Do arterial stiffness and wave reflections improve more with angiotensin receptor blockers than with other antihypertensive drug classes?
In their meta-analysis Chen and co-authors pooled together ten randomized controlled studies assessing the effect of angiotensin II receptors blockers (ARBs) on pulse wave velocity (PWV) and augmentation index (AIx), compared to a mix of other antihypertensive drugs (1). The authors documented that ARB treatment was as effective as dihydropyridine calcium channel blockers, beta-blockers and diuretics on PWV, whereas the effect on AIx was superior with ARBs. Authors deliberately settled to limit their systematic review to hypertensive patients with no co-morbidities, in order to avoid any external bias on the evaluation of treatment efficacy. They also decided to include in the meta-analysis only studies with a sufficiently long-term follow-up, in order to increase the chance of observing a significant treatment effect.
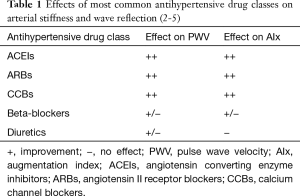
Previous meta-analyses have shown that antihypertensive agents of different classes may influence arterial stiffness and wave reflections to different extents, as summarized in Table 1 (2-5). The results of the meta-analysis of Chen and co-authors add to previous evidence by specifically focusing on ARBs’ effect and on AIx. The authors hypothesize that the superiority of ARBs for improving AIx may be explained by their effect on both vascular function and structure. It is well known that ARBs improve endothelial function and relax smooth muscle of the arteries (1). Vasodilation is not a specific property of ARB and is common to other antihypertensive drugs, which also improve arterial stiffening. In addition, ARBs contrast the profibrotic action of the renin-angiotensin system, reducing the collagen content of the arteries and attenuating extracellular matrix remodeling, and they may reverse smooth muscle hypertrophy, increasing arterial distensibility (6). Such mechanisms are plausible and they have been documented in a number of studies (4). Unfortunately, in their meta-analysis Chen and coworkers do not provide data on the pressor effect of the antihypertensive drugs at the brachial artery level, and even more so at the aortic (central) level. This is important, because it has been showed that, despite almost equivalent lowering of brachial blood pressure (BP), differences in the effects of different antihypertensive drug classes may be explained by a differential lowering of central BP, rather than pleiotropic mechanisms. This because different drug classes may have different vasodilator effects at the central level and this may result in a variable impact on wave reflection and thus on PWV and AIx. As a matter of fact, a recent meta-analysis showed that the placebo-adjusted central to brachial amplification is quantitatively different among different drug classes (2). In the meta-analysis, treatment with beta-blockers and diuretics resulted in significant changes in central to brachial amplification, whereas other drug classes, including ARBs and calcium channel blockers, had equivalent effects on central and brachial systolic BP. Treatment with beta-blockers was also associated with an increase in AIx, while the other classes reduced AIx to a similar extent. In the meta-analysis of Chen et al. the comparator was in most cases a calcium channel blocker for PWV and in most cases a beta-blocker for AIx. This might explain why the authors found that the ARB was superior to the comparators for improving the AIx, but not for PWV. Thus, it is important, when assessing the effect of the ARB on arterial stiffness and AIx to carefully consider the type of comparator and the pressor effect of the drug.
Full table
While acknowledging the importance of the results of the meta-analysis of Chen, some limitations require attention to interpret the findings appropriately.
There was a quite substantial heterogeneity of results among the studies, which was taken into account by using a random effect model in the presentation of the results. However, publication bias was not assessed or accounted for in the data analysis. Indeed, there were several possible sources of heterogeneity in the study. As correctly discussed by authors the comparators in the studies were quite heterogeneous, with a prevalence of dihydropyridine calcium channel blockers. Also the drug doses employed were quite unbalanced among studies, with some studies using low or moderately high dose, some others using high dose, and others adding a thiazide diuretic, a beta-blocker or a calcium channel blocker to the high dose monotherapy, in case of no response. We cannot exclude that the effect of treatment on both PWV and AIx could have been drug- and dose-dependent.
Assessment of PWV was made with different devices and techniques, and measurements were done at various sites along the arterial tree. Some studies estimated carotid-femoral PWV by pulsed Doppler technique, other studies measured brachial-ankle PWV by plethysmography, one study used transducers placed on the carotid, radial and femoral artery. Conversely to PWV, AIx was assessed in all studies with the same device, based on transfer function analysis of pulse waveforms obtained by applanation tonometry at the radial artery. It should be pointed out that although these and other numerous studies of antihypertensive agents have used noninvasive assessment of PWV and AIx, there are very few specific validation data for these techniques in the presence of antihypertensive drugs. Since it is expected that the accuracy in the evaluation of PWV and AIx may be largely device-dependent, the analysis should have accounted for such differences. In addition, no study actually compared PWV and AIx simultaneously collected in the same patients and thus differences due to subjective response could have been added to those due to the device used.
Some of the studies included in the meta-analysis of Chen and co-authors reported changes with treatment, others only values during treatment. Thus, it was difficult to perform a genuine pooled analysis of the different studies. Eventually, data were analyzed only by dividing the studies into two groups, this inevitably resulting in a drastically reduction in the power of the results. Study heterogeneity also extended to the length of follow-up, which was spread over a period ranging from 6 to 72 weeks, and to the patients’ characteristics. Concerning the possible influence of the length of treatment on vascular function, a recent individual meta-analysis of randomized controlled trials has documented a decrease in PWV of 1.30 m/s in long-term trials (average duration 2.5 months), which was larger than that observed for short-term trials lasting less than 1 week (0.75 m/s) (3). This meta-analysis also allowed to determine that the contribution of BP reduction to the improvement of PWV is negligible in long-term trials, whereas it is still relevant in case of short duration of treatment, supporting the hypothesis that the effect of long-term treatment with antihypertensive drugs may affect only in part the dynamic component of arterial stiffness, whereas the effect of the structural component may be predominant. The inclusion of studies with a short observation period in the meta-analysis of Chen and coauthors may have masked or blunted the effect of ARB treatment and prevented to show what has been previously shown (3), namely that arterial stiffness can be improved by antihypertensive treatment, independently of BP lowering.
Although in the study selection phase authors limited the inclusion to patients with arterial hypertension with no additional risk factors or co-morbidities, actually there was one study including type 2 diabetic patients and two studies including mostly or exclusively elderly patients. Since ageing and diabetes are associated with important vascular structural changes the impact of treatment in these patients could have been different compared to that in uncomplicated hypertensive patients.
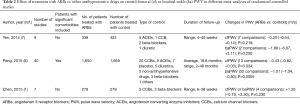
All these considerations are supported by two previous meta-analyses, which were specifically designed to assess the impact of ARB treatment on PWV. As shown in Table 2, Yen and coauthors also concluded that ARBs have a similar effect as other antihypertensive agents in reducing PWV (7). Similarly to the meta-analysis of Chen, the review was based on few studies (n=9), with a relatively long-term treatment (range 4 to 40 weeks), and excluded patients with significant co-morbidities. At variance from the meta-analysis of Chen, Yen and coworkers assessed the effect on arterial stiffness separately by carotid-femoral and brachial-ankle PWV. A more recent large meta-analysis of randomized trials comparing the ARB treatment with placebo or other types of drugs, showed a significant effect of ARBs on both carotid-femoral and brachial-ankle PWV (8). At variance from the meta-analyses of Yen (7) and Chen (1), this systematic review was based on a large number of studies (n=40), did not exclude patients with co-morbidities and was characterized by a long duration of the follow-up (18.8 months on average; range, 2–48 months).
Full table
In conclusion, the systematic review performed by Chen and coworkers represents a substantial step forward in the research of possible ancillary differences in the effect of antihypertensive drugs, particularly on vascular function. Nevertheless, the limited number and quality of papers selected for the meta-analysis and the high heterogeneity of the results, suggest that future large scale direct comparative randomized studies based on adequate drug doses and proper comparators should be designed and performed. Such studies should rely on the use of accurate and validated techniques. When different devices are used, one must be sure that measurements obtained are interchangeable.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Chen X, Huang B, Liu M, et al. Effects of different types of antihypertensive agents on arterial stiffness: a systematic review and meta-analysis of randomized controlled trials. J Thorac Dis 2015;7:2339-47. [PubMed]
- Manisty CH, Hughes AD. Meta-analysis of the comparative effects of different classes of antihypertensive agents on brachial and central systolic blood pressure, and augmentation index. Br J Clin Pharmacol 2013;75:79-92. [Crossref] [PubMed]
- Ong KT, Delerme S, Pannier B, et al. Aortic stiffness is reduced beyond blood pressure lowering by short-term and long-term antihypertensive treatment: a meta-analysis of individual data in 294 patients. J Hypertens 2011;29:1034-42. [Crossref] [PubMed]
- Janić M, Lunder M, Sabovič M. Arterial stiffness and cardiovascular therapy. Biomed Res Int 2014;2014:621437.
- Trudeau L. Central blood pressure as an index of antihypertensive control: determinants and potential value. Can J Cardiol 2014;30:S23-8. [Crossref] [PubMed]
- Struthers AD, MacDonald TM. Review of aldosterone- and angiotensin II-induced target organ damage and prevention. Cardiovasc Res 2004;61:663-70. [Crossref] [PubMed]
- Yen CH, Lai YH, Hung CL, et al. Angiotensin Receptor Blockades Effect on Peripheral Muscular and Central Aortic Arterial Stiffness: A Meta-Analysis of Randomized Controlled Trials and Systematic Review. Zhonghua Minguo Xin Zang Xue Hui Za Zhi 2014;30:98-107. [PubMed]
- Peng F, Pan H, Wang B, et al. The impact of angiotensin receptor blockers on arterial stiffness: a meta-analysis. Hypertens Res 2015;38:613-20. [Crossref] [PubMed]


