Mycotic aortic arch aneurysm coexistent with constrictive pericarditis: is surgery a dangerous resort?
Introduction
Salmonella infection is an etiology of multiple cardiovascular complications, one of which being mycotic aneurysm of the aorta. However, constrictive pericarditis, either isolated or coexistent, is rarely seen associated with Salmonella infection, and represents a surgical challenge. We report a case of mycotic aneurysm of the aortic arch together with constrictive pericarditis successfully treated by combined open and endovascular surgery with satisfactory outcome and minimal morbidity.
Case presentation
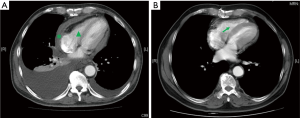
A 68-year-old man presented with fever, chest pain, anaemia and deranged liver function. Investigations were unremarkable except a positive Widal’s test. Contrast computer tomography (CT) scan of thorax revealed pericardial effusion with diffusely thickened pericardium especially anterior to the right ventricle, causing significant reduction in right ventricular volume, and a 4.5 cm partially-thrombosed aneurysm arising from lateral wall of aortic arch, with the aneurysm neck of around 1.5 cm at the aortic arch. Echocardiogram revealed delayed relaxation of ventricles during diastole, with normal valves and left ventricular ejection fraction.
In view of constrictive pericarditis and a suspected mycotic aneurysm of the aortic arch, it was decided to perform an open pericardiectomy and aortic debranching under cardiopulmonary bypass. The patient was cannulated with right atrial-venous 2-stage cannulation and right femoral arterial cannulation. Intra-operatively the pericardium was noted to have burn-out inflammation with complete symphysis within the pericardial space. After total pericardiectomy from phrenic to phrenic and from the aortic arch to diaphragm level, it was discovered that the aortic arch was diving deep down to the posterior mediastinum. Despite careful dissection of the arch vessels, they are very densely adherent to the left inferior aspect of the aortic arch, with poor visualization of the left common carotid artery. An aorto-brachiocephalic bypass (size 9 PTFE graft) was performed in preparation of a second-stage thoracic endovascular aortic repair (TEVAR). Aortic side clamp was applied and a 9 mm HEMASHIELD™ (Maquet, Rastatt, Germany) graft was anastomosed to the ascending aorta with 5-0 polypropylene. Right brachiocephalic artery was transected after proximal and distal clamping, followed by end-to-end anastomosis between the graft and right brachiocephalic artery. The stump of the brachiocephalic artery was oversewn with two layers of 4-0 polypropylene and reinforced with 4-0 pledget felt stitch. The total operative time of the first operation was 260 minutes.
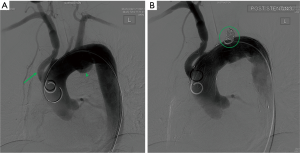
The second stage operation was performed 1 week later under general anaesthesia. Carotid-carotid bypass was constructed, via bilateral anterior neck incision, using a 6-mm EXXCEL™ (Maquet, Rastatt, Germany) soft thin-wall ePTFE vascular graft. Then the left femoral artery was cannulated with a 5 Fr sheath, followed by passage of a 4 Fr pigtail catheter via guidewire. The position of arch aneurysm was confirmed with digital subtraction aortogram. One RELAY Plus® (Bolton, Sunrise, Florida, USA) thoracic stent graft (40 mm × 195 mm) was passed to the ascending aorta via the guidewire. The stent was deployed with the proximal landing just distal to the aorto-brachiocephalic bypass (zone 0 stenting). Completion aortogram confirmed that the arch aneurysm was satisfactorily excluded by the stent graft. Then a 4 Fr MPA (Beacon® Tip Torcon NB® Advantage, Cook®, Bloomington, Indiana, USA) catheter was passed to the proximal left subclavian artery via left brachial artery cannulation over Terumo® (Somerset, New Jersey, USA) guidewire. The left subclavian artery was embolized at the origin using Nester® (Cook®, Bloomington, Indiana, USA) embolization coil. Completion aortogram showed satisfactory exclusion of the aneurysm (Figure 1A,B). The total operative time of the second operation was 225 minutes.
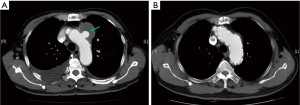
Post-operatively patient did not show any distal circulation or neurological abnormalities. Intravenous ceftriaxone was completed for a total 8-week course, followed by lifelong oral co-trimoxazole. C-reactive protein gradually normalized. Pathology of the excised pericardium showed only fibrosis with no evidence of organism growth. He remained well 2 years after the operation. Follow-up CT scan at 18 months after the operation showed resolution of the arch aneurysm with no evidence of endoleaks or fistulation (Figure 2A,B), and complete restoration of the filling of the right ventricle (Figure 3A,B).
Discussion
Salmonella infection is a well-known causation of mycotic aneurysm of the thoracic aorta (1). Nevertheless, the infection is rarely associated with constrictive pericarditis (2). The coexistence of the two conditions has never been reported in the English literature, and our patient represents the first one.
Pericardiectomy against severe pericardial adhesion as a result of burnout pericarditis was expected to carry high operative mortality (30-day mortality up to 18.6%) (3,4). Pre-existing ventricular function impairment, increased blood loss from raw areas after meticulous tissue dissection need of cardiopulmonary bypass, and distorted anatomy of the great vessels rendered the subsequent total arch replacement surgery a huge technical challenge. Despite all these, there was still an alternative way for treatment using the hybrid approach (5). Though not yet proven to be superior to total arch replacement, its safety and feasibility were well shown for mycotic aneurysm of the aorta in the literature (6,7), and our treatment for this patient also demonstrated these. Additionally, the avoidance of deep hypothermic circulatory arrest in times of sepsis reduces the risk of profound systemic inflammatory response syndrome (SIRS), and thus reduces surgical mortality and morbidity.
Successful treatment requires, aside from surgical expertise, comprehensive preoperative planning and prediction of unexpected situations which may warrant an immediate change in the treatment approach. In our case, once it was discovered that a total arch replacement was technically impossible, an endovascular alternative was immediately indicated. However, this was not possible in the setting of conventional operating rooms with no devices and facilities for vascular access and image guidance. The use of hybrid operation theatre would be beneficial under the circumstances in that it allowed the change of surgical approach to the “backup plan” at once, without the need of staged procedures which subjects the patient to a second general anaesthesia and its associated risks.
We conclude that, in time of a mycotic aneurysm of the aortic arch, coexistence with constrictive pericarditis should not be considered as a contraindication to aggressive surgical treatment. Staged hybrid aortic arch repair is shown, from our case, safe and feasible, avoiding the need of deep hypothermic circulatory arrest in times of sepsis, and thus its increased risk of profound SIRS, mortality and morbidities.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Hsu RB, Lin FY. Infected aneurysm of the thoracic aorta. J Vasc Surg 2008;47:270-6. [Crossref] [PubMed]
- Doig JC, Hilton CJ, Reid DS. Salmonella: a rare cause of subacute effusive-constrictive pericarditis. Br Heart J 1991;65:296-7. [Crossref] [PubMed]
- Vistarini N, Chen C, Mazine A, et al. Pericardiectomy for Constrictive Pericarditis: 20 Years of Experience at the Montreal Heart Institute. Ann Thorac Surg 2015;100:107-13. [Crossref] [PubMed]
- Busch C, Penov K, Amorim PA, et al. Risk factors for mortality after pericardiectomy for chronic constrictive pericarditis in a large single-centre cohort. Eur J Cardiothorac Surg 2015;48:e110-6. [PubMed]
- Lao WF, Huang CH, Lin CH, et al. Endovascular stent graft repair for a Salmonella-infected aneurysm of thoracic aorta. Ann Vasc Surg 2012;26:731.e5-8. [Crossref] [PubMed]
- Yu SY, Lee CH, Hsieh HC, et al. Treatment of primary infected aortic aneurysm without aortic resection. J Vasc Surg 2012;56:943-50. [Crossref] [PubMed]
- Kritpracha B, Premprabha D, Sungsiri J, et al. Endovascular therapy for infected aortic aneurysms. J Vasc Surg 2011;54:1259-65; discussion 1265. [Crossref] [PubMed]


