Management of an intrapleural foreign body and empyema with video-assisted thoracoscopy
Introduction
Intrathoracic foreign bodies are infrequent but are usually present secondary to penetrating trauma injuries and foreign body aspiration. Most intrathoracic foreign bodies present in the bronchi, lung, or esophagus, and there are few reports of intracardiac or intrapleural foreign bodies. Intrapleural foreign bodies are comparatively rare, and there are few cases documented in the literature. Previous studies indicate the etiology is most commonly secondary to iatrogenic injury or traumatic event (1). We present a case of a 33-year-old male requiring surgical management of an intrapleural foreign body and an associated empyema.
Case representation
A 33-year-old male with a history of foreign body ingestion and numerous laparotomy procedures, presented with left upper quadrant abdominal pain after confirmed foreign body ingestion. Four days prior to presentation, he complained of worsening abdominal pain which he described as episodic, sharp and progressively intense and frequent. He endorsed fever, chills, nausea, bloody emesis and his physical examination was remarkable for abdominal rebound tenderness and involuntary guarding. He was febrile and had a leukocytosis. The abdominal CT of the abdomen with contrast demonstrated evidence of multiple foreign bodies in the stomach (Figure 1). He was taken emergently to the operating room, where he underwent an exploratory laparotomy, gastrotomy with retrieval of foreign bodies. Upon entering the stomach, multiple foreign bodies (pencils, plastic spoons, and ballpoint pens) were discovered and safely removed. Upon further inspection, there was evidence of a foreign body that migrated through the posterior gastric wall into the lesser sac; however, this item was not safely retrievable given the extensive adhesions from previous operations and the risk of significant injury to the stomach.

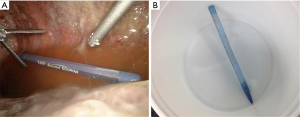
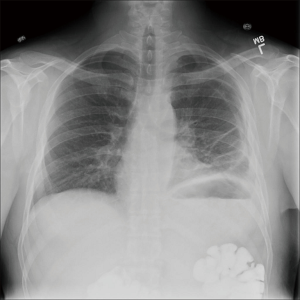
On post-operative day 8, he complained of left-sided pleuritic chest pain that radiated to the diaphragm. He was febrile and developed tachycardia. His physical exam was remarkable for decreased breath sounds in the left lung field. The white blood cell count was elevated to 21,000. A chest X-ray demonstrated a large left pleural effusion (Figure 2A). A CT scan of the thorax demonstrated the presence of a writing pen located in left apex of the pleural cavity, a large left pleural effusion and a small pneumothorax (Figure 2B,C). We recommended surgical intervention given these findings. He was taken to the operating room where he underwent an esophagogastroduodenoscopy (EGD), left video-assisted thoracoscopic surgery (VATS), pulmonary decortication with removal of the intrapleural foreign body.

The EGD revealed no evidence of an esophageal or gastric perforation. During the VATS procedure, there was a writing pen visualized in the left apex of the pleural cavity (Figure 3A,B). The ballpoint pen was covered in adhesions in the setting of multi-loculated pockets of pleural fluid consistent with a fibropurulent empyema. The adhesions were disrupted and all of the pleural fluid was suctioned. The pen was removed and the left surface of the diaphragm was inspected and there was no evidence of perforation or inflammation. The patient had no major intraoperative complications. He recovered well and had no post-operative complications. His postoperative chest X-ray demonstrated resolution of the left pleural effusion (Figure 4).
Comments
Foreign bodies located in the pleural cavity are exceedingly rare. The incidence of intrapleural foreign bodies remained unknown, given the limited documentation in the literature. Intrapleural foreign bodies can be categorized as those entering the pleural space as a result of inhalation or passing through the chest wall from the exterior (1). There are few case reports that describe patients with intrapleural foreign bodies secondary to iatrogenic causes (chest tube placement, therapeutic pneumothorax, zinc oxide treatment, and surgical sponges) (1-4). Most intrathoracic foreign bodies can be detected radiographically and treated with surgical removal. Complications of retained intrapleural foreign bodies may include pneumonia, lung abscess, pulmonary gangrene, and empyema.
In our case, the patient had an extensive psychiatric history and history of foreign body ingestion. He presented initially to the acute care surgery service with an acute ingestion of multiple foreign bodies, which included utensils and a ballpoint pen. Given the concern for enteric perforation and peritonitis, he was taken to the operating room for foreign body removal by the acute care surgery service. Post-operatively, he developed a left-sided pleural effusion and empyema secondary to the intrapleural foreign body. The left diaphragm was observed to be intact intraoperatively and there were no signs of a perforation of the esophagus or the stomach. The mechanism by which the writing pen migrated from the lesser sac to the apex of the left pleural cavity remains unknown. There was no objective evidence on imaging or endoscopy that the patient sustained an esophageal perforation.
The migration of foreign bodies from the abdomen to the pleural space is extremely rare. Most cases of ingested foreign bodies can result in esophageal injury requiring repair and mediastinal drainage (2). This case is particularly unique because the patient’s ingested foreign body migrated from the stomach into the lesser sac and into the left pleural cavity without any evidence of diaphragmatic or esophageal injury. Surprisingly, that migration did not lead to pericardial, esophageal, gastric or intravascular injury. One possible mechanism may include migration of the foreign body through the esophageal hiatus.
In conclusion, an ingested foreign body infrequently migrates from the gastrointestinal tract to the pleural space. Complications such as gastrointestinal, vascular and pulmonary injury should be considered and close follow up is advocated. Safe removal of retained intrapleural foreign objects should be considered in order to minimize the risk of prospective complication.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: A waiver for consent was obtained from the IRB committee.
References
- Ireland J. Intrapleural foreign bodies. Am J Surg 1940;49:356-8. [Crossref]
- Leroux BT. Intrathoracic foreign bodies. Thorax 1964;19:203-17. [Crossref] [PubMed]
- Willauer G, Chodoff RJ. Removal of intrapleural foreign body under thoracoscopic guidance: Case report. Am J Surg 1942;55:606. [Crossref]
- Trombold JS, McCuistion AC, Harris HW. Slowly expanding intrapleural lesion due to a foreign body. Report of a case. N Engl J Med 1961;264:172-4. [Crossref] [PubMed]


