A survey among Brazilian thoracic surgeons about the use of preoperative 2D and 3D images
Introduction
Preoperative planning is critical and has an influence on surgical outcomes (1). It is done mainly by the use of tomographic images computed in thoracic surgery (2). The use of 2D axial images computerized is routine in clinical practice. New forms of medical information display as 3D volumetric (reconstructed from computed tomography (CT) of the chest on devices with multidetector) can facilitate this planning; improve intra-operative results, thus influencing the final surgical outcomes (3-5).
Therefore, it would be significant to know the reality of the Brazilian Thoracic surgeon as your needs as an end user of the medical information contained in 2D and 3D tomographic images. The notion of the importance of images based surgical planning and the reasons for non-routine use of these new computational tools in their clinical practice would be additional data (6). It is, therefore, rational for a research project to assess how the Brazilian thoracic surgeons, linked to private university hospitals or clinics, manage and manipulate tomographic medical imaging and evaluated the logical process of current preoperative surgical planning using 2D medical images generated by CT scan, and what impact the use of interactive 3D graphics models. Thus, the objectives of this study were: (I) describe the characteristics of how the Brazilian Thoracic surgeon uses the 2D/3D medical imaging to perform surgical planning, clinical practice and teaching in thoracic surgery; and (II) check the initial choice and the final selection of the Brazilian Thoracic surgeon as the 2D and 3D models pictures before and after acquiring theoretical knowledge on the generation, manipulation and interactivity of 3D views.
Methods
The Research Ethics Committee approved the study at the Hospital das Clinicas, Ribeirão Preto School of Medicine, University of São Paulo. A detailed cross-type Survey to data provided by the Brazilian Thoracic Surgeons (members of the Brazilian Society of Thoracic Surgery) who responded to a multimedia online questionnaire via the internet on their computers or personal devices.
A data collection instrument was developed a multimedia online questionnaire consisting of 33 questions grouped into five sections: section #1, “preoperative planning”; section #2, “2D–3D imaging and medical information display”; section #3, “2D vs. 3D images”; section #4, “additional data”; section #5, “demographics”.
The survey is available at http://survey2d3d-convidados.questionpro.com, and in Figure 1 is represented one example of the questionnaire. It was completed on a voluntary basis, and all participating physicians agreed with the informed consent and informed presented as the initial question in the survey.
We used the OsiriX software (version 5.9 32-bit; Pixmeo SARL, Bernex, Switzerland) for handling and preparation of 3D models as well as to export animations in video file format (MPEG). Videos containing animations of the 3D model and videos created to demonstrate the use of an image processing program (Osirix) were made using Camtasia software (version 2.8.2; TechSmith, Okemos, MI, USA). This software allows, besides editing the video files, the computer screen recording in real time, thus facilitating the creation of educational videos and training.
They used rented Internet services to store web questionnaire and allow its electronic distribution. QuestionPro platform web was used for this distribution (QuestionPro Survey Software, Seattle, WA, USA). Also illustrative surgical videos questionnaires were allocated to another internet server, ensuring their availability in the event of failure of the first, Screencast.com platform (TechSmith, Okemos, MI, USA).
Data analysis
The database was structured using building a dictionary, data spreadsheet software, for encoding of the variables. Next, the data were processed using the GraphPad Prism software (version 6.0; GraphPad Software Inc., San Diego, CA, USA), enabling the realization of descriptive and comparative statistics and the preparation of tables and graphs. Results for categorical variables (diagnosis, disease extension evaluation, surgical planning preoperative, communication between physicians, training of residents, graduate education and explanation of the patient) were presented as absolute values and in the form of proportion. We used the chi-square test for independent samples to compare the preference groups 2D, 3D or 2D + 3D. A level of P<0.05 was considered indicative of statistical significance.
Results
Demographic sample data
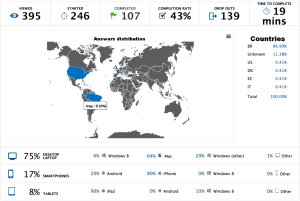
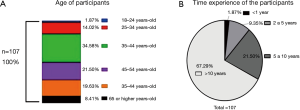
Of the 395 invitations distributed by e-mail received and viewed by thoracic surgeons SBCT, 246 doctors have begun the process of answering the questionnaire. Those who started, 107 physicians completeted the entire questionnaire with response rates of 43%.
The average time for completion of all the answers to the questionnaire was 19 minutes per questionnaire. Medical responders, 75% used personal computers; smartphones 17% and 8% used tablets.
Demographically, the management system for Internet questionnaires for the application reported the locations (country) of origin of the responses, this information together with the above are shown in Figure 2. The distributions of respondents by age and by the time the experiment are presented in Figure 3.
Evaluation of 2D and 3D images—surgeon preference at three times the questionnaire
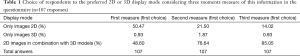
Regarding the type or display mode tomographic image (2D and/or 3D image) routinely used by surgeons in clinical practice and that preferred by the surgeon during the process of questionnaire answers, it was agreed and asked if the interviewee, the preference for 2D and/or 3D images in two stages of the process, called “2D–3D initial preference” and “2D–3D preferred end”, respectively.
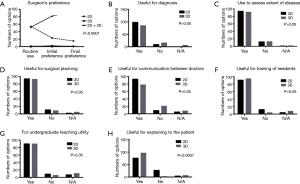
The data obtained are shown in Table 1 for information capture three times the “2D–3D preference of the surgeon”, using the same question and answer format the same. There was a significant change in the final preferred choice for 3D models used together with the 2D images (P<0.0001) as shown in Figure 4A.
Full table
Comparison of 2D and 3D images for specific applications
Comparing the 2D vs. 3D models pictures for various applications, we asked the surgeon interviewed the information that the 2D and 3D images provide enough information for (I) diagnosis, (II) assessment of the extent of the disease, (III) preoperative surgical planning, (IV) communication between doctors, (V) training of residents, (VI) the medical undergraduate education and (VII) explanation to the patient.
The results for each of the seven aforementioned applications are presented, comparing the choice of surgeons for 2D and 3D images in Figure 4B (useful for diagnostics), Figure 4C (usefulness to assess extent of disease), Figure 4D (useful for surgical planning), Figure 4E (utility for communication between doctors) Figure 4F (helpful for training of residents), Figure 4G (for undergraduate teaching utility) and Figure 4H (useful for explaining to the patient).
The analysis of comparisons “utilities 2D vs. 3D” no significant difference for diagnostic purposes, assessment of the extent of disease, preoperative surgical planning, communication among physicians, residents and training of undergraduate medical education. Only the analysis of the usefulness of “explanation to the patient” showed statistical significance for 3D images on the choice of the surgeon (P<0.0001).
Evaluation of 2D and 3D surgical video
The first video of the questionnaire demonstrates concepts of imaging and applications of 2D images. The video is available in: http://www.screencast.com/t/dp9tRFdvtEH. The results for the choice of surgeons when the respondent answers the usefulness of the 2D images in the clinic immediately after the video display are shown in Figure 5A.

The second video shows the questionnaire concepts and imaging applications of 3D images. The video is available at http://www.screencast.com/t/hbqPkzq0W4V. The results found when the respondent selects the utility of 3D images to clinical practice, after the video display, are shown in Figure 5B.
The third video of the questionnaire demonstrated concepts and navigation modes for 2D images (sequentially “scrolling”) and the 3D images (interactively with 3D mouse). The video is available at http://www.screencast.com/t/TIrwCx2HafQl. The results found when the respondent chooses the preferred display mode and interaction with the images, after viewing the video, are shown in Figure 5C.
Discussion
Advances in medical imaging since 1970, have open borders huge for clinical diagnosis. The computer, the digital radiologic technology, and new imaging techniques significantly expanded the possibilities for an accurate preview, and noninvasive, providing an accurate measurement of the morphology and function of organs and body systems (5).
In the last two decades the technological evolution of diagnostic imaging, based on digital technology, occurred at a remarkable speed to the point of compromising their adoption in clinical practice.
This is so true that one of the initial ideas of our research includes the transition from traditional radiography (Rx) to conventional CT and, finally, the evolution of 2D and 3D images. However, since the initial outline of the construction of the questionnaire revealed that the research would become a “never-ending story”. For this reason, it was decided to adopt the current situation that is the evolution of technology 2D to 3D. Therefore, to broaden the spread and improvement of new 3D visualization techniques was born the proposal of a detailed survey of Brazilian thoracic surgeons, end users tomographic medical information to assess the current use of 2D images 3D models in their routine surgical practice.
The man has always bothered to register signs and has been so since the rock records in prehistoric images. The records created, regardless of their purpose at any given time will be assessed, constituting one of the best forms of human communication. All produced image will appear at some point and with some purpose (7).
The view can be understood as the formation of visual mental images. The view is the primary way to interpret the vast amount of data generated, for example, a current tomography apparatus. When an observer sees a particular image, it creates a new mental model and compares it with pre-existing models in its personal memory.
For complex data or a lot of images, build a mental model requires interaction and time since all data cannot be evaluated in a single view. Again, for the example of CT scan of the chest, is estimated to be generated, on average, 400 axial images per examination, which should be examined conventionally 2D sequential format by the evaluator.
New and advanced visualization tools can help users to update and refine their mental models, as close to the real world. They should preferably be easy to use and does not require sophisticated computer skills or the users (8).
There are several lines of studies that try to understand how human beings perceive the world through their sensory system. For this study, the important thing here, to the context of our research is how humans interact with the computer, whereas the medical use almost invariably, a personal computer video monitor to evaluate the tomographic medical imaging and perform medical decision-making.
This approach, given the man-machine interaction, will develop new visualization modalities of medical information (such as virtual 3D models), and also, design interfaces that allow the user of a computer system receiving the information, store them in memory (human) and “processing” them, using inductive and deductive reasoning. And finally, contribute to the formation of their personal bank mental picture templates (9).
The cornerstone of image-based visualization is the extraordinary ability of the human visual system to analyze the data. However, considering the explosion of generated medical images, this ability may be impaired.
The information visualization, a new specialty in growing expansion, aims to reduce the complexity of the analysis and understanding of information for physicians through interaction. Search visually present medical data in a more intuitive, easy to understand, learn, and recognize, in addition to navigation in interactive computing environments (10). On the other hand, also seeks to prevent information overload and allow members of a clinical team dominate larger amounts of medical information.
The above and taking into account the proposal of our research, to introduce new forms of 3D visualization of medical images, the concept of information visualization is the theoretical basis of our study. The preoperative planning is of relevance and influence on surgical outcomes. It is performed routinely using 2D images in thoracic surgery (11). However, as published in other surgical specialties, new forms of medical information display using reconstructions 3D models can facilitate this planning and thus improve the intraoperative results, benefiting end-surgical results (12).
Considering the broad topic addressed in this study, delimited to the question of research to the study of 3D images for the purpose of surgical planning, and that guided the design and manufacture of the survey instrument, illustrated questionnaire with pictures and demonstration videos.
Initially, it is important to mention the difficulties encountered and the time used to select applications (software) and learn how to use them, as well as internet tools for implementation and management of questionnaires.
The acquisition of computer skills and programming was crucial, both for the construction of the questionnaire with images and graphic videos, as to the correct management of the questionnaires internet platform. It was believed that the effort would result in a highly interactive and attractive material for the user, shown by the final evaluation of the highly satisfactory questionnaire.
Develop animations of demonstration videos format require a lot of time, dedication, and patience. Countless hours of work were devoted to every minute of animation, not including processing time taken by the computer. It was found that the computational platform adopted adequately fulfilled purposes. Therefore, with a system based on personal computer and the appropriately selected programs, the development objectives and the questionnaires were well executed (13).
The domain knowledge of the content to be explored is the critical point in the elaboration of an animation, because it cannot contain misconceptions. The comprehensive conceptual discussion was always the most important issue in the development of videos with animations and the questionnaire itself, because, in addition to reducing the time the production phase, resulted in videos free of conceptual errors, considered essential for the transmission of new knowledge the doctors interviewed.
The initial planning of the questionnaire also involved the choice of subjects covered for which the demonstration videos with 2D and 3D views would be developed. Exploring their applications in thoracic surgery, demonstrating concepts of imaging and producing an interactive format suitable for publication of questionnaires on the Internet platform.
Still on the initial design of the questionnaire design, we tried to follow some guidelines to make it more representative and measurable (14). The questionnaires were developed using the Likert scale. This level seeks to identify the consent of the researched about information submitted and, at the same time avoiding distortions in the answers. Specifically, this study we used the 5-point scale in some questions and the other 10 points range.
He tried to match the questions to avoid distortions and conflicts in their chosen answers. Most of the questions were closed with unique responses to categorize them actually and, if necessary, an open “other” category was used to allow respondents to specify details.
Few questions allowed entry texts in free-form (open questions) arranged at the end of the questionnaire. A good portion of the questions was also illustrated with tomographic reconstructions 2D and 3D images.
In the questionnaire preparation was arbitrated the five levels of care already mentioned. Perhaps the most active stage of the project, where the maturation of the final objectives of the research and gain knowledge in programming tools, culminating in the production of a questionnaire, illustrated with pictures and videos specifically built in an interactive format and applied internet platform.
Section #01 (preoperative planning) aimed to evaluate and describe the clinical practice and the evaluation of flow (workflow) of the thoracic surgeon using medical images. In addition to the preoperative planning, were registered opinions on the importance of 2D and 3D images for surgical planning? He tried also to obtain information about the available resources and devices used for evaluation of the images. Questions about the importance and satisfaction of the radiological report finished this section.
Section #02 (2D imaging/3D and medical information display) aimed at evaluating the level of knowledge of the interviewee about 2D and 3D imaging and visualization of the delivery of medical information. Research deepened to discover possible experiences related to the acquisition, generation and interactive manipulation of 3D models using dedicated software.
Section #03 (2D vs. 3D comparison) used demo videos showing 2D and 3D views for clinical practice. After instruction phase and gain knowledge of using the videos like a real educational resource, the respondent would be able to relate impressions, although subjective, comparing the two forms of medical information visualization. At this point, the question called “surgeon preference evaluation by images 2D and or 3D” is displayed for the third time, i.e., after the display concepts being presented even for those who were unaware.
Also in this section, we discuss some information, including:
- The frequency of 2D and 3D images used in clinical practice;
- The reason for the lack of use of these computational tools 3D views;
- The comparative utility of 2D and 3D images to defined applications such as diagnosis, the extent of disease, surgical planning, communication among physicians, resident training, education in medical teaching and communication with the patient.
Section #04 (additional information and concluding remarks) aimed a peer review evaluation of the research, including a free text field for shows and personal opinions.
Finally, Section #05 (demographic information) collected profile data of respondents such as age, length of experience, workplaces, and medical specialty.
Some comments were selected to be included in this discussion because they represent a real “peer review” and reflect the impact of research. These observations, no doubt, “speak for themselves”.
“..great model. If it were leaner, could be used routinely..”.
“As for the question about image viewer preference, I think that there might be an item with the option: ‘I prefer to use because I have no experience with 2D images image/3D image use’. I suggest this modification because choose this response if it was available (an option which was offered only after viewing all videos). Also, could be indicated by clinical participant some 3D software for visualization of medical images at the end of the survey”.
“Some issues did not allow a standard response to the fact that using CT in 3D, in particular, situations and not a routine. In selected cases CT in 3D is a great help”.
“I liked the idea, found it fascinating and educational. Everything worked fine. I think some questions elicit some response and will be difficult to completion (few). In question 23 I was not sure about the alternatives 3:05, I think they are very close, and I could not see a significant difference in time to select them. I think the educational point of view this research is phenomenal and worth maybe in the future to evaluate the academic potential of such questionnaires. And the academic potential already has a conclusion. I think the researcher would need to be identified to have possibly other questions in the future”.
“I find it necessary to discuss with the radiologist, also in selected cases in which he can do other reconstructions and ask questions. I would stress that we are not all radiologists, and indeed, the view of an expert is usually more accurate”.
“Chest images are central to the planning of procedures and follow-up treatments. Another primary interest is in medical school graduate and residency. In addition to the CT, key images for the practice of a specialist in thoracic surgery, I believe that the conventional radiographic images, or even in the digital system, should not be forgotten because they are still part of the reality of our country”.
“I think the image and totally underused in our specialty, much due to the heterogeneity of devices, but mainly by the lack of access to programs such as Osirix for example, by most professionals”.
“I believe that everything you add to define the best surgical approach preoperatively, especially with the consecration of minimally invasive surgery to extended resections, only has to contribute and add in our daily practice”.
“I would like to congratulate the organizer of this research. As always it is a stimulator of new techniques especially those relating to information technology as improvement method, encouraging update and consequently an improvement in service to our patients. To that currently, for various reasons, have turned away from teaching hospitals but believe in private medicine as essential to people in their most different levels, there can be no exclusivity in medicine “tip” only those who have access to said teaching hospitals”.
“I have observed over the past 5 years, the uses of 3D images are very useful for diagnosis of superior sulcus tumors, subclavian vessels invasion, brachial plexus, and particularly Giant tumors of the chest wall, as desmoids infiltrating under the scapula. It has also proven useful in lung transplantation in Kartagener syndrome with bilateral bronchiectasis for selection of arterial and bronchial gauges since most of these patients have suffered stunted lobectomy. I have however observed that in bone lesions of the chest wall (osteolytic lesions of the ribs, sternum, and vertebrae) the method underestimates the radial limits of the injuries. Perhaps it is necessary to improve the software. Already I extirped osteochondrosarcomas and osteosarcomas sternum and ribs guided by 3D, and the margins were compromised, although the 3D CT did not show up”.
“I found it interesting because although the topic is important, some of us surgeons do not have the time or willingness to learn about thoracic radiology and this research can be a trigger for this type of learning”.
“Medical images generated by filters for the 3D structure analysis usually produce artifacts that make them unreliable for the assessment of disease extent and limits. Exceptions to the analysis of ribs in multislice devices, demonstrating excellent images for injury analysis”.
Doctors have years of experience in the use of images based on X-ray films and CT axial and, therefore; have a profoundly entrenched reference in the 2D images to their clinical reasoning and the practice of surgical planning.
The continuous evolution of 3D visualization and promises to expand scientific exploration and increase research. The knowledge of reality and the profile of end users may contribute significantly to this new display technologies incorporation process. However, the inclusion of a new tool in the doctor’s work routine will require a transition period, when new methods are gradually included, and compared with conventional methods as the advantages and disadvantages of its implementation.
The use of new techniques does not necessarily mean improving the quality of the resulting work; other related factors such as the method of labor and the training of human resources for the efficient use of the software are also key.
The positive results of this study reflect the growing evidence that the 3D visualization and interactive analysis of medical images are the bridge from theory to practice and the computer lab to the operating room. Showing also that a paradigm shift in vision, 2D, and 3D views are complementary and not antagonistic.
Conclusions
The major findings of this study, to end the discussion and that answer the objectives of the survey were:
- There were no statistical differences when compared to 2D images vs. 3D models for the following purposes: diagnosis, assessment of extent of disease, preoperative surgical planning, communication among physicians, residents and training of undergraduate medical education;
- After the completed questionnaire responses was no significant change in the final choice of thoracic surgeons for the 3D models used in conjunction with the 2D images.
Study limitations
Although by applicable a suitably structured questionnaire and to include an assessment of the default preference of the surgeon concerning 2D images and 3D using video demonstration and educational character, developed research presents major limitations of a descriptive exploratory study type survey.
Clinical validation of 3D visualization protocols in thoracic surgery, not just for surgical planning, but also as a diagnostic contribution, should be conducted. On the other hand, well-structured data obtained and produced by this investigation should properly drive the design of the validation protocols medical application of virtual 3D visualization models.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Post-graduation Committee of the Department of Surgery and Anatomy. It is a PhD thesis based on a survey that did not involve patients.
References
- Graves ML. The value of preoperative planning. J Orthop Trauma 2013;27 Suppl 1:S30-4. [Crossref] [PubMed]
- Kanzaki M, Kikkawa T, Shimizu T, et al. Presurgical planning using a three-dimensional pulmonary model of the actual anatomy of patient with primary lung cancer. Thorac Cardiovasc Surg 2013;61:144-50. [Crossref] [PubMed]
- Eggebrecht H, Pamler R, Zipfel B, et al. Thoracic aorta endografts: variations in practice among medical specialists. Catheter Cardiovasc Interv 2006;68:843-52. [Crossref] [PubMed]
- Akiba T. Utility of three-dimensional computed tomography in general thoracic surgery. Gen Thorac Cardiovasc Surg 2013;61:676-84. [Crossref] [PubMed]
- Pommert A, Höhne KH, Burmester E, et al. Computer-based anatomy a prerequisite for computer-assisted radiology and surgery. Acad Radiol 2006;13:104-12. [Crossref] [PubMed]
- Ikeda N, Yoshimura A, Hagiwara M, et al. Three dimensional computed tomography lung modeling is useful in simulation and navigation of lung cancer surgery. Ann Thorac Cardiovasc Surg 2013;19:1-5. [Crossref] [PubMed]
- Tory M, Möller T. Human factors in visualization research. IEEE Trans Vis Comput Graph 2004;10:72-84. [Crossref] [PubMed]
- Udupa JK, Tian J, Hemmy DC, et al. A Pentium personal computer-based craniofacial three-dimensional imaging and analysis system. J Craniofac Surg 1997;8:333-9. [Crossref] [PubMed]
- Groesel M, Gfoehler M, Peham C. Alternative solution of virtual biomodeling based on CT-scans. J Biomech 2009;42:2006-9. [Crossref] [PubMed]
- Chittaro L. Information visualization and its application to medicine. Artif Intell Med. 2001;22:81-8. [Crossref] [PubMed]
- Hemminger BM, Molina PL, Egan TM, et al. Assessment of real-time 3D visualization for cardiothoracic diagnostic evaluation and surgery planning. J Digit Imaging 2005;18:145-53. [Crossref] [PubMed]
- Alder ME, Deahl ST, Matteson SR. Clinical usefulness of two-dimensional reformatted and three-dimensionally rendered computerized tomographic images: literature review and a survey of surgeons' opinions. J Oral Maxillofac Surg 1995;53:375-86. [Crossref] [PubMed]
- McGhee J. 3-D visualization and animation technologies in anatomical imaging. J Anat 2010;216:264-70. [Crossref] [PubMed]
- Patel A, Edwards R, Chandramohan S. Surveillance of patients post-endovascular abdominal aortic aneurysm repair (EVAR). A web-based survey of practice in the UK. Clin Radiol 2013;68:580-7. [Crossref] [PubMed]


