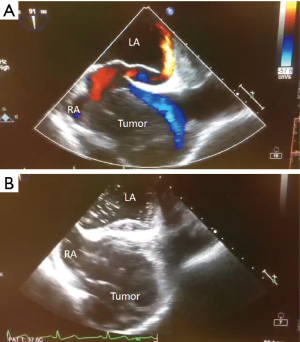
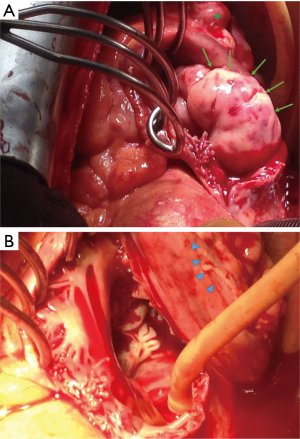
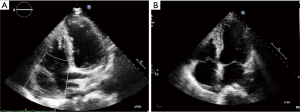
An emergency operation was performed. On-table trans-esophageal echocardiogram showed a 2-cm PFO with right to left shunt (Figures 2-4). There was a fungating right atrial tumor arose from the atrio-ventricular (AV) groove and extended to the right ventricle surface (Figure 5A). Cardiopulmonary bypass circuit was achieved via right femoral arterial and venous cannulation. A right atriotomy was made distant from the tumor margin. It was noted that the right atrial tumor arose from the AV groove with a 6-cm tumor bulk within the RA. There is no tumor invasion to the tricuspid valve, the vena cava, interatrial septum and coronary sinus. As the tumor involved the AV groove and was not feasible for complete tumor resection, only the intra-atrial part of the tumor was debulked (Figure 5B). The PFO was closed with plegetted 3/0 polypropylene suture. The right atriotomy was closed followed by decannulation and successful weaning from cardiopulmonary bypass. Post-operative trans-esophageal echocardiogram showed no tumor mass within the right cardiac chambers and no residual intra-cardial shunting. The total bypass time was 37 minutes, and the total operative time was 130 minutes.


Pathology of the right atrial mass showed DLBCL. Positron-emission tomography (PET) scan showed no lymphoma involvement in other organs. He was given chemotherapy (R-CHOP regimen) by Oncologist. Echocardiography 7 months after the operation showed no right atrial tumor, intra-cardiac shunt or pericardial effusion (Figure 6). He remained well 14 months after operation with no heart failure symptoms or lymphoma recurrence.
Discussion
Primary cardiac tumors had a wide range of presentations including dyspnea and palpitation. Type 1 respiratory failure, suggested by hypoxemia in blood gas analysis, was a rare encounter in right-sided cardiac tumor in the absence of embolism into the pulmonary circulation. For our patient, we postulate the hypoxemia was secondary to a forced right-to-left shunt from a huge space occupying tumor in the RA. A careful echocardiogram study is the key diagnostic tool for explaining the abnormalities.
Primary cardiac lymphoma comprises only a tiny proportion (1.3%) of all primary cardiac tumors (3). The commonest non-Hodgkin subtype was DLBCL (4). This subtype, like its extra-cardiac counterparts, was highly malignant and aggressive. Although primary cardiac malignant neoplasms were notoriously known to have poor prognosis, good clinical outcomes were commonly reported after treatments for cardiac lymphoma with overall response rate up to 79% and complete remission rate up to 59% (4). Although surgery alone was not shown to improve survival (4,5), it palliates immediate hemodynamic disturbances, and allows definite histological diagnosis to guide oncological therapies.
Complete surgical resection is ideal but may not be feasible because of tumor extension or invasion. Moreover, it may not be a necessity for good survival. The longest survival of primary cardiac DLBCL after combined partial resection and chemotherapy was at least 13 years (6). It may be explained by the intrinsic high sensitivity of the tumor to cytotoxic agents, and further improved sensitivity after tumor debulking.
Conclusions
Hypoxemia is not a common presentation/association with right-sided cardiac tumors. Meticulous echocardiographic exam is necessary to look for any intracardiac shunts. Surgery is the single most important initial management in that it prevents or relieves any hemodynamically significant mechanical sequelae (e.g., obstruction, compression, embolism), and allows histological diagnosis which guides adjuvant therapy. Definite histological diagnosis is essential, as cardiac lymphoma is distinct from other primary cardiac malignancy in terms of a much better prognosis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Yu PS, Ng CS, Wong RH, et al. Color Doppler in intra-operative trans-esophageal echocardiogram. Asvide 2016;3:258. Available online: http://www.asvide.com/articles/1020
- Yu PS, Ng CS, Wong RH, et al. Bubble saline injection in intra-operative trans-esophageal echocardiogram. Asvide 2016;3:259. Available online: http://www.asvide.com/articles/1021
- Johri A, Baetz T, Isotalo PA, et al. Primary cardiac diffuse large B cell lymphoma presenting with superior vena cava syndrome. Can J Cardiol 2009;25:e210-2. [Crossref] [PubMed]
- Petrich A, Cho SI, Billett H. Primary cardiac lymphoma: an analysis of presentation, treatment, and outcome patterns. Cancer 2011;117:581-9. [Crossref] [PubMed]
- Ceresoli GL, Ferreri AJ, Bucci E, et al. Primary cardiac lymphoma in immunocompetent patients: diagnostic and therapeutic management. Cancer 1997;80:1497-506. [Crossref] [PubMed]
- Gyoten T, Doi T, Nagura S, et al. Primary cardiac malignant lymphoma: survival for 13 years after surgical resection and adjuvant chemotherapy. Ann Thorac Surg 2015;99:1060-2. [Crossref] [PubMed]