Atrial fibrillation post coronary artery bypass surgery: is there still a role for perioperative statins after STICS?
Atrial fibrillation (AF) is a common arrhythmia after coronary artery bypass grafting (CABG). It is estimated to occur in about one-third of the patients post-CABG (1-3). In a prospective observational study of 1,878 consecutive patients undergoing CABG, post-CABG AF was associated with a four-fold increased risk of disabling stroke and a three-fold increased risk of cardiovascular mortality (1). The intense systemic inflammatory response associated with CABG has been implicated as an important mechanism of post-CABG AF (4,5). Statins or hydroxymethylglutaryl-CoA reductase inhibitors exert a pleiotropic or anti-inflammatory effect (6), which is thought to be associated with a reduction in the risk of post-CABG AF (7,8). Meta-analyses of randomized trials suggested that statin therapy reduces the risk of post-CABG AF (9,10). However, these randomized trials were limited by the small sample size, and the primary outcome of some of these studies was inflammatory markers, rather than post-CABG AF. These shortcomings have led to the recently published Statin Therapy In Cardiac Surgery (STICS) trial (11).
The STICS trial included 1,992 patients in normal sinus rhythm (not taking anti-arrhythmic agents at baseline, other than beta-blockers) scheduled to undergo elective CABG (87% of the patients), aortic valve surgery, or both. Subjects were randomized to rosuvastatin (n=960) versus placebo (n=962). Patients were recruited at a tertiary center in China. The study medication was initiated up to 8 days preoperatively (58% started the medication only 2 days or less), and continued for 5 days after surgery. The co-primary outcomes were postoperative AF, detected by continuous Holter monitoring for 5 days postoperatively, and perioperative myocardial injury (assessed by area-under-the-curve for Troponin I release). The risk of postoperative AF was similar in both groups: 203 patients (21%) in the rosuvastatin group versus 197 patients (20%) in the placebo group. In addition, rosuvastatin had no significant effect on Troponin I release (11).
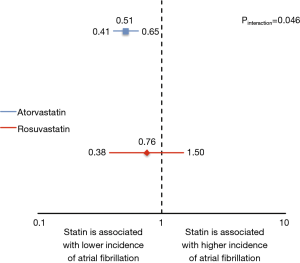
The STICS trial was a well-designed study and recruited a large number of patients, however; the findings of the STICS trial were inconsistent with the previous studies. What could explain this difference? First, the pleiotropic effect has been shown to vary among the individual statins; favoring the more lipophilic statins such as atorvastatin and simvastatin (12). By performing a meta-analysis of randomized trials including the STICS trials, we showed that atorvastatin was associated with 49% reduction in the risk of postoperative AF, but this effect was not observed with rosuvastatin (P for interaction =0.046) (Figure 1). A second consideration is the duration needed for statins to exert the maximum pleiotropic effect. Although statins, particularly atorvastatin, have been shown to exert a rapid anti-oxidant effect in patients undergoing elective CABG (13), studies have suggested that 14 days of statin therapy are usually required to achieve the full anti-inflammatory effect (14,15). This finding was supported by a meta-regression analysis, in which statins were associated with a 3% reduction in the risk of postoperative AF per day of therapy, which highlights the incremental benefit with earlier initiation of preoperative therapy (9). In the STICS trial, 58% of the patients were started on rosuvastatin only 2 days or less prior to the surgery and the maximum duration of therapy preoperatively was 8 days (11). This relatively short duration of preoperative treatment might have diminished the pleiotropic effects of statin therapy. Finally, genetic polymorphisms are known to affect the pharmacokinetics and pharmacodynamics of statins, resulting in inter-individual and inter-ethnic variability in the response to the drug (16). In the STICS trial, all patients were recruited from China, which might affect generalization of these results to other ethnicities.
An unexpected finding of the STICS trial was the higher incidence of acute kidney injury (AKI) with rosuvastatin, driven mainly by stage 1 AKI (11). The effect of perioperative statin therapy on renal function after cardiac surgery has been an area of debate. Earlier observational studies suggested a “renoprotective” effect for statins (17-19). These findings were disputed in a recent randomized trial, which showed no benefit with high dose atorvastatin on the risk of AKI after cardiac surgery (20). In fact, there was an increased risk of AKI in statin-naive patients with preexisting chronic kidney disease. In the STICS trial, almost two-thirds of the patients were statin-naive, which suggests a possibly higher risk of renal adverse events with de-novo initiation of therapy. Furthermore, some studies had suggested that East Asian subjects, as compared with Caucasians, have higher plasma exposure to rosuvastatin and its metabolites with the same dose, probably secondary to genetic polymorphism (21).
In summary, the STICS trial demonstrated no benefit for short-term perioperative rosuvastatin therapy in the prevention of postoperative AF in patients undergoing elective CABG, and a possible increased risk of AKI. The findings also support the hypothesis that early smaller studies could magnify the benefit of a treatment effect, which are oftentimes challenged by the results of large scale randomized trials (22). However, the results of the STICS trial may not be extrapolated to other statins (most importantly atorvastatin) if initiated earlier (i.e., ≥14 days prior to the surgery).
Acknowledgements
None.
Footnote
Provenance: This is an invited Editorial commissioned by the Section Editor Kai Zhu (Department of Cardiac Surgery, Zhongshan Hospital Fudan University, Shanghai, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mariscalco G, Klersy C, Zanobini M, et al. Atrial fibrillation after isolated coronary surgery affects late survival. Circulation 2008;118:1612-8. [Crossref] [PubMed]
- Mathew JP, Fontes ML, Tudor IC, et al. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA 2004;291:1720-9. [Crossref] [PubMed]
- Gillinov AM, Bagiella E, Moskowitz AJ, et al. Rate control versus rhythm control for atrial fibrillation after cardiac surgery. N Engl J Med 2016;374:1911-21. [Crossref] [PubMed]
- Hirai S. Systemic inflammatory response syndrome after cardiac surgery under cardiopulmonary bypass. Ann Thorac Cardiovasc Surg 2003;9:365-70. [PubMed]
- Aviles RJ, Martin DO, Apperson-Hansen C, et al. Inflammation as a risk factor for atrial fibrillation. Circulation 2003;108:3006-10. [Crossref] [PubMed]
- Barakat AF, Saad M, Abuzaid A, et al. Perioperative statin therapy for patients undergoing coronary artery bypass grafting. Ann Thorac Surg 2016;101:818-25. [Crossref] [PubMed]
- Patti G, Chello M, Candura D, et al. Randomized trial of atorvastatin for reduction of postoperative atrial fibrillation in patients undergoing cardiac surgery: results of the ARMYDA-3 (Atorvastatin for Reduction of MYocardial Dysrhythmia After cardiac surgery) study. Circulation 2006;114:1455-61. [Crossref] [PubMed]
- Ji Q, Mei Y, Wang X, et al. Effect of preoperative atorvastatin therapy on atrial fibrillation following off-pump coronary artery bypass grafting. Circ J 2009;73:2244-9. [Crossref] [PubMed]
- Chen WT, Krishnan GM, Sood N, et al. Effect of statins on atrial fibrillation after cardiac surgery: a duration- and dose-response meta-analysis. J Thorac Cardiovasc Surg 2010;140:364-72. [Crossref] [PubMed]
- Elgendy IY, Mahmoud A, Huo T, et al. Meta-analysis of 12 trials evaluating the effects of statins on decreasing atrial fibrillation after coronary artery bypass grafting. Am J Cardiol 2015;115:1523-8. [Crossref] [PubMed]
- Zheng Z, Jayaram R, Jiang L, et al. Perioperative rosuvastatin in cardiac surgery. N Engl J Med 2016;374:1744-53. [Crossref] [PubMed]
- Turner NA, Midgley L, O'Regan DJ, et al. Comparison of the efficacies of five different statins on inhibition of human saphenous vein smooth muscle cell proliferation and invasion. J Cardiovasc Pharmacol 2007;50:458-61. [Crossref] [PubMed]
- Antoniades C, Bakogiannis C, Leeson P, et al. Rapid, direct effects of statin treatment on arterial redox state and nitric oxide bioavailability in human atherosclerosis via tetrahydrobiopterin-mediated endothelial nitric oxide synthase coupling. Circulation 2011;124:335-45. [Crossref] [PubMed]
- Albert MA, Danielson E, Rifai N, et al. Effect of statin therapy on C-reactive protein levels: the pravastatin inflammation/CRP evaluation (PRINCE): a randomized trial and cohort study. JAMA 2001;286:64-70. [Crossref] [PubMed]
- Plenge JK, Hernandez TL, Weil KM, et al. Simvastatin lowers C-reactive protein within 14 days: an effect independent of low-density lipoprotein cholesterol reduction. Circulation 2002;106:1447-52. [Crossref] [PubMed]
- Ieiri I, Higuchi S, Sugiyama Y. Genetic polymorphisms of uptake (OATP1B1, 1B3) and efflux (MRP2, BCRP) transporters: implications for inter-individual differences in the pharmacokinetics and pharmacodynamics of statins and other clinically relevant drugs. Expert Opin Drug Metab Toxicol 2009;5:703-29. [Crossref] [PubMed]
- Tabata M, Khalpey Z, Pirundini PA, et al. Renoprotective effect of preoperative statins in coronary artery bypass grafting. Am J Cardiol 2007;100:442-4. [Crossref] [PubMed]
- Layton JB, Kshirsagar AV, Simpson RJ Jr, et al. Effect of statin use on acute kidney injury risk following coronary artery bypass grafting. Am J Cardiol 2013;111:823-8. [Crossref] [PubMed]
- Huffmyer JL, Mauermann WJ, Thiele RH, et al. Preoperative statin administration is associated with lower mortality and decreased need for postoperative hemodialysis in patients undergoing coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth 2009;23:468-73. [Crossref] [PubMed]
- Billings FT 4th, Hendricks PA, Schildcrout JS, et al. High-dose perioperative atorvastatin and acute kidney injury following cardiac surgery: A Randomized Clinical Trial. JAMA 2016;315:877-88. [Crossref] [PubMed]
- Birmingham BK, Bujac SR, Elsby R, et al. Rosuvastatin pharmacokinetics and pharmacogenetics in Caucasian and Asian subjects residing in the United States. Eur J Clin Pharmacol 2015;71:329-40. [Crossref] [PubMed]
- Elgendy IY, Huo T, Bhatt DL, et al. Is Aspiration thrombectomy beneficial in patients undergoing primary percutaneous coronary intervention? Meta-analysis of randomized trials. Circ Cardiovasc Interv 2015;8:e002258. [Crossref] [PubMed]


