A 20-year study on treating childhood infective endocarditis with valve replacement in a single cardiac center in China
Introduction
Infective endocarditis (IE) in children is an uncommon infection and was previously only a rare complication of rheumatic heart disease. In developed countries, majority of patients developing IE in childhood are the patients living with surgical repairs of congenital lesions (1). While in developing countries, where rheumatic heart disease is still prevalent, antibiotic prophylaxis for potential septic procedures is not routinely followed and late referral is common (2). In all age groups, IE leads to significant morbidity and mortality. Although IE occurs less in children than in adults, childhood IE leads to significant morbidity and mortality (3). If medical management fails or complications of endocarditis ensue, timely surgical intervention is crucial for prognosis (4,5). Hickey et al. (6) have indicated that native valve preservation should be preferred in the children with IE. Though valve replacement confers to a high risk of repeat replacement at the 15th year (7), valve replacement is necessary in many Chinese children with IE because either they come to hospital with advanced clinical manifestations or their valves are damaged too severely where preservation of the values is not a feasible option.
The purpose of our study was to review the 20-year treatment experience of childhood IE with valve replacement surgery at our institution with regard to incidence, pathologic status, diagnosis, surgical strategies, operative mortality, recurrence of infection, re-operation, short-term and long-term surgical results.
Methods
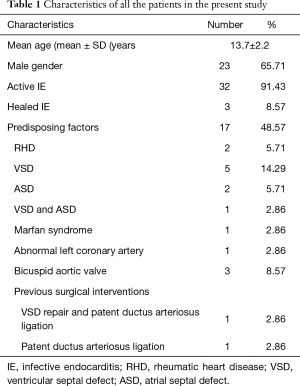
We reviewed the cardiac surgery database of Shanghai Changhai Hospital (a 1,000-bed tertiary care teaching hospital with an annual cardiac operations of approximately 1,200) to identify the pediatric patients who had surgery for native valve endocarditis (NVE) from January 1993 to December 2013. A total of 35 children (23 boys, 12 girls), with a mean age of 13.7±2.2 years, underwent surgery for IE. They represent 9% of the total 388 cardiovascular surgical procedures performed for IE at our institution during that period. The acute clinical events present on admission or before surgery were recorded. Preoperative transthoracic echocardiographic (TTE) evaluation was performed in all patients. All patients had three sets of blood cultures (with two bottles per set), separated from each other by at least 1 h, and obtained from different venipuncture sites over 24 h. The review of these patients was approved by our institutional committee for human research. Follow-up was available to a mean of 9.5±3.6 years after surgery with a total of 160 patient years.
The patients’ temperature was controlled and monitored for over 2 weeks before the surgery. The mean time from surgery after the diagnosis of IE was 3–21 days. Congestive heart failure, accompanying other heart diseases, persistent sepsis and systemic emboli were considered as the primary indication for operation. All operations were performed through a median sternotomy on full cardiopulmonary bypass between the 2 venae cava and the ascending aorta. Mild systemic hypothermia (28–30 °C) was used in all the patients. Myocardial protection was identical for all patients and consisted of an anterograde cold blood crystalloid cardioplegia with topical ice slush.
Our principles of surgical intervention for IE consisted of uncompromising and thorough excision of all infected material and tissues, cutting back until healthy tissues were identified and followed by appropriate reconstruction. If the infection extended to the annulus or surrounding structures, a radical resection of the abscess and patch reconstruction of the annulus and adjoining structures was accomplished with fresh autologous pericardium. When infection was limited to the leaflets of the native valve, valve repair or simple replacement was performed. Valve repair was preferred option when adequate valve tissue was left after complete excision of infected material. When infection had extended to or beyond the annulus, as seen with abscess formation, then surgical intervention consisted of radical resection of all infected tissue, followed by reconstruction as necessary with valve replacement.
Data were procured from institutional medical records detailing patient demographics, pre-intervention echocardiography and angiography, operative procedures, subsequent clinic attendances and autopsy reports in the advent of death. Data were analyzed by using SPSS statistical software (Version 15.0). Data are presented as frequencies, medians with ranges, means with standard deviations or odds/hazard ratios with 95% confidence intervals (CI) as appropriate. Actuarial time-related outcomes were calculated by using Kaplan-Meier principles. In the case of missing data, mean values were imputed and the frequency of the missing data was indicated. Statistical significance was considered as P<0.05.
Results
Clinical characteristics
The characteristics of the patients are shown in Table 1. Endocarditis was active in 32 patients and healed in 3 (8.6%) patients with a mean age of 13.7±2.2 years. Predisposing factors were found in 17 (48.6%) patients, with rheumatic heart valve disease in 2 (5.7%), and congenital heart disease (CHD) in 15(42.8%). Previous sternotomy had been performed on one patient for VSD repair and patent ductus arteriosus ligation, and another patient had undergone patent ductus ligation via thoracotomy.
Full table
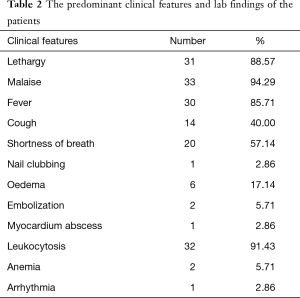
Most of the patients had constitutional and non-specific features of systemic sepsis such as lethargy, malaise and fever. While physical signs associated with adult IE such as nail clubbing, Osler’s nodes, Janeway lesions or splinter hemorrhages were uncommon. About 32 (91.43%) patients had elevated inflammatory markers or leukocytosis. Some patients had anemia, myocardium abscess, thrombocytopenia, and high level of creatinine. The diagnosis of embolism event was based on clinical signs and data derived from non-invasive procedure. Clinical embolization had occurred preoperatively in 2 (5.71%) patients (Table 2).
Full table
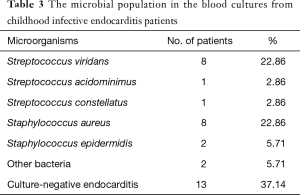
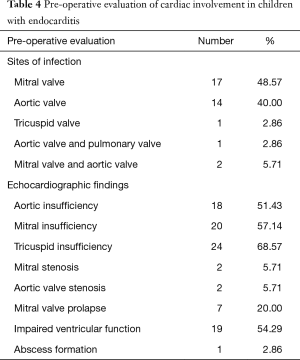
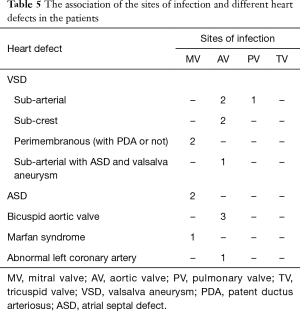
Different microorganisms were grown in blood cultures (n=22) (Table 3). Staphylococci and Streptococci were seen in equal number of patients. The preoperative TTE findings showed that the aortic and mitral valves were the primary sites of infection, while the pulmonary and tricuspid valves were less frequently involved (Table 4). Two valves involvement was seen in 3 (8.6%) patients. CHD was present in 15 (42.8%) children. The sites of infection associated with different heart defects are shown in Table 5.
Full table
Full table
Full table
Operative procedure
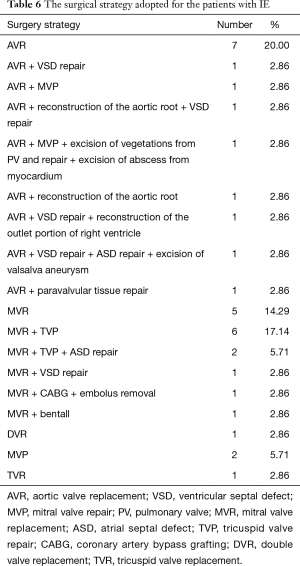
The distribution of operative procedures is shown in Table 6. Aortic value replacement (AVR) was the common procedure performed. Valve replacement has to be performed on many children with IE where there is advanced damage of valves, and the most frequently used valve was Regent mechanical valve with size ranged from 12 to 18. The superior leaflet, tendon and papillary muscle were preserved when mitral valve replacement (MVR) was performed. The patient suffering from coronary artery embolization underwent coronary artery bypass grafting and the embolus was removed.
Full table
Outcome
All patients were placed under postoperative antibiotic regimens for a period of 4 to 6 weeks. The median intensive care stay was 6 (range, 3–26) days. Important postoperative complications included rhythm disturbances in two with AF and supraventricular tachycardia, the underlying mechanism may be injuries due to surgery and inflammation in CPB, the both patients were treated with anti-arrhythmia drugs and recovered without recurrence. We also recorded aortic root abscess in one, and superior vein compression in one patient a year after operation.
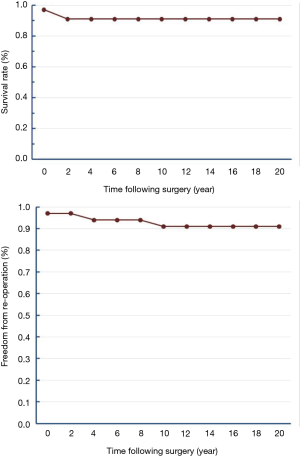
There was one early death due to abscess formation in the root of aorta in 1 month after AVR for IE of aortic valve. One patient who had undergone double valve replacement (DVR) was infected by Streptococcus again after 2 years post-surgery, and was cured by antibiotics. One patient was diagnosed to have dissection of descending aorta 7 years after surgery, and was found to have anticoagulation complications after 1 year. One patient died after Re-AVR surgery for IE of the mechanical aortic valve in 2 years after the first AVR surgery. While the other one was cured by re-AVR surgery for IE of the mechanical aortic valve 10 years after the first AVR surgery (Figure 1).
Discussion
IE is an uncommon infection in childhood and occurs primarily in children with CHD (8), while rheumatic heart disease is a rarely seen in developed countries (3,9). IE in children leads to significant morbidity and mortality. Although rheumatic heart disease is still prevalent in China, it is not an important cause of IE in children unlike in Pakistan (10). In the 1990’s, Staphylococcus aureus (S. aureus) endocarditis was less frequent than the Streptococcus endocarditis with prevalence ranging from 8% to 30% (11). A population-based study from 1970 to 2000 in Minnesota, USA, showed predominant presence of viridans group Streptococci (VGS) in adult IE (12). We identified higher rates of S. aureus infections in our IE case series. The change in trend of etiological agents and increasing incidence of S. aureus in childhood IE has been reported in some recent case series (3,13-15). We observed IE by S. aureus and Streptococcus in equal number of patients and culture-negative endocarditis in 13 (37.1%). As to fungal endocarditis, we have not recorded patients in our center, and the related reports were only scatter cases. Reported prevalence rates of IE with negative blood cultures ranged between 10% and 30% and found even higher in Pakistan and Eastern Europe (16,17). One of the main causes of negative blood cultures in IE patients is antibiotic pretreatment. The antibiotic abuse was also said to be prevalent in China before the 21st century.
The rate of emergence of resistant and multi-resistant bacteria has increased during the past two decades, especially among gram-positive microorganisms and so in some IE cases surgical treatment is needed. The clinical manifestations of IE are predominantly vague and constitutional, rather than specific. The predominant clinical features of IE in our series were lethargy, malaise, fever and leukocytosis that led to misdiagnosis and improper treatment in some patients before final diagnosis was made. Valve replacements were performed in many children with IE in China instead of valve repair because often the valve was damaged too severely to be preserved. In children with damaged AV who needed AVR, Ross procedure was reported to be alternative option in early years, but because of shortage of homograft and the difficulties of procedure, Ross procedure was scarce in China.
Some centers have reported their recent surgical experience with infective IE in children. In a 29-year study period by Hickey’s group on 30 children under the age of 18, valve replacement was performed in 24% (6). They observed lower 5-year survival in patients who underwent valve repair operation. Monro’s group studied 16 children with IE (18). Compared with Hickey’s study, Monro’s group reported prosthetic tissue IE in 19% of cases with similar anatomical distribution of infected valves, etiologic organisms and associated congenital heart defects (69%). Interestingly, they described slightly a higher rate of cusp perforation, abscess formation or chordal rupture which may explain higher valve replacement rate of 63%. Preservation of native valve in childhood IE patients in China is difficult, although many doctors feel that valve repair is better than valve replacement (18). Factors such as expense for treatment, transportation inconvenience, and neglect of the common early clinical features affect the surgical option of IE treatment in the developing country. In Hickey’s group, the rate of 10-year freedom from re-operation was 60%±18%, while it was 91% in our study.
From our experience, we found that valve replacement was not worst option as thought before, even the rate of 5-year survival and freedom from re-operation of the patient who underwent valve replacement is better than that of the patient who underwent valve repair operation, although it is not the primary choice for the children with IE. Preservation of the native valve will improve late survival, freedom from re-operation and functional outcomes. The first contact pediatric doctors should pay attention to the common clinical features of IE to diagnose the condition early and consider early referral so that the native valve as far as possible could be preserved, especially in the developing countries.
Limitations
The present study is limited by the smaller number of subjects and the unknown population denominator of children diagnosed with IE during the study period. However, it serves to emphasize that valve replacement may be better than valve repair if done early in the disease process.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The review of these patients was approved by our institutional committee for human research.
References
- Morris CD, Reller MD, Menashe VD. Thirty-year incidence of infective endocarditis after surgery for congenital heart defect. JAMA 1998;279:599-603. [Crossref] [PubMed]
- Sadiq M, Nazir M, Sheikh SA. Infective endocarditis in children--incidence, pattern, diagnosis and management in a developing country. Int J Cardiol 2001;78:175-82. [Crossref] [PubMed]
- Liew WK, Tan TH, Wong KY. Infective endocarditis in childhood: a seven-year experience. Singapore Med J 2004;45:525-9. [PubMed]
- Cheng TO. Infective endocarditis: to operate or not to operate? That's a question that is still unresolved. Int J Cardiol 2009;135:1-3. [Crossref] [PubMed]
- O'Gara PT. Infective endocarditis 2006: indications for surgery. Trans Am Clin Climatol Assoc 2007;118:187-98. [PubMed]
- Hickey EJ, Jung G, Manlhiot C, et al. Infective endocarditis in children: native valve preservation is frequently possible despite advanced clinical disease. Eur J Cardiothorac Surg 2009;35:130-5. [Crossref] [PubMed]
- Kojori F, Chen R, Caldarone CA, et al. Outcomes of mitral valve replacement in children: a competing-risks analysis. J Thorac Cardiovasc Surg 2004;128:703-9. [Crossref] [PubMed]
- Horváth P, Hucin B, Slavik Z, et al. Operative treatment of infective endocarditis in children. Eur J Cardiothorac Surg 1989;3:26-32. [Crossref] [PubMed]
- Day MD, Gauvreau K, Shulman S, et al. Characteristics of children hospitalized with infective endocarditis. Circulation 2009;119:865-70. [Crossref] [PubMed]
- Beg A, Sadiq M. Subclinical valvulitis in children with acute rheumatic Fever. Pediatr Cardiol 2008;29:619-23. [Crossref] [PubMed]
- Cabell CH, Jollis JG, Peterson GE, et al. Changing patient characteristics and the effect on mortality in endocarditis. Arch Intern Med 2002;162:90-4. [Crossref] [PubMed]
- Geggel RL. Conditions leading to pediatric cardiology consultation in a tertiary academic hospital. Pediatrics 2004;114:e409-17. [Crossref] [PubMed]
- Coward K, Tucker N, Darville T. Infective endocarditis in Arkansan children from 1990 through 2002. Pediatr Infect Dis J 2003;22:1048-52. [Crossref] [PubMed]
- Alshammary A, Hervas-Malo M, Robinson JL. Pediatric infective endocarditis: has Staphylococcus aureus overtaken viridans group streptococci as the predominant etiological agent? Can J Infect Dis Med Microbiol 2008;19:63-8. [Crossref] [PubMed]
- Gutschik E. New developments in the treatment of infective endocarditis infective cardiovasculitis. Int J Antimicrob Agents 1999;13:79-92. [Crossref] [PubMed]
- Krcmery V, Gogová M, Ondrusová A, et al. Etiology and risk factors of 339 cases of infective endocarditis: report from a 10-year national prospective survey in the Slovak Republic. J Chemother 2003;15:579-83. [Crossref] [PubMed]
- Tariq M, Alam M, Munir G, et al. Infective endocarditis: a five-year experience at a tertiary care hospital in Pakistan. Int J Infect Dis 2004;8:163-70. [Crossref] [PubMed]
- Alexiou C, Langley SM, Monro JL. Surgery for infective valve endocarditis in children. Eur J Cardiothorac Surg 1999;16:653-9. [Crossref] [PubMed]


