A “reverse direction” technique of single-port left upper pulmonary resection
Introduction
In the past two decades video-assisted thoracoscopic surgery (VATS) has been performed with increasing frequency for lung cancer treatment (1). Since 2004, Rocco et al. published different articles about the single-port VATS approach (1). Single-port VATS left upper lobectomy is difficult amongst all the lobes (2). In 2011, Gonzalez et al reported the first single-port VATS left upper lobectomy (2). This report describes a new technique for single-port left upper lobectomy with the concept of “reverse-direction”.
Operative techniques
A 68-year-old male patient was admitted to our hospital for surgery of a left upper lobe mass. A computed tomography (CT) scan revealed a 4-cm mass in the upper lobe of the left lung (LUL). Bronchoscopy was normal. A positron emission tomography (PET) scan showed high uptake in the left upper mass with no lymph node involvement.
Under general anesthesia and single-lung ventilation, a VATS approach by 4 cm single-incision was done in the 4th intercostal space between the anterior axillary line and mid-axillary line, in a lateral position. The camera used was 10 mm HD scope 30 degree. No trocar is required. The wound protector is utilized. Incomplete fissure was detected. A mass was confirmed by digital palpation in the LUL too deep to perform a wedge resection. Instruments were long and curved with two (proximal and distal) articulations to allow the insertion of 3 or 4 instruments simultaneously. The surgeon and the cameraman stand in front of the patient. The camera was placed in the posterior part of the utility incision and the instruments were inserted in the anterior part.
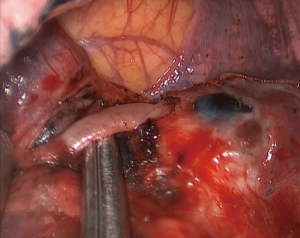
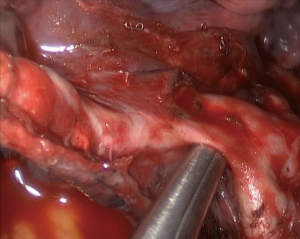
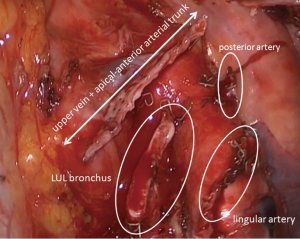
Optimal traction of the upper lobe to anterior was necessary in order to achieve an adequate exposure of the arterial branches of the pulmonary artery. The posterior artery was exposed and divided with a stapler which had been inserted through the anterior part of the incision (Figure 1). The next step was stapling the fissure from anterior to posterior. The lingular artery was then dissected and divided by a stapler (Figure 2).
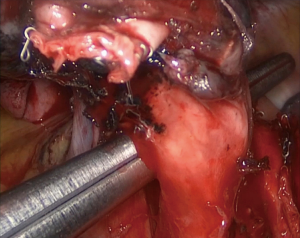
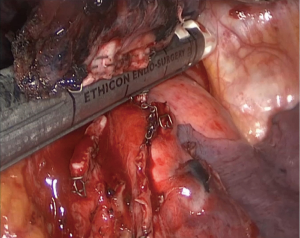
We continued the procedure by dissecting and stapling the bronchus of the LUL (Figure 3). Once the previous arterial branches are stapled, the bronchus is easily exposed. Dissection and stapling of the upper vein and apical-anterior arterial trunk was the last step and can be done together (Figures 4,5). Since the bronchus and arterial branches are stapled, the optimal angulation for the upper vein and apical-anterior arterial trunk can be easily achieved by staplers (Figure 6). The specimen was finally removed in a protective bag. Systematic lymph node dissection of the subcarinal, aorto-pulmonary window and prevascular space finished the procedure. A single chest tube was placed in the posterior part of the utility incision.

Comments
Single-port left upper lobectomy is difficult (4). The location of the pulmonary artery in relation with the branching pattern of the left pulmonary artery and the aorta increases the difficulty of the procedure. At the beginning of single-port lobectomies, the upper lobes were believed not to be amenable for single-port approach due to the difficult angulation for staplers. Gonzalez-Rivas reported the first single-port left upper lobectomy in 2011 (2) and his operative procedures quickly became the mainstream surgical method for single-port LUL, which is similar to conventional VATS with the upper lobe apical-anterior arterial trunk divided first to facilitate the division of the upper lobe vein. Sectioning first the apical-anterior arterial trunk helps the access with the aid of staplers to the upper vein, which is the most uncomfortable structure to reach with staplers in single-port left upper lobectomies.
The current practice mentioned above is repeatable and effective; however, the dissection of apical-anterior arterial trunk remained as the most challenging part during operation because care must be taken with pulmonary artery which lies posterior. The pulmonary artery should be carefully protected. Injuries to pulmonary artery could be disastrous and usually requires the conversion to multi-port or open surgery.
Contrary to the current practice, we divide the apical-anterior arterial trunk with upper vein in the last. The procedure sequence is described as follows: posterior artery, lingular artery, bronchus and finally upper vein & apical-anterior arterial trunk. It mostly starts from posterior, which is reverse to the current practice. This method could overcome the angular limitations frequently encountered in single-port VATS procedures; reduce the risk of injuries to pulmonary artery. Additionally, it is not necessary to dissociate pulmonary arteries within the hypoplastic lung fissure because in the last step of this procedure, it is easy to remove the lung fissure with a cutting stapler after the bronchus and vessels have already been dissected. This means the new technique could potentially broaden the indications of single-port LUL to include hypoplastic lung fissures.
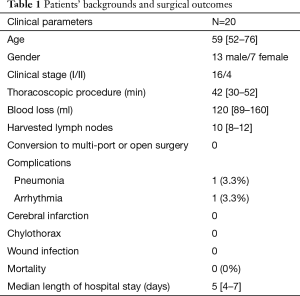
Literatures surrounding the practice of single-port LUL are quite limited. This “reverse direction” technique is not reported. We have performed 20 surgeries by this new sequence (Table 1) in our center and it was proved to be repeatable, safe and effective in practice. Limitations of this new practice are similar to that of multiple-port surgery, such as the enlargement or severe calcifications of hilar and bronchial lymph nodes. In our series, most patients are in their early stage (16 in stage I and 4 in stage II) (Table 1); the lymph node dissection was relatively easy. Recently, we have performed several cases with severe enlargement of bronchial lymph nodes. Our experience is to place the camera in the upper part of the incision and insert 3 or 4 instruments below the camera to complete the systematic dissection. It is helpful to insert two 10 mm endopeanuts in the lower part of the incision to retract the aorta, esophagus and lung. This operation facilitates the dissection with instruments placed above the peanuts and below the camera.
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflict of interest to declare.
Informed consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg 2011;13:539-41. [Crossref] [PubMed]
- Zhang M, Sihoe AD, Du M. Surgical procedure of uniportal LUL. Asvide 2016;3:336. Available online: http://www.asvide.com/articles/1105
- Sawada S, Komori E, Yamashita M. Evaluation of video-assisted thoracoscopic surgery lobectomy requiring emergency conversion to thoracotomy. Eur J Cardiothorac Surg 2009;36:487-90. [Crossref] [PubMed]