A case of long-term survival after multimodal local treatments of intramedullary spinal cord metastasis of squamous cell lung cancer
Introduction
Intramedullary spinal cord metastasis of non-small cell lung cancer is rare, and it has a short prognosis (1-3). As its clinical symptoms can be confused with other causes (4), brain and spinal cord magnetic resonance imaging (MRI) should be performed when neurological symptoms occur in patients with lung cancer. Regardless, there is no standard therapy. We describe a patient with intramedullary spinal cord metastasis of squamous cell lung cancer who survived for 25 months because of multimodal local treatments.
Case presentation
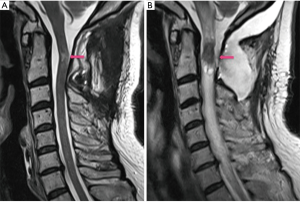
A 53-year-old man presented with a left pulmonary mass on chest radiography in August 2011. He was diagnosed with cT4N0M0, stage IIIA squamous cell lung cancer and underwent left pneumonectomy (pT4N0M0). After 10 months, he experienced a sensorimotor disorder of his left hand and had performance status 1. T2 weighted MRI showed a 2.5 cm intramedullary spinal cord tumor at the axis level (Figure 1), not in the brain. The intramedullary spinal cord tumor was resected (Figure 2A); the patient was diagnosed with metastatic squamous cell lung cancer. Although radiotherapy (30 Gy) and chemotherapy with carboplatin and gemcitabine were administered to treat the residual tumor, intramedullary spinal cord metastasis recurred locally 11 months after resection. Stereotactic radiotherapy was performed, and the tumor shrank again. After 5 months, another residual tumor developed locally, and the patient had performance status 2. Although his neurological deficit worsened, a second surgical treatment was successfully performed. Sequential chemotherapies, including docetaxel, nanoparticle albumin-bound paclitaxel, and S-1, were ineffective, and the tumor recurred (Figure 2B). After 25 months from the metastatic diagnosis, he died of respiratory arrest due to brain stem compression.

Discussion
The present patient’s clinical course suggests two important clinical issues. First, metastatic squamous cell lung cancer of the intramedullary spinal cord can be detected in patients with a good performance status. However, it can be overlooked because of the following reasons. Intramedullary spinal cord metastasis of lung cancer is rare with an incidence rate of 1.65% and that of squamous cell lung cancer is especially rare at 0.16% on autopsy (1). The prognosis of intramedullary spinal cord metastasis of non-small cell lung cancer is short at approximately 5 months (2) and 23.5 months at the longest (3). Lastly, the neurologic symptoms are often confused with brain metastasis, meningitis carcinomatosa, or the side effects of chemotherapy (4). Thus, clinicians should perform brain and spinal cord MRI when they observe neurological deficits during the clinical course of lung cancer.
Second, patients with metastatic squamous cell lung cancer of the intramedullary spinal cord may survive for long periods with multimodal local treatments. Surgical treatment of spinal intradural carcinoma metastasis may improve survival (5,6), and radiotherapy may contribute to improving survival (3,7,8). We performed multimodal local therapies because our patient had a good performance status and local recurrence with the risk of brain stem compression. Therefore, surgery, radiotherapy, or a combination of both should be performed whenever feasible. Chemotherapy may be effective for intramedullary spinal cord metastases of small cell lung cancer (9), and tyrosine kinase inhibitors (TKI) may be effective against metastases originating from TKI-sensitive adenocarcinoma (10,11). Chemotherapy can be poorly effective for intramedullary metastases with low drug permeability due to the blood-spinal cord barrier (12). In our case, chemotherapies were ineffective even after surgeries that were supposed to break the blood-spinal cord barrier. Treatment of intramedullary metastases may be related to drug permeability and the nature of the chemoresistance of squamous cell lung cancer. Yet, despite the neurological complication, surgical and radiological treatment reduced the tumor size and improved the patient’s survival.
Conclusions
This is a rare case of squamous cell lung cancer metastasizing to the intramedullary spinal cord, and our patient survived longer with multimodal local treatments.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Okamoto H, Shinkai T, Matsuno Y, et al. Intradural parenchymal involvement in the spinal subarachnoid space associated with primary lung cancer. Cancer 1993;72:2583-8. [Crossref] [PubMed]
- Conill C, Marruecos J, Verger E, et al. Clinical outcome in patients with intramedullary spinal cord metastases from lung cancer. Clin Transl Oncol 2007;9:172-6. [Crossref] [PubMed]
- Potti A, Abdel-Raheem M, Levitt R, et al. Intramedullary spinal cord metastases (ISCM) and non-small cell lung carcinoma (NSCLC): clinical patterns, diagnosis and therapeutic considerations. Lung Cancer 2001;31:319-23. [Crossref] [PubMed]
- Ishibashi Y, Tokuchi Y, Kamachi M, et al. A case of non-small-cell lung cancer with intramedullary spinal cord metastasis diagnosed pre-mortem. Nihon Kokyuki Gakkai Zasshi 2000;38:943-6. [PubMed]
- Dam-Hieu P, Seizeur R, Mineo JF, et al. Retrospective study of 19 patients with intramedullary spinal cord metastasis. Clin Neurol Neurosurg 2009;111:10-7. [Crossref] [PubMed]
- Kalayci M, Cağavi F, Gül S, et al. Intramedullary spinal cord metastases: diagnosis and treatment - an illustrated review. Acta Neurochir (Wien) 2004;146:1347-54; discussion 1354. [Crossref] [PubMed]
- Grem JL, Burgess J, Trump DL. Clinical features and natural history of intramedullary spinal cord metastasis. Cancer 1985;56:2305-14. [Crossref] [PubMed]
- Holoye P, Libnoch J, Cox J, et al. Spinal cord metastasis in small cell carcinoma of the lung. Int J Radiat Oncol Biol Phys 1984;10:349-56. [Crossref] [PubMed]
- Miura S, Kaira K, Kaira R, et al. The efficacy of amrubicin on central nervous system metastases originating from small-cell lung cancer: a case series of eight patients. Invest New Drugs 2015;33:755-60. [Crossref] [PubMed]
- Hata Y, Takai Y, Takahashi H, et al. Complete response of 7 years' duration after chemoradiotherapy followed by gefitinib in a patient with intramedullary spinal cord metastasis from lung adenocarcinoma. J Thorac Dis 2013;5:E65-7. [PubMed]
- Wagner M, Besse B, Balleyguier C, et al. Leptomeningeal and medullary response to second-line erlotinib in lung adenocarcinoma. J Thorac Oncol 2008;3:677-9. [Crossref] [PubMed]
- Gazzeri R, Galarza M, Neroni M, et al. Failure rates and complications of interspinous process decompression devices: a European multicenter study. Neurosurg Focus 2015;39:E14. [Crossref] [PubMed]


