Concomitant off-pump coronary artery bypass and non-cardiovascular surgery
Introduction
Due to an aging patient population, the number of patients with both cardiac and non-cardiovascular surgical diseases is increasing (1). Non-cardiovascular surgical disease can be found during preoperative evaluation of a patient who is to undergo coronary artery bypass grafting (CABG), or significant coronary artery disease requiring revascularization can be found during preoperative evaluation of a patient who is to undergo non-cardiovascular surgery. One previous study demonstrated that prior successful CABG was protective by significantly lowering the perioperative cardiac complication rate among patients who underwent high-risk noncardiac surgery (2). However, the exact timing of CABG and composition of an appropriate patient population remained undefined. In addition, the staged procedures were associated with higher cost, delay in surgery for non-cardiovascular malignant disease, and longer hospital stays (3). Although concomitant operations avoid the need for a second operation and reduce the overall hospital stay and cost, surgeons are reluctant to perform concomitant cardiac and non-cardiovascular operations because of concerns about systemic heparin administration and exposure of two different operative fields (4).
Recent treatment guidelines for cardiac patients who also have non-cardiac vascular disease such as carotid or peripheral arterial disease have evaluated and summarized all available evidence (5); however, the surgical treatment strategy of concomitant cardiac and non-cardiovascular surgical disease remains controversial. The aims of the present study were: (I) to assess the operative mortality and postoperative morbidities of concomitant OPCAB and non-cardiovascular surgeries; (II) to compare the results of concomitant OPCAB and non-cardiovascular surgeries with those of isolated OPCAB.
Methods
The study protocol was reviewed by the Institutional Review Board and approved as a minimal risk retrospective study (approval number: H-1511-096-721) that did not require individual consent based on the institutional guidelines for waiving consent.
Patient characteristics
A total of 2,604 patients underwent isolated CABG between January 1999 and December 2014 at our institution, and OPCAB was performed in 2,439 patients (93.7%). Of the 2,439 OPCAB patients, 115 underwent concomitant OPCAB and non-cardiovascular surgery (group 1) and 2,251 underwent isolated OPCAB (group 2) and were included in the study. Informed written consent, including the possible benefits and risks of concomitant OPCAB and non-cardiovascular surgery, was obtained from all patients.
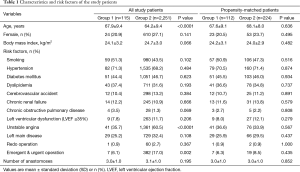
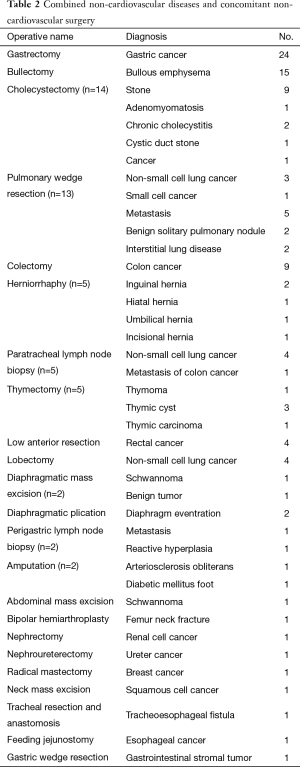
The remaining 73 patients who underwent concomitant OPCAB and non-cardiac vascular surgery, such as carotid endarterectomy, peripheral arterial bypass and abdominal aortic replacement, were excluded from the study because recent guidelines for such patients have already evaluated and summarized all available evidence (5). Preoperative patient characteristics revealed that group 1 patients were significantly older (67.9±9.4 vs. 64.2±9.4 years, P<0.0001), had less unstable angina (35.7% vs. 60.5%, P<0.0001) and required less emergent or urgent operation (6.1% vs. 17.0%, P=0.002) than group 2 patients. A propensity score model was constructed to adjust differences in preoperative characteristics and intraoperative data between the two groups, and 112 patients in group 1 and 224 patients in group 2 were extracted by 1:2 matching. There were no differences in demographic data and preoperative risk factors between the two propensity score-matched groups (Table 1). Combined non-cardiovascular diseases included 63 malignant (24 stomach cancers, 18 lung cancers, 13 colorectal cancers, and 8 other cancers), and 52 benign (15 pulmonary bullous emphysemas, 13 benign gallbladder diseases, 5 hernias, and 19 other benign conditions) diseases. Concomitant non-cardiovascular surgeries performed were general (n=62; 24 gastrectomies, 14 cholecystectomies, 13 colorectal resections, and 11 other general surgeries), thoracic (n=47; 15 bullectomies, 13 wedge resections, 5 thymectomies, 4 lobectomies, and 10 other thoracic surgeries), orthopedic (n=3), urologic (n=2), and otolaryngologic surgeries (n=1) (Table 2).
Full table
Full table
Operative technique
The basic surgical procedures and strategies of OPCAB have been previously described (6,7). During the study period, we changed revascularization strategies based on our patency study after OPCAB (6); however, the left internal thoracic artery has continuously been used as the first conduit of choice for CABG. Patients were given an initial dose of heparin (1.5 mg/kg) and periodic supplemental doses to maintain an activated clotting time of >300 seconds. Protamine was given to neutralize the effect of heparin at the end of OPCAB procedures. Group 1 patients stopped taking aspirin 5 days before the operation at the request of the non-cardiovascular surgeon; however, most of group 2 patients took aspirin until the day of surgery. All patients resumed aspirin as soon as possible after surgery. Therefore, patients stopped aspirin for a short perioperative period.
After myocardial revascularization and full neutralization of heparin to ensure a relatively dry field, a concomitant non-cardiovascular surgery was performed by a non-cardiovascular surgeon of each subspecialty in all group 1 patients. Thoracic surgeries such as lobectomy and pulmonary wedge resection were performed via the median sternotomy approach after OPCAB. General surgeries such as gastrectomy and cholecystectomy were performed by extension of the skin incision to the upper abdomen after closure of the sternum. Other non-cardiovascular surgeries were performed via a separate skin incision after closure of the median sternotomy wound.
Statistical analysis
Statistical analysis was performed with the SPSS (version 22; SPSS Inc., Chicago, IL, USA) and SAS (version 9.2; SAS Institute, Cary, NC, USA) statistical software packages. Data were expressed as mean ± standard deviation (SD), or proportions, and a P value of less than 0.05 was considered as statistically significant.
A propensity score matching analysis was performed to adjust differences in preoperative and intraoperative factors. A propensity score model was constructed by including 16 preoperative and intraoperative variables (P value for Hosmer Lemeshow test =0.6406, and c statistic =0.761). These variables were 15 preoperative factors such as sex, age, body mass index, smoking, hypertension, diabetes mellitus, dyslipidemia, history of stroke, chronic renal failure, chronic obstructive pulmonary disease, left ventricular dysfunction, unstable angina, left main coronary artery disease, redo operation, and urgent or emergent operation; and 1 operative factor (number of distal anastomoses). Because there was a large difference in the number of patients between the two groups, 112 patients in group 1 and 224 patients in group 2 were extracted by 1:2 matching. Comparison between the two groups was performed using the χ2 test or Fisher exact test for categorical variables and the Student t-test or Wilcoxon rank sum test for continuous variables.
Results
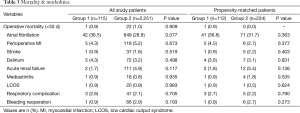
The average number of distal anastomoses per patient was similar between the two groups (3.0±1.0 vs. 3.1±1.0, P=0.195). Operative mortalities (any death within 30 days, including deaths after hospital discharge) were 0.9% (1 of 115) in group 1 and 1.0% (22 of 2,251) in group 2 (P=0.909). Operative mortality in group 1 developed in an 81-year-old male with advanced stomach cancer who died of pneumonia on postoperative day 26. There were no significant differences in the incidence of postoperative morbidities including atrial fibrillation (36.5% vs. 28.8%, P=0.077), perioperative myocardial infarction (MI) (4.3% vs. 5.2%, P=0.673), acute renal failure (1.7% vs. 4.9%, P=0.177), mediastinitis (0.9% vs. 0.8%, P=0.935), bleeding reoperation (0.9% vs. 2.9%, P=0.193), and respiratory complications (2.6% vs. 2.1%, P=0.705) between the two groups. After 1:2 propensity scoring, there were no significant differences in the postoperative morbidities between the two groups (Table 3).
Full table
Discussion
The present study demonstrated that concomitant OPCAB and non-cardiovascular surgery did not increase operative mortality and perioperative morbidities when compared with isolated OPCAB, and suggested that the need for second operation would be avoided by performing a combined procedure.
The combination of coronary artery and non-cardiovascular surgical diseases is not uncommon and is expected to increase due to an increasing elderly population. However, the optimal strategy for a patient who has combined cardiac and non-cardiovascular surgical diseases remains controversial. Surgical treatment can be performed separately by 2-stage operations or simultaneously by a concomitant operation. The 2-stage procedure, prior successful CABG followed by non-cardiovascular surgery, has been demonstrated to reduce mortality and morbidities; however, this technique was associated with higher cost, delay in surgery for malignant disease, and longer hospital stay (2,3,8). An unpredictable delay between the two procedures could be detrimental in cases of malignancy. Surgical management of combined surgical diseases at the same time is an ideal approach by virtue of avoiding the need for a second operation.
Previous studies demonstrated that concomitant operations avoided the need for a second operation and reduced the overall hospital stay and cost (4,9). However, concomitant cardiac surgery using cardiopulmonary bypass had a substantial risk of postoperative bleeding due to the inevitable coagulopathy and platelet dysfunction seen when using cardio pulmonary bypass (4).
In addition, use of cardiopulmonary bypass for cardiac surgery has been shown to have a possible detrimental effect on both cellular and humoral immunity, thereby causing immunosuppression, dissemination, or progression of malignant disease (9-13). In addition, cardiac surgery using cardiopulmonary bypass generally causes systemic tissue edema, which may increase the risk of failure of gastrointestinal tract anastomoses (13). A recent trend has been the use of off-pump CABG to avoid the effect of cardiopulmonary bypass and decrease the use of heparin (10,14,15). The off-pump technique could markedly lower the risk of the disadvantages related to use of cardiopulmonary bypass, although other studies found no advantage of using an off-pump technique compared with cardiac surgery using cardiopulmonary bypass (3,13-15).
The present study demonstrated that concomitant OPCAB and non-cardiovascular surgery compared with those of isolated OPCAB did not increase operative mortality and perioperative morbidities, although the majority of patients had concomitant malignant disease and underwent laparotomy (63 patients had combined malignant diseases; 62 patients underwent general surgeries opening the abdominal cavity). In addition, gastrointestinal surgery also carries a risk of bacterial contamination during concomitant cardiac surgery. In the present study, one diabetic patient who received bilateral internal thoracic artery grafts developed mediastinitis in group 1. Incidence of mediastinitis was not higher in group 1 compared with group 2.
There are limitations to the present study that must be recognized. First, the present study was a retrospective observational study in a single institution, although 1:2 propensity score-matched analysis was performed to overcome the limitation of difference in baseline patient characteristics. Second, the results of concomitant OPCAB surgery were not compared with those of concomitant on-pump CABG surgery, because almost all CABG procedures at our institution were performed using OPCAB during the study period. Third, the results of concomitant OPCAB surgery were not also compared with those of the 2-stage operations, because almost all surgical management of combined surgical diseases at our institution were performed using concomitant OPCAB during the study period. Fourth, mid-term or long-term follow up results were not included in the present study. It will be necessary to extend the follow-up and to demonstrate more completely the advantages of concomitant OPCAB and non-cardiovascular surgery, particularly in patients with malignancies.
Acknowledgements
We wish to thank the Medical Research Collaborating Center, Seoul National University Hospital, for providing statistical consultation services.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol was reviewed by the Institutional Review Board and approved as a minimal risk retrospective study (approval number: H-1511-096-721) that did not require individual consent based on the institutional guidelines for waiving consent.
References
- Fleisher LA, Eagle KA. Clinical practice. Lowering cardiac risk in noncardiac surgery. N Engl J Med 2001;345:1677-82. [Crossref] [PubMed]
- Eagle KA, Rihal CS, Mickel MC, et al. Cardiac risk of noncardiac surgery: influence of coronary disease and type of surgery in 3368 operations. CASS Investigators and University of Michigan Heart Care Program. Coronary Artery Surgery Study. Circulation 1997;96:1882-7. [Crossref] [PubMed]
- Darwazah AK, Osman M, Sharabati B. Use of off-pump coronary artery bypass surgery among patients with malignant disease. J Card Surg 2010;25:1-4. [Crossref] [PubMed]
- Rao V, Todd TR, Weisel RD, et al. Results of combined pulmonary resection and cardiac operation. Ann Thorac Surg 1996;62:342-6; discussion 346-7. [Crossref] [PubMed]
- Kolh P, Windecker S, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg 2014;46:517-92. [Crossref] [PubMed]
- Kim KB, Kim JS, Kang HJ, et al. Ten-year experience with off-pump coronary artery bypass grafting: lessons learned from early postoperative angiography. J Thorac Cardiovasc Surg 2010;139:256-62. [Crossref] [PubMed]
- Hwang HY, Kim JS, Oh SJ, et al. A randomized comparison of the Saphenous Vein Versus Right Internal Thoracic Artery as a Y-Composite Graft (SAVE RITA) trial: early results. J Thorac Cardiovasc Surg 2012;144:1027-33. [Crossref] [PubMed]
- Zhang H, Wang DX, Xiao F, et al. The impact of previous or concomitant myocardium revascularization on the outcomes of patients undergoing major non-cardiac surgery. Interact Cardiovasc Thorac Surg 2009;9:788-92. [Crossref] [PubMed]
- Danton MH, Anikin VA, McManus KG, et al. Simultaneous cardiac surgery with pulmonary resection: presentation of series and review of literature. Eur J Cardiothorac Surg 1998;13:667-72. [Crossref] [PubMed]
- Darwazah AK. Surgical management of coronary artery disease associated with malignancy. J Card Surg 2012;27:581-8. [Crossref] [PubMed]
- Akbas H, Erdal AC, Demiralp E, et al. Effects of coronary artery bypass grafting on cellular immunity with or without cardiopulmonary bypass: changes in lymphocytes subsets. Cardiovasc Surg 2002;10:586-9. [Crossref] [PubMed]
- Mayumi H, Zhang QW, Nakashima A, et al. Synergistic immunosuppression caused by high-dose methylprednisolone and cardiopulmonary bypass. Ann Thorac Surg 1997;63:129-37. [Crossref] [PubMed]
- Suzuki S, Usui A, Yoshida K, et al. Effect of cardiopulmonary bypass on cancer prognosis. Asian Cardiovasc Thorac Ann 2010;18:536-40. [Crossref] [PubMed]
- Dyszkiewicz W, Jemielity M, Piwkowski C, et al. The early and late results of combined off-pump coronary artery bypass grafting and pulmonary resection in patients with concomitant lung cancer and unstable coronary heart disease. Eur J Cardiothorac Surg 2008;34:531-5. [Crossref] [PubMed]
- Schoenmakers MC, van Boven WJ, van den Bosch J, et al. Comparison of on-pump or off-pump coronary artery revascularization with lung resection. Ann Thorac Surg 2007;84:504-9. [Crossref] [PubMed]


