Non-intubated laparoscopic repair of giant Morgagni’s hernia for a young man
Introduction
Morgagni’s hernia (MH) caused by a congenital defect in the sternal aspect of the diaphragm is one kind of the diaphragmatic hernias, which is rare and involves a defect just behind the sternum, also known as retrosternal hernia, parasternal hernia and anterolateral hernia. Laparoscopic repair of MH was traditionally performed via general anesthesia. Here, a patient with MH was presented, and he underwent laparoscopic hernia repair under regional anesthesia with minimal anesthesia-related complications and encouragingly fast recovery.
Case presentation
A 22-year-old man without any complaints was admitted to department of thoracic surgery because his chest radiograph indicated a giant mediastinal lipoma-like density in the right cardiophrenic angle during premarital examination (Figure 1A). Apart from overweight with body mass index of 27.0, his physical examination was normal. Then axial and sagittal reconstruction CT demonstrated a large incarcerated MH, characterized by a defect in the right anterior diaphragm with herniation of the omentum into the thorax, nearly 16 cm at the widest point (Figure 1B,C). He denied blunt trauma and other risk factors for acquired diaphragmatic hernia.
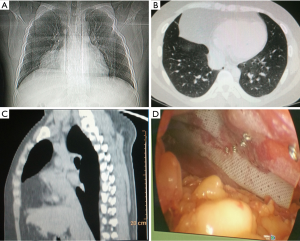
Instead of general anesthesia, regional anesthesia was chosen for cost saving after preoperative discussion by anesthetists and surgeons as the coagulant activity of the patient was normal, therefore, the hernia was reduced using a laparoscopic procedure under epidural anesthesia without endotracheal intubation, and a laryngeal mask was used for inhalation of oxygen, combined with continued sedation by infusion of remifentanil under spontaneous respiration. The patient was placed in a supine position and close CO2 pneumoperitoneum with 15 mmHg of intra-abdominal pressure was performed. One 10 mm trocar below the umbilicus was inserted for laparoscopic exploration, and two additional trocars were placed for manipulation respectively. A diaphragmatic defect measuring about 7 cm × 5 cm in size was located just posterolateral to the sternum on right side of the xiphoid and anterior to the right lobe of liver, which was consistent with MH. The hernia content of omentum was gently repositioned back into abdominal cavity by grasping forceps, and the diaphragmatic defect was repaired with composite mesh to achieve a tension-free repair successfully without resection of the hernia sac (Figure 1D).
The hemodynamic index including PaO2, PaCO2, blood pressure and central venous pressure were stable throughout the surgery, and the operative time was 75 min. Besides, the patient started oral diet and returned to normal activities 6 hours after the operation without cough, palpitation, dyspnea, nausea or vomiting, however, the patient felt thirsty, mild chest stuffy and abdominal distension after sedation for nearly 12 hours, which was alleviated after defecate, and the abdominal drainage tube was removed on the following day. Recovery was mainly uneventful, and postoperative right pleural effusion was indicated 2 days later, and he was discharged after chest drainage while a chest radiograph confirmed the closure of MH. Then he was followed up remotely via internet-based approaches for life-style and psychological consultation persistently for 2 months without hernia recurrence.
Discussion
MH accounted for only 1–2% of all congenital diaphragmatic hernia (1). The MH sac is most commonly on the right side and can contain small bowel, transverse colon, omentum, and rarely stomach or liver, furthermore, sustained or sudden severe increased intra-abdominal pressure, trauma or pregnancy could lead to the acute onset of MH, thus, if patients present with prolonged shortness of breath, or a right cardiophrenic angle lesion on chest radiograph, the diagnosis of a diaphragmatic hernia should be considered (2). Axial and sagittal CT scan could indicate anatomical details of MH contents and possible complications such as bowel obstruction or strangulation.
It was reported that mesh repair for MH could be performed via laparotomy, thoracotomy and thoraco-abdominal approach, but mesh insertion was not always necessary for diaphragmatic hernia (3,4). On the contrary, a retrospective review indicated that MH recurrence was high after laparoscopic repair in patients without patch, and more frequent use of patch may be beneficial (5). Besides, the percutaneous suturing technique and single-site umbilical laparoscopic repair of MH was an easy alternative to normal laparoscopic surgery (1). Furthermore, laparoscopic transabdominal preperitoneal approach was reported as an excellent alternative for inguinal hernia repair (6), which could be also considered for diaphragmatic hernia, as controversy persists about the optimal procedure. In addition, laparoscopic repair should be the first choice for MH, which is suitable for sac exploration and hernia repair (7). Meanwhile, laparoscopic approach for MH indicated general benefits of minimally invasive surgery, including less postoperative pain, decreased complications and hospital stay (4), which is also simple and safe for elderly patients (8). Moreover, laparoscopic repair of MH could be even performed in an outpatient setting with excellent outcome (9). Additionally, hernia sac excision is not necessary (3), and the disadvantages of sac excision may include massive pneumomediastinum and potential injury to the lung, pericardium, or mediastinal structures (10).
On the other hand, laparoscopic procedures have been traditionally performed under general anesthesia due to the respiratory changes caused by pneumoperitoneum, and hernia repair of MH could be safely performed via general anesthesia (7). Up to date, regional anesthesia has emerged as an alternative choice for laparoscopy, which theoretically includes several advantages, such as prevention of airway manipulation, awake and spontaneous breathing, minimal nausea and vomiting, effective post-operative analgesia and early recovery. The non-intubated procedures try to minimize the adverse effects of tracheal intubation and general anesthesia, such as intubation-related airway trauma, ventilation-induced lung injury, residual neuromuscular blockade, and postoperative nausea and vomiting (11). However, it may be associated with certain side effects such as the requirement of a higher sensory level, more severe hypotension, discomfort due to diaphragmatic irritation, and respiratory embarrassment caused by pneumoperitoneum (12), meanwhile, gaseous distension of the abdomen may compromise the ventilation of the patients during the surgery. Encouragingly, reports of non-intubated thoracoscopic approach had suggested the optimal feasibility for wedge resection, lung volume reduction surgery, resection of lung cancer, bronchial sleeve resection and even carina reconstruction, especially for patients with significant risks for intubated general anesthesia (13-15). And for old patients with severely compromised lung function or tracheal deformity, non-intubated procedure could be considered as an alternative if mesh repair is necessary.
It is noteworthy that patients with MH can be asymptomatic or present with vague gastrointestinal or respiratory symptoms, and a misdiagnosis can lead to obstruction or strangulation presented as gastric outlet obstruction, peritonitis from infarcted contents or acute respiratory distress, which warrants early surgical intervention (2).
In conclusion, this case indicated the potential feasibility and safety of non-intubated laparoscopic mesh repair of giant MH via epidural anesthesia combined with sedation, however, more studies are required for the widespread application of this procedure.
Acknowledgements
Funding: This study was supported by Speciality Fund for Jiangsu Key Laboratory of Molecular and Translational Cancer Research (No. BM2013007).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Zouari M, Jallouli M, Bendhaou M, et al. Percutaneous suturing technique and single-site umbilical laparoscopic repair of a Morgagni hernia: Review of three cases. Arch Pediatr 2015;22:1272-5. [Crossref] [PubMed]
- Humble AG, Sample CB. Morgagni's hernia in a hypoxaemic adult. Lancet 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Aghajanzadeh M, Khadem S, Khajeh Jahromi S, et al. Clinical presentation and operative repair of Morgagni hernia. Interact Cardiovasc Thorac Surg 2012;15:608-11. [Crossref] [PubMed]
- Park A, Doyle C. Laparoscopic Morgagni hernia repair: how I do it. J Gastrointest Surg 2014;18:1858-62. [Crossref] [PubMed]
- Garriboli M, Bishay M, Kiely EM, et al. Recurrence rate of Morgagni diaphragmatic hernia following laparoscopic repair. Pediatr Surg Int 2013;29:185-9. [Crossref] [PubMed]
- Pironi D, Palazzini G, Panarese A, et al. Open mesh technique versus laparoscopic transabdominal preperitoneal (TAPP) approach in inguinal hernia repair. Our experience. G Chir 2008;29:497-504. [PubMed]
- Li S, Liu X, Shen Y, et al. Laparoscopic repair of Morgagni hernia by artificial pericardium patch in an adult obese patient. J Thorac Dis 2015;7:754-7. [PubMed]
- Ikarashi M, Matsuda M, Murayama I, et al. Laparoscopic repair of Morgagni hernia with composite mesh in an elderly woman: Report of a case. Asian J Endosc Surg 2015;8:216-8. [Crossref] [PubMed]
- Yamaguchi S, Marshall MB. Outpatient laparoscopic repair of a Morgagni hernia. Surg Innov 2013;20:NP38-9. [Crossref] [PubMed]
- Shields TW, LoCicero J, Reed CE, et al. editors. General Thoracic Surgery. 7th ed. Philadelphia: Lippincott Williams & Wilkins, 2009.
- Gonzalez-Rivas D, Bonome C, Fieira E, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721-31. [Crossref] [PubMed]
- Bajwa SJ, Kulshrestha A. Anaesthesia for laparoscopic surgery: General vs regional anaesthesia. J Minim Access Surg 2016;12:4-9. [Crossref] [PubMed]
- Pompeo E. State of the art and perspectives in non-intubated thoracic surgery. Ann Transl Med 2014;2:106. [PubMed]
- Wang W, Peng G, Guo Z, et al. Radical resection of right upper lung cancer using uniportal video-assisted thoracic surgery with non-intubated anesthesia. J Thorac Dis 2015;7:2362-5. [PubMed]
- Peng G, Cui F, Ang KL, et al. Non-intubated combined with video-assisted thoracoscopic in carinal reconstruction. J Thorac Dis 2016;8:586-93. [Crossref] [PubMed]


